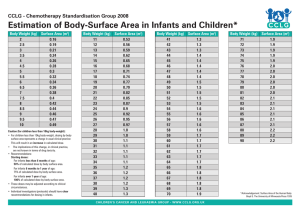
650 Pharmacology Exam 4 Study Guide (all MC, need calculator and blank paper) ADME (absorption, distribution, metabolism, elimination) Absorption o Gastrointestinal Tract – 2 factors affect the absorption of drugs pH-dependent passive diffusion Gastric emptying time The net effect of these factors on drug absorption is impossible to predict; phenobarbital has been reported to be absorbed rapidly, whereas diazepam absorption may be delayed o Intramuscular Sites – Altered in premature infants (Rare use except in emergencies r when an IV site is inaccessible Differences in relative muscle mass Poor perfusion to various muscles Insufficient muscular contractions o Skin – Percutaneous absorption increased substantially in newborns Skin – underedeveloped epidermal barrier (stratum corneum) and increased skin hydration-the relative systemic exposure of topically applied drugs, including corticosteroids, may be higher in infants and young children than in adults. The increased exposure can produce toxic effects after topical use of hexachlorophene soaps and powders,12 salicylic acid ointment, and rubbing alcohol. o Total body surface area (BSA) to total body weight is highest in the young Distribution o Drug distribution in the neonate depends on Amount of body water, body fat and drug binding o Body Water (BW) Neonates(70%) have more BW than adults (50 - 60%) Full-term: 70 - 78% body weight is water Pre-term: 85%: body weight is water o Body Fat Pre-term infants have much less fat than full-term therefore lipid soluble drugs may not accumulate o Drug Binding to plasma proteins Binding of drugs to albumin is reduced Drug competition for binding albumin may occur o Distribution – Determined by physiochemical properties of drugs which are constant, though physiologic functions often vary in patient populations Gentamicin distribution volume = 0.48 L/Kg in neonates and 0.20 L/Kg in adults. Tobramycin distribution volume is largest in the most premature infants o Decreased binding of drugs to plasma proteins in newborns Many drugs including phenobarbital, salicylates, and phenytoin have significantly less plasma protein binding in neonates than adults Increase apparent volume of distribution (Vd) o Increased concentrations of free or unbound drug in the serum and tissues Pharmacologic and toxic effects directly related to the free drug concentration o Substantially lower body fat in neonates than adults Highly lipid-soluble drugs are distributed less widely in infants than adults Diazepam’s Vd has ranged from 1.4 to 1.8 L/kg In neonates and from 2,2 to 2.6 L/kg in adults Certain drugs distributed in breast milk may be problematic for infants o Increase Vd – Premature infants require a larger loading dose than older children and adults to achieve a therapeutic serum concentration of drugs such as phenobarbital19 and phenytoin. Metabolism o Drug metabolism is substantially slower in infants than in older children or adults Important differences in the maturation of metabolism pathways in a premature infant Sulfation pathway is well developed, Glucoronidation pathway is underdeveloped Acetaminophen metabolism by glucoronidation is impaired in infants but balanced by the sulfation pathway. Chloramphenicol-induced gray baby syndrome in newborns is due to the decreased metabolism Infants require higher serum concentrations of morphine to achieve efficacy in premature infants versus adults Metabolism by oxidation is also impaired in newborns – (Phenobarbital, Phenytoin, Theophylline) More rapid metabolism with phenobarbital and phenytoin than with theophylline Involves the cytochrome P450 (CYP) isozymes Because of decreased metabolism, daily doses of these drugs + diazepam should be decreased in premature infants. o Two additional observations about theophylline metabolism by CYP1A2 in pediatric patients should be noted. First, in premature infants receiving theophylline for treatment of apnea, a significant amount of its active metabolite caffeine may be present, unlike the case in older children and adults. Second, theophylline clearance in children 1 to 9 years of age exceeds the values in infants as well as adults. Thus, a child with asthma often requires markedly higher doses on a weight basis of theophylline compared with an adult. Because of decreased metabolism, daily doses of drugs such as theophylline, phenobarbital, phenytoin, and diazepam should be decreased in premature infants. Elimination o Drugs and their metabolites are often eliminated by the kidney o Low glomerular filtration rates (GFR) in preterm and term infants (GFR is much lower in newborns than in older infants) o GFR, tubular secretion and tubular reabsorption determine the efficiency of renal secretion (These processes may not develop fully for several weeks to 1 year after birth Tobramycin clearance during the first postnatal week may increase with an increase in gestational age Postnatal age also correlates directly with aminoglycoside clearance in infants up to 1 month after birth Premature infants require a lower daily dose of drugs eliminated by the kidney during the first week of life; the dosage requirement increases with age o Toddlers have a shorter drug elimination half-life (t1/2) than older children and adults probably due to increased renal elimination and metabolism o Dose-related toxicity may result from an underdeveloped gluronidation pathway Dosing of obese children Weight-based dosing of medications for obese children may result in suboptimal drug therapy Obese children have a higher proportion of body fat, which generally results in a higher Volume of distribution (Vd) for lipophilic drugs and lower Vd for hydrophilic medications compared with normal-weight children Obese children have higher total body water, lower percent lean mass, increased organ mass and greater cardiac output, GFR, and serum creatinine concentrations than normal-weight children Vancomycin distributes into total body water and other tissues and is eliminated primarily by glomerular filtration. Obese children have been found to have an increased time to reach therapeutic INR with warfarin dosing Giving injections: sites in infants (IM and subq) Intramuscular injections are administered at a 90-degree angle to the skin, preferably into the anterolateral aspect of the thigh or the deltoid muscle of the upper arm, depending on the age of the patient Age group Needle length Injection site Children (birth-18 years) Neonates(a) 5/8 inch (16 mm)(b) Anterolateral thigh Infants, 1-12 months 1 inch (25 mm) Anterolateral thigh 1-1.25 inch (25-32 mm) Anterolateral thigh(c) Toddlers, 1-2 years 5/8(b)-1 inch (16-25 mm) Deltoid muscle of arm 5/8(b)-1 inch (16-25 mm) Deltoid muscle of arm(c) Children, 3-10 years 1-1.25 inches (25-32 mm) Anterolateral thigh 5/8(b)-1 inch (16-25 mm) Deltoid muscle of arm(c) Children, 11-18 years 1-1.5 inches (25-38 mm) Anterolateral thigh Subcutaneous injections are administered at a 45-degree angle, usually into the thigh for infants aged <12 months and in the upper-outer triceps area of persons aged ≥12 months. Subcutaneous injections may be administered into the upper-outer triceps area of an infant if necessary. A ⅝-inch, 23- to 25-gauge needle should be inserted into the subcutaneous tissue Kernicterus: which medication class associated When severe jaundice goes untreated for too long, it can cause a condition called kernicterus. Kernicterus is a type of brain damage that can result from high levels of bilirubin in a baby’s blood. It can cause athetoid cerebral palsy and hearing loss. Kernicterus also causes problems with vision and teeth and sometimes can cause intellectual disabilities. Early detection and management of jaundice can prevent kernicterus. Class that causes: sulfonamides Grey baby syndrome: which medication class associated Chloramphenicol-induced gray baby syndrome in newborns is due to decreased metabolism, so the decreased metabolism of chloramphenicol by glucoronyl transferases to the infants at the glucuronide metabolite occurs. This particular metabolic pathway appears to be age related and may take several months to 1 year to develop fully as evidenced by the increase in clearance of chloramphenicol with age up to 1 year Chloramphenicol is an antibiotic Lipid soluble drugs Preterm infants have much less body fat than full-term and therefore lipid soluble drugs may not accumulate in the preterm infant. There is substantially lower body fat in neonates than adults, so highly lipid soluble drugs are distributed less widely in infants than adults Aminoglycosides The aminoglycosides are frequently prescribed for infants and children, especially newborn infants with suspected or documented sepsis or meningitis. In older infants and children, the aminoglycosides are commonly used to treat acute respiratory exacerbations in patients with cystic fibrosis, intra-abdominal sepsis, complicated urinary tract infections, and other infections caused by gram-negative enteric bacilli. Tobramycin, vancomycin, and gentamicin Dosing based on weight Watch serum creatine for toxicity (ototoxicity & nephrotoxicity common) There are certain drugs; i.e., aminoglycosides that may be less toxic in pediatric patients than in adults, so in adults aminoglycoside toxicity is related to both peripheral compartment accumulation and individual patient’s inherent sensitivity to these tissue concentrations. Although neonatal peripheral tissue compartments for gentamicin have been reported to closely resemble those of adults with similar renal function, gentamicin is infrequently nephrotoxic in infants. This dissimilarity in the instance of nephrotoxicity; i.e., less nephrotoxicity in infants implies that newborn infants have less inherent tissue. Renal diseases: what they do to drugs Because most drugs are metabolized by the liver or eliminated by the kidneys, hepatic and renal disease are expected to decrease the dosage requirements in patients Tetracyclines Tetracyclines are not recommended for treatment in children younger than 8 years of age. This group is better used in younger children only when other drugs are likely to be in effective and when benefits clearly out weigh risks. Dosage schedules and strength of formulations differ. Tetracycline is available as 250/500 mg per tab/cap and doxycycline as 50/100 mg tab/cap Children can develop permanent brown discoloration of the teeth due to drug deposition, probably due to its chelating property and the formation of a tetracycline–calcium orthophosphate complex. Therefore, the risk is when the teeth are being calcified. The period of greatest danger is from mid pregnancy to about 4 to 6 months of the postnatal period for the deciduous anterior teeth, and from a few months to 5 years of age for the permanent anterior teeth. However, children up to 8 years old may be susceptible to this complication of tetracycline therapy. Enamel defects and hypoplasia can also occur. Tetracyclines are contraindicated during pregnancy, nursing, and children younger than 8 years, though, as a side note, the Centers for Disease Control and Prevention has recommended the use of doxycycline for initial prophylaxis after suspected bioterrorism related exposure to anthrax because the potential benefits here outweigh the potential risks among infants and children. Issues related to tetracyclines are dental staining and mammal defects within the baby and permanent teeth and a decrease in bone growth. Macrolide antibiotics Azithromycin (Zithromax) – Macrolide Antibiotic, Protein Synthesis Inhibitor, Binds 50 S o General Dosing: 10 – 12 mg/kg/dose on Day 1, 5 – 6 mg/kg/dose once daily for the duration (similar to z-pack) o Group A Strep: 12 mg/kg/dose once daily for 5 days o No renal dose adjustments (Caution GFR < 10 ml/min) o No hepatic adjustments though predominantly hepatically eliminated o Convenient once a day dosing-compliance should not be an issue Beta-lactam antibiotics Amoxicillin – Beta Lactam Antibiotic, Cell Wall Synthesis Inhibitor (CWI) o General Dosing: 25 – 45 mg/kg/day in divided doses q 12 hours ( Max 875mg/dose) o AOM: 80 – 90 mg/kg/day in divided doses q 12 hours (variable duration) o Adjust dose in Renal Impairment o No Hepatic adjustments o Inexpensive, well tolerated o Can treat Strep throat, pneumonia, ear infections, sinus infections Amoxicillin/Clavulanate – Augmentin – Beta Lactam + Beta Lactamase Inhibitor ( potassium clavulanate), CWI o Dosing varies based on age/weight o Commonly used to treat ear infections, sinus infections, pneumonia, infected bites, oral infections o High Dose (Augmentin ES) treats resistant Streptococcus pneumononiae o Take with food o Can commonly cause diarrhea / upset stomach if not taken with food Cefdinir – Cephalosporin, Beta Lactam Antibiotic, CWI o Broad spectrum, third generation cephalosporin o Acute Otitis Media (AOM): 7mg/kg/dose twice daily or 14mg/kg/dose once daily o Not usually first-line o Treats sinus infections, ear infections and pneumonia o More expensive o Renal adjustment CrCl < 30 ml/min o No hepatic adjustment o Cephalexin – Cephalosporin, Beta Lactam Antibiotic CWI o Narrower spectrum than cefdinir, first generation o General Dosing: 25 – 50 mg/kg/day divided every 6 to 12 hours o Treats strep throat, skin infections (cellulitis, impetigo) and bone/joint infections o Inexpensive o Renal adjustment CrCl < 50 ml/min o No hepatic adjustment Broad spectrum antibiotics: AOM Cefdinir, Augmentin (amoxicillin/clavulanate), amoxicillin Drugs to treat eczema and allergies Triamcinolone – Nasacort AQ nasal spray (OTC), triamcinolone acetonide cream (TAC)/ointment – Eczema flares and other skin rashes Singulair (Montelukast Sodium) – Antiasthmatic, Leukotriene Receptor Antagonist o Relieve symptoms of seasonal allergic rhinitis and perennial allergic rhinitis Fluticasone – Flonase nasal, Flovent MDI, Cutivate cream/ointment, Veramyst – Adrenal Corticosteroid, Antiasthmatic, Anti-Inflammatory o Dosing varies upon dosage form o Treats eczema, allergies and/or asthma Drugs to treat asthma Albuterol – ProAir HFA, Ventolin HFA – Short Acting Beta2 Agonist – Relaxes bronchial smooth muscles via Beta2 receptors o Bronchodilator, Sympathomimetic o Relieves Asthma Symptoms o Available Metered Dose Inhaler (MDI), Nebulization o Syrup – Rarely used in pediatrics o Inexpensive Fluticasone – Flonase nasal, Flovent MDI, Cutivate cream/ointment, Veramyst – Adrenal Corticosteroid, Antiasthmatic, Anti-Inflammatory o Dosing varies upon dosage form o Treats eczema, allergies and/or asthma o Generic Flonase is OTC (less expensive nasal allergy medication) Prednisolone Sodium Phosphate - Pediapred – Adrenal Corticosteroid, Antiasthmatic, Anti-Inflammatory o Available in 25mg/5ml and 15mg/5ml syrups **important to note which you are prescribing to prevent errors** o Commonly used to treat exacerbations of asthma, poison ivy, croup, other corticosteroid responsive disorders o Take with food, can cause hyperactivity-take earlier in the day o Make you urinate frequently Singulair (Montelukast Sodium) – Antiasthmatic, Leukotriene Receptor Antagonist o Use to prevent and treat asthma o Prevents exercise-induced asthma o Relieve symptoms of seasonal allergic rhinitis and perennial allergic rhinitis o Available as a generic o Monitor mood behavior changes (suicidal thinking/behavior) Prednisone – Adrenal corticosteroid – Treats a number of corticosteroid-responsive disorders in children, used in small dosages for short bursts for asthma flares, poison ivy and croup, etc. Prednisolone – liquid steroid commonly used to treat flare-ups of asthma, poison ivy reactions, croup Drug Calculations PEDIATRIC DOSAGE CALCULATIONS: o Most drugs in children are dosed according to weight (mg/kg) or body surface area (BSA) (mg/m2). Be cautious in converting lbs. to kg (or avoid lbs. altogether). Dosing also varies by indication. Use caution when looking up dosing to verify pediatric not adult indications. Many medications are available in different concentrations; always use the manufacturer’s directions for concentrations. KNOW THE FOLLOWING EQUIVALENCIES: o 1 gm = 1000 mg o 1 oz = 30 mL o 1 kg = 2.2 lbs o 1 mg = 1000 mcg o 5 mL = 1 tsp **Look at lecture powerpoint for examples** Drugs in infants Drugs in toddlers From the FaceBook Group! What does ADME stand for? Pharmacodynamics, Pharmacokinetics, Mechanism of Action, and Contraindication definitions Dosing of obese children Drug absorption Giving injections: sites in premature infants Which medication class is associated with Kernicterus? Which medication class is associated with Grey baby syndrome? Lipid Soluble drugs in pre-term infants Binding of Drugs-neonates Drug Metabolism in infants compared to older children Drugs in Infants Drugs in Toddlers Aminoglycosides toxicity Renal Diseases: What they do to drugs Tetracyclines Macrolide antiobiotic-treat? Beta-Lactam antibiotics Albuterol causes AOM: Broad –spectrum antibiotic 1st and 2nd line Drugs treating eczema, allergies, and asthma Drugs treating asthma Drug dose calculations