Community-Acquired Pneumonia: Prevention, Diagnosis, Treatment
advertisement

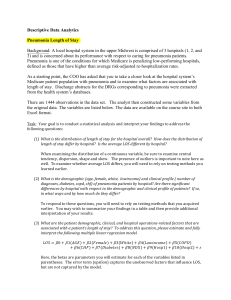
Annals of Internal MedicineT In the ClinicT Community-Acquired Pneumonia C ommunity-acquired pneumonia is an important cause of morbidity and mortality. It can be caused by bacteria, viruses, or fungi and can be prevented through vaccination with pneumococcal, influenza, and COVID-19 vaccines. Diagnosis requires suggestive history and physical findings in conjunction with radiographic evidence of infiltrates. Laboratory testing can help guide therapy. Important issues in treatment include choosing the proper venue, timely initiation of the appropriate antibiotic or antiviral, appropriate respiratory support, deescalation after negative culture results, switching to oral therapy, and short treatment duration. CME/MOC activity available at Annals.org. Physician Writer Michael B. Rothberg, MD, MPH Cleveland Clinic, Cleveland, Ohio doi:10.7326/AITC202204190 This article was published at Annals.org on 12 April 2022. CME Objective: To review current evidence for prevention, diagnosis, treatment, and practice improvement of community-acquired pneumonia. Funding Source: American College of Physicians. Acknowledgment: The author thanks Michael S. Niederman, MD, author of the previous version of this In the Clinic. Disclosures: Dr. Rothberg, ACP Contributing Author, reports grants or contracts from the Agency for Healthcare Research and Quality and the National Institute on Aging, consulting fees from Health Advances, participation on a data safety monitoring board or advisory board for BMS, and stock in Moderna. All relevant financial relationships have been mitigated. Disclosures can also be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M21-4473. With the assistance of additional physician writers, the editors of Annals of Internal Medicine develop In the Clinic using MKSAP and other resources of the American College of Physicians. The patient information page was written by Monica Lizarraga from the Patient and Interprofessional Partnership Initiative at the American College of Physicians. In the Clinic does not necessarily represent official ACP clinical policy. For ACP clinical guidelines, please go to https://www.acponline.org/clinical_information/ guidelines/. © 2022 American College of Physicians Prevention Treatment Diagnosis Practice Improvement Community-acquired pneumonia (CAP) can vary from a mild outpatient illness to a more severe disease requiring hospital admission or intensive care. In the United States, CAP together with influenza is the ninth leading cause of death overall and the leading cause of death from infectious disease (1). Outpatient CAP is managed mainly by primary care physicians, whereas inpatient treatment often involves hospitalists. The key management decisions related to CAP are recognition and treatment in a timely and effective manner, defining the appropriate site of care (home, hospital, or intensive care unit [ICU]), choosing effective treatment based on the cause, limiting antibiotic duration, and prevention. In particular, persons who have recently been hospitalized and received parenteral antibiotics and those who have previously been infected with multidrug-resistant organisms (MDROs) are at increased risk for resistant infections. Prevention Who is at increased risk for CAP? 1. Heron M. Deaths: Leading Causes for 2019. National Vital Statistics Reports. National Center for Health Statistics; 2021. 2. QuickStats: death rates from influenza and pneumonia among persons aged ≥65 years, by sex and age group— National Vital Statistics System, United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69:1470. [PMID: 33031359] 3. Nuorti JP, Butler JC, Farley MM, et al. Cigarette smoking and invasive pneumococcal disease. Active Bacterial Core Surveillance Team. N Engl J Med. 2000;342:681-9. [PMID: 10706897] 4. Gupta NM, Lindenauer PK, Yu PC, et al. Association between alcohol use disorders and outcomes of patients hospitalized with community-acquired pneumonia. JAMA Netw Open. 2019;2:e195172. [PMID: 31173120] 5. Patel MS, Patel SB, Steinberg MB. Smoking cessation. Ann Intern Med. 2021;174:ITC177-ITC192. [PMID: 34904907] 6. Kobayashi M, Farrar JL, Gierke R, et al. Use of 15valent pneumococcal conjugate vaccine and 20-valent pneumococcal conjugate vaccine among U.S. adults: updated recommendations of the Advisory Committee on Immunization Practices —United States, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:109-117. [PMID: 35085226] 7. Moberley S, Holden J, Tatham DP, et al. Vaccines for preventing pneumococcal infection in adults. Cochrane Database Syst Rev. 2013:CD000422. [PMID: 23440780] Persons with comorbid illness and elderly persons are at increased risk for pneumonia and for having a more complex course. The death rate from pneumonia per 100 000 persons increases rapidly with age, from 31.7 among adults aged 65 to 74 years to 377.6 among those aged 85 years or older (2). Existing respiratory disease, cardiovascular disease, diabetes mellitus, chronic liver disease, immunosuppression, chronic kidney disease, and previous splenectomy are associated with increased incidence of CAP. Cigarette smoking and alcohol misuse predispose to severe CAP and to bacteremic pneumococcal infection (3, 4). Patients should be screened for these conditions, should be advised to quit, and should be offered counseling and pharmacotherapy (5). Other common comorbid conditions include cancer and neurologic illnesses that predispose to aspiration, such as seizures and dementia. Who should receive pneumococcal vaccination, and when? Pneumococcal vaccination is recommended for all persons at increased risk for pneumococcal infection (Table 1). For persons without high-risk conditions, vaccination should be given at age 65 years. Patients with risk factors © 2022 American College of Physicians ITC50 In the Clinic should be vaccinated when the risk is first identified. New recommendations from the Centers for Disease Control and Prevention (CDC) vastly simplify the approach to vaccination (6). The 20-valent conjugate vaccine (PCV20) can be given in a single dose to all patients with risk factors or those aged 65 years or older. If PCV15 is administered instead, it should be followed by the 23-valent polysaccharide vaccine (PPSV23) 6 to 12 months later, or as soon as 8 weeks later for persons with cochlear implants, cerebrospinal fluid leaks, or immunosuppressive conditions. Persons who have previously received only PPSV23 should receive a dose of PCV15 or PCV20 at least 1 year later. A 2013 Cochrane review of pneumococcal vaccination found that it reduces the frequency of invasive pneumonia in healthy, immunocompetent adults (7). There was no evidence of effectiveness in adults with chronic illness, but there were very few events and CIs were wide. In a subsequent double-blind randomized controlled trial (RCT) of 84 496 adults older than 65 years, PCV13 prevented both bacteremic and nonbacteremic vaccine strain–specific pneumococcal pneumonia and vaccine-type invasive pneumococcal pneumonia; Annals of Internal Medicine April 2022 Table 1. Persons Eligible for Pneumococcal Vaccination Risk Group Characteristic or Underlying Medical Condition Older persons Immunocompetent persons Age ≥65 y Chronic heart disease* Chronic lung disease† Diabetes mellitus Cerebrospinal fluid leak Cochlear implant Alcoholism Chronic liver disease, cirrhosis Cigarette smoking Sickle cell disease/other hemoglobinopathy Congenital or acquired asplenia Congenital or acquired immunodeficiency‡ HIV infection Chronic renal failure Nephrotic syndrome Leukemia Lymphoma Hodgkin disease Generalized cancer Iatrogenic immunosuppression§ Solid organ transplant Multiple myeloma Persons with functional or anatomic asplenia Immunocompromised persons * Includes congestive heart failure and cardiomyopathies but excludes hypertension. † Includes chronic obstructive pulmonary disease, emphysema, and asthma. ‡ Includes B-lymphocyte (humoral) or T-lymphocyte deficiency, complement deficiencies (particularly C1, C2, C3, and C4 deficiencies), and phagocytic disorders (excluding chronic granulomatous disease). § Diseases requiring treatment with immunosuppressive drugs, including long-term systemic corticosteroids and radiation therapy. however, it did not reduce all-cause CAP or mortality (8). Over 4 years, it prevented 41 cases, for a number needed to treat of approximately 1000. In an RCT of 1006 nursing home residents in Japan, PPSV23 significantly reduced the frequency and mortality of pneumococcal pneumonia, as well as the frequency—but not the mortality—of all-cause pneumonia (9). What is the role of influenza vaccination in the prevention of CAP and its complications? Influenza is a common cause of CAP and may be complicated by bacterial co-infection (10). By limiting the spread of influenza, vaccination can reduce the incidence of CAP and protect vulnerable persons (11). The Advisory Committee on Immunization Practices (ACIP) recommends yearly influenza vaccine for all persons older than 6 months. Although patients with weakened immune systems, older patients, and those with chronic medical illnesses have the highest risk for hospitalization and death, even healthy adults can be hospitalized with influenza and can spread it to others. Details about specific influenza vaccines were reviewed in a previous In the Clinic article (12). Prevention... Physicians should screen for tobacco use at every visit; smokers should be advised to quit, be referred for counseling, and be offered pharmacologic treatment. Persons at risk for CAP and its complications should be offered pneumococcal and influenza vaccination, and all patients should be encouraged to get COVID-19 vaccination. CLINICAL BOTTOM LINE April 2022 Annals of Internal Medicine In the Clinic ITC51 8. Bonten MJ, Huijts SM, Bolkenbaas M, et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med. 2015;372:1114-25. [PMID: 25785969] 9. Maruyama T, Taguchi O, Niederman MS, et al. Efficacy of 23-valent pneumococcal vaccine in preventing pneumonia and improving survival in nursing home residents: double blind, randomised and placebo controlled trial. BMJ. 2010;340:c1004. [PMID: 20211953] 10. Bartley PS, Deshpande A, Yu PC, et al. Bacterial coinfection in influenza pneumonia: rates, pathogens, and outcomes. Infect Control Hosp Epidemiol. 2021:1-6. [PMID: 33890558] 11. Taksler GB, Rothberg MB, Cutler DM. Association of influenza vaccination coverage in younger adults with influenza-related illness in the elderly. Clin Infect Dis. 2015;61:1495503. [PMID: 26359478] 12. Uyeki TM. Influenza. Ann Intern Med. 2021;174: ITC161-ITC176. [PMID: 34748378] © 2022 American College of Physicians Diagnosis CAP accounts for only about 5% of respiratory complaints in the ambulatory setting. History and physical examination can help suggest the presence of pneumonia; predict the cause, which dictates treatment; and define severity, which determines the site of care. 13. Rowe TA, Jump RLP, Andersen BM, et al. Reliability of nonlocalizing signs and symptoms as indicators of the presence of infection in nursinghome residents. Infect Control Hosp Epidemiol. 2020:1-10. [PMID: 33292915] 14. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440-5. [PMID: 9356004] 15. Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination: relevant or relic. Arch Intern Med. 1999;159:1082-7. [PMID: 10335685] 16. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45e67. [PMID: 31573350] 17. Graffelman AW, le Cessie S , Knuistingh Neven A , et al. Can history and exam alone reliably predict pneumonia. J Fam Pract. 2007;56:465-70. [PMID: 17543257] 18. Hersh AL, King LM, Shapiro DJ, et al. Unnecessary antibiotic prescribing in US ambulatory care settings, 20102015. Clin Infect Dis. 2021;72:133-7. [PMID: 32484505] 19. Hopstaken RM, Witbraad T, van Engelshoven JM, et al. Inter-observer variation in the interpretation of chest radiographs for pneumonia in community-acquired lower respiratory tract infections. Clin Radiol. 2004;59:743-52. [PMID: 15262550] 20. Claessens YE, Debray MP, Tubach F, et al. Early chest computed tomography scan to assist diagnosis and guide treatment decision for suspected community-acquired pneumonia. Am J Respir Crit Care Med. 2015;192:974-82. [PMID: 26168322] How is the diagnosis made? CAP usually presents with both respiratory and systemic symptoms, particularly in young and immunocompetent persons. It should be suspected when the patient has cough, purulent sputum, pleuritic chest pain, dyspnea, fever, and chills. Among older patients and those with chronic illness, the disease may go unrecognized because fever may be absent or the patient may have nonrespiratory symptoms, such as confusion, weakness, lethargy, falling, poor oral intake, or decompensation of a chronic illness (for example, congestive heart failure [CHF]) (13). Most patients present acutely with symptoms for 1 to 2 days, but symptoms may be present for longer in older persons. Physical findings suggestive of pneumonia include fever or hypothermia, tachypnea, hypoxia, and rales or bronchial breath sounds on auscultation. Unfortunately, no single symptom or finding is sufficiently sensitive or specific to diagnose or rule out pneumonia, and prediction rules that combine several findings have failed to outperform physician judgment (14). Moreover, physicians' agreement on findings is often poor, and the prognostic value of the finding varies from one physician to the next (15). Thus, clinical diagnosis of pneumonia is often inaccurate, with overall sensitivity ranging from 70% to 90% and specificity ranging from 40% to 70% (16, 17). A chest radiograph (CXR) can confirm the diagnosis and identify certain complications. When signs and symptoms from history (cough, fever, dyspnea, pleuritic pain) and physical examination (focal crackles, © 2022 American College of Physicians ITC52 In the Clinic temperature ≥38 C) were used to predict the presence of radiographic pneumonia in a study of 129 patients with lower respiratory tract infection (26 with pneumonia), no combination of signs and symptoms was highly accurate. The positive predictive value of each varied from 17% to 43% (17). When should clinicians obtain a CXR? In general, when CAP is suspected, a CXR should be obtained. However, for otherwise healthy outpatients with clinical features strongly suggestive of CAP, it is reasonable to forego CXR, bearing in mind that prescribing antibiotics without a CXR may contribute to overuse, which is already a major issue in the United States (18). It is important to maintain a strong index of suspicion because elderly and immunosuppressed patients can have radiographic evidence of pneumonia without clinical features. It is especially important to obtain a CXR if the diagnosis is questionable or if pleural effusion, lung abscess, necrotizing pneumonia, or multilobar illness is suspected. Radiographs can aid patient management if findings of severe illness are present (bilateral, multilobar, or rapidly expanding infiltrates), but patterns rarely suggest a specific cause (for example, tuberculosis, Pneumocystis jirovecii). Radiologists frequently disagree on the presence of an infiltrate; thus, a negative study is more likely to rule out pneumonia than a positive one is to rule it in (19). However, if the patient has a convincing history and focal physical findings, pneumonia may be present even in the absence of a radiographic infiltrate. In this setting, computed tomography (CT) scans may be helpful. One singlecenter study found that routine CT scanning affected treatment in about 25% of cases (20). Another prospective study of older patients with suspected pneumonia found that 30% had their Annals of Internal Medicine April 2022 Table 2. Organisms That Commonly Cause Community-Acquired Pneumonia* Organisms Frequency, %† Bacteria Streptococcus pneumoniae Staphylococcus aureus Pseudomonas Escherichia coli Klebsiella Mycoplasma pneumoniae Chlamydophila pneumoniae Legionella pneumophila Haemophilus influenzae Other Streptococcus species Mycobacterium tuberculosis 14.0 5.1 1.6 <1 1.4 <1 1.9 <1 1.4 <1 <1 <1 Viruses Human rhinovirus Influenza A or B Adenovirus Human metapneumovirus Respiratory syncytial virus Parainfluenza virus Coronavirus 27.0 8.6 5.8 1.4 3.9 3.0 3.0 2.3 Fungi Histoplasma Coccidioides 1.0 <1 <1 * Adapted from reference 22. † No discernible cause is found in 62% of patients. treatment downgraded, and another 15% had it upgraded (21). The economic implications of routine CT scans for pneumonia diagnosis have not been established. However, because of the high cost and radiation exposure, it should be reserved for cases in which the diagnosis remains in doubt after CXR. viral–bacterial co-infection. The most commonly identified pathogens were human rhinovirus, influenza, and Streptococcus pneumoniae (pneumococcus); other common bacterial pathogens included Mycoplasma pneumoniae, Staphylococcus aureus, Legionella, and Enterobacteriaceae. Control patients had few or none of these pathogens. How is the cause determined? History and physical examination cannot determine the cause of pneumonia, which requires laboratory testing. However, the history can identify risk factors for MDROs, such as hospitalization with intravenous antibiotic therapy in the previous 90 days. This is important because treatment is usually empirical. History can also identify risk factors for less common causes of pneumonia, such as exposure to birds (Chlamydia psittaci, Cryptococcus neoformans) or bats (Histoplasma capsulatum) or travel to the southwestern United States CAP can be caused by viruses, bacteria, or fungi (Table 2). A prospective population-based surveillance study conducted at 3 hospitals in Chicago, Illinois, and 2 in Nashville, Tennessee, before the COVID-19 pandemic found that despite comprehensive diagnostic testing, a causative organism was isolated in only 38% of cases (22). Viruses were present in 27% of patients, bacteria in 14%, and fungi in 1%. Three percent of patients had April 2022 Annals of Internal Medicine In the Clinic ITC53 21. Prendki V, Scheffler M, Huttner B, et al. Low-dose computed tomography for the diagnosis of pneumonia in elderly patients: a prospective, interventional cohort study. Eur Respir J. 2018;51. [PMID: 29650558] 22. Jain S, Self WH, Wunderink RG, et al; CDC EPIC Study Team. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373:415-27. [PMID: 26172429] © 2022 American College of Physicians (endemic fungi, such as coccidioidomycosis). This information is useful if patients do not respond to usual therapy. 23. Klompas M, Imrey PB, Yu PC, et al. Respiratory viral testing and antibacterial treatment in patients hospitalized with communityacquired pneumonia. Infect Control Hosp Epidemiol. 2021;42:81725. [PMID: 33256870] 24. Schimmel JJ, Haessler S, Imrey P, et al. Pneumococcal urinary antigen testing in United States hospitals: a missed opportunity for antimicrobial stewardship. Clin Infect Dis. 2020;71:142734. [PMID: 31587039] 25. Self WH, Balk RA, Grijalva CG, et al. Procalcitonin as a marker of etiology in adults hospitalized with community-acquired pneumonia. Clin Infect Dis. 2017;65:183-90. [PMID: 28407054] 26. Upadhyay S, Niederman MS. Biomarkers: what is their benefit in the identification of infection, severity assessment, and management of community-acquired pneumonia. Infect Dis Clin North Am. 2013;27:19-31. [PMID: 23398863] 27. Christ-Crain M, Stolz D, Bingisser R, et al. Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med. 2006;174:84-93. [PMID: 16603606] 28. Vaughn VM, Flanders SA, Snyder A, et al. Excess antibiotic treatment duration and adverse events in patients hospitalized with pneumonia: a multihospital cohort study. Ann Intern Med. 2019;171:153-63. [PMID: 31284301] What is the role of laboratory tests? For outpatients, no tests are needed beyond pulse oximetry and a rapid influenza test during influenza season (12). For inpatients, additional testing may be required to define disease severity and identify the cause. Clinicians should measure pulse oximetry in all patients and arterial blood gases if carbon dioxide retention is suspected. Even with extensive diagnostic testing, a specific cause is found in fewer than half of patients (22). Blood culture results are positive in only about 10% of patients with CAP, and in low-risk patients (hospitalized without severe illness), the incidence of false-positive results may exceed the incidence of true-positive results, leading to potential overtreatment (16). Thus, blood cultures should not be ordered routinely. In patients with severe pneumonia and patients suspected of being infected with an MDRO or an unusual pathogen, 2 sets of blood cultures should be collected before therapy is started, and sputum should be collected if a goodquality sample can be obtained. Urine should be tested for Legionella and pneumococcal antigens. Serologic tests for viruses and atypical pathogens are not useful because they require convalescent titers in 6 to 8 weeks to identify infection. Rapid diagnostic tests for viral pathogens, such as rapid antigen testing, direct fluorescent antibody, or polymerase chain reaction (PCR), are available and should be considered, especially during local outbreaks (for example, during influenza season or a COVID-19 outbreak). The role of these tests in managing patients with CAP and in guiding antibiotic selection is not yet established, although some studies have shown that they may reduce unnecessary antibiotic use and increase antiviral prescribing, especially when results are positive for influenza (23). Similarly, testing for © 2022 American College of Physicians ITC54 In the Clinic COVID-19 can inform isolation and treatment. Other rapid diagnostic testing, such as streptococcal and Legionella urinary antigen testing, can reduce the use of overly broad empirical antibiotic coverage and promote antimicrobial stewardship (24). Measurement of serum procalcitonin has been proposed to differentiate between bacterial and viral infections. Levels are usually elevated with bacterial and Legionella infection, but not always with other atypical pathogens and not with viral infections (25). In prospective studies, however, the sensitivity is too low to reliably identify patients who do not require antibiotics, so procalcitonin is not recommended for this purpose. Alternatively, among hospitalized patients with an initially elevated procalcitonin level, serial measurements may help determine when to stop antibiotic therapy (26). A randomized trial of 302 patients hospitalized with CAP compared those managed with usual care versus those managed with an algorithm recommending antibiotics and the duration of therapy. The algorithm was based on serial measurement of procalcitonin levels on admission and after 6 to 24 hours, 4 days, 6 days, and 8 days. The procalcitonin-guided group had significantly less antibiotic use, and the duration of therapy was reduced from 12 to 5 days with similar clinical success (27). What other disorders should clinicians consider in patients suspected of having CAP? Most CAP responds to empirical antibiotics within 48 to 72 hours (28). If the patient does not respond within this window, clinicians should consider the possibility of a resistant bacterium; a virus; or unusual bacterial pathogens, such as Mycobacterium tuberculosis (which may be masked by a partial response to empirical quinolone therapy for CAP) or endemic fungi (histoplasmosis, coccidioidomycosis, blastomycosis). Clinicians should also consider noninfectious possibilities, such as bronchiolitis Annals of Internal Medicine April 2022 obliterans with organizing pneumonia, pulmonary vasculitis, hypersensitivity pneumonitis, interstitial diseases, lung cancer, lymphangitic carcinoma, bronchoalveolar cell carcinoma, lymphoma, or CHF. If the patient's condition deteriorates after an initial response to therapy, clinicians should consider pulmonary embolus; antibiotic-induced colitis; and the pneumonia complications of empyema, meningitis, and endocarditis. Diagnosis... History is valuable for defining risk factors for specific pathogens, and physical findings help define disease severity. Clinical findings are less dramatic in elderly persons. Clinicians should confirm the diagnosis of CAP with a CXR, or a CT scan if the CXR is negative and suspicion is high. Laboratory testing can also help to define severity and identify complications. Diagnosing specific pathogens early can help to guide antiviral therapy and empirical antibiotic selection. If the patient does not respond to initial therapy, a specialist should be consulted. CLINICAL BOTTOM LINE Treatment What is the overall approach to treatment, and how should clinicians determine whether a patient with CAP requires outpatient, inpatient, or ICU care? Treatment decisions are based on severity of illness. The first step is determining the appropriate site of care— outpatient, hospital, or ICU—and the second is choosing the appropriate treatment. Hospitalization decisions can be facilitated with the Pneumonia Severity Index (PSI) or the British Thoracic Society (BTS) rule (Figures 1 and 2), which predict risk for death. Patients at high risk are generally managed in the hospital. The PSI stratifies patients into 5 categories based on age, comorbid illness, physical examination findings, and laboratory data. In general, patients in classes I and II are treated as outpatients, those in class III require careful clinical assessment to determine the site of care, and those in classes IV and V are admitted to the hospital. The BTS rule, or “CURB-65,” evaluates patients for the presence of Confusion, blood Urea nitrogen level above 7.0 mmol/L (>19.6 mg/dL), Respiratory rate of 30 breaths/min or higher, systolic Blood pressure below April 2022 Annals of Internal Medicine 90 mm Hg or diastolic blood pressure of 60 mm Hg or lower, and age 65 years or older. Patients meeting at least 2 of these criteria are usually hospitalized (16, 29, 30). For select patients, a hospital-at-home program can substitute for inpatient care, reduce costs, and prevent readmissions (31). A prospective study of 3181 patients seen in 32 emergency departments compared the PSI with the CURB-65 criteria and found that both approaches accurately identified low-risk patients. CURB-65 was better for predicting mortality in high-risk patients (29). In another prospective study of 1651 patients, measurement of serum procalcitonin levels supplemented data obtained by prognostic scoring, and patients who had low procalcitonin levels had low mortality, regardless of PSI class or CURB-65 score (30). The PSI and CURB-65 were not developed to predict need for ICU care. Current guidelines recommend ICU care if the patient requires assisted ventilation, has septic shock requiring vasopressors, or has at least 3 of the following: respiratory rate of 30 breaths/ min or higher, PaO2–FiO2 ratio of 250 or In the Clinic ITC55 29. Aujesky D, Auble TE, Yealy DM, et al. Prospective comparison of three validated prediction rules for prognosis in communityacquired pneumonia. Am J Med. 2005;118:38492. [PMID: 15808136] 30. Huang DT, Weissfeld LA, Kellum JA, et al; GenIMS Investigators. Risk prediction with procalcitonin and clinical rules in community-acquired pneumonia. Ann Emerg Med. 2008;52:48-58.e2. [PMID: 18342993] 31. Levine DM, Ouchi K, Blanchfield B, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172:77-85. [PMID: 31842232] © 2022 American College of Physicians Figure 1. Pneumonia Severity Index for evaluating severity of illness in community-acquired pneumonia. Factor Demographic Factors Age Female sex Nursing home resident Comorbid Illnesses Neoplastic disease Liver disease Congestive heart failure Cerebrovascular disease Renal disease Physical Examination Findings Altered mental status Respiratory rate ≥30 breaths/min Systolic blood pressure <90 mm Hg Temperature <95 °F or ≥104 °F Pulse ≥125 beats/min Laboratory and Radiographic Findings Arterial pH <7.35 BUN level ≥30 mg/dL Sodium level <130 mEq/L Glucose level ≥250 mg/dL Hematocrit <30% PaO2 <60 mm Hg or oxygen saturation <90% Pleural effusion Score <51 51–70 71–90 91–130 >130 Risk Class I II III IV V Points 1 per year -10 +10 +30 +20 +10 +10 +10 +20 +20 +20 +15 +10 +30 +20 +20 +10 +10 +10 +10 Interpretation Mortality 0.1% 0.6% 0.9% 9.3% 27.0% Recommendation Outpatient Outpatient Careful assessment Inpatient Inpatient BUN = blood urea nitrogen. lower, multilobar infiltrates, confusion or disorientation, blood urea nitrogen level of 7.1 mmol/L (20 mg/dL) or higher, leukocyte count below 4 109 cells/L, platelet count below 100 109 cells/L, temperature below 36 C, and hypotension requiring aggressive fluid resuscitation (16). Figure 2. CURB-65 score for evaluating severity of illness in community-acquired pneumonia. 32. Gupta V, Yu KC, Schranz J, et al. A multicenter evaluation of the US prevalence and regional variation in macrolide-resistant S. pneumoniae in ambulatory and hospitalized adult patients in the United States. Open Forum Infect Dis. 2021;8: ofab063. [PMID: 34250183] Factor Confusion Blood Urea nitrogen level >19 mg/dL Respiratory rate ≥30 breaths/min Systolic Blood pressure <90 mm Hg or diastolic Blood pressure ≤60 mm Hg Age ≥65 y Total Score 0 or 1 2 ≥3 © 2022 American College of Physicians Points 1 1 1 1 1 _____ Interpretation Mortality Recommendation 1.5% Outpatient 9.2% Inpatient 22% Inpatient ITC56 In the Clinic Which antibiotics should be prescribed for outpatients? For patients without cardiopulmonary disease or factors that increase risk for infection with MDROs, the American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) guidelines recommend high-dose amoxicillin, doxycycline, or a macrolide (azithromycin, clarithromycin, or erythromycin), with macrolides appropriate only in areas where fewer than 25% of pneumococcal isolates are resistant to macrolides (Table 3; Appendix Table, available at Annals.org). In most of the United States, macrolide resistance now exceeds 30% (32). For outpatients with cardiopulmonary disease or factors that increase risk for infection with drug-resistant S pneumoniae (DRSP) or enteric gram-negative bacteria, treatment should include a respiratory Annals of Internal Medicine April 2022 Table 3. Initial Treatment Strategies for Inpatients With CAP, by Level of Severity and Risk for Drug Resistance Level of Severity Standard Regimen Prior Respiratory Isolation of MRSA Prior Respiratory Isolation of Pseudomonas aeruginosa Recent Hospitalization and Parenteral Antibiotics and Locally Validated Risk Factors for MRSA Recent Hospitalization and Parenteral Antibiotics and Locally Validated Risk Factors for P aeruginosa Nonsevere inpatient pneumonia* b-Lactam þ macrolide† or Add MRSA coverage§ and Add coverage for Obtain cultures but withObtain cultures but respiratory obtain cultures/nasal PCR P aeruginosa|| and obtain hold MRSA coverage initiate coverage for fluoroquinolone‡ to allow deescalation or cultures to allow deescala- unless culture results are P aeruginosa only if confirmation of need for tion or confirmation of positive culture results are positive continued therapy need for continued If rapid nasal PCR is availtherapy able, add coverage if PCR result is positive and obtain cultures Severe inpatient pneumonia* b-Lactam þ macrolide† or Add MRSA coverage§ and Add coverage for Add MRSA coverage§ and Add coverage for b-lactam þ fluoroquinoobtain cultures/nasal PCR P aeruginosa|| and obtain nasal PCR and cul- P aeruginosa|| and obtain lone‡ to allow deescalation or obtain cultures to allow tures to allow deescalation cultures to allow deescalaconfirmation of need for deescalation or confirma- or confirmation of need tion or confirmation of continued therapy tion of need for continued for continued therapy need for continued therapy therapy ATS = American Thoracic Society; CAP = community-acquired pneumonia; HAP = hospital-acquired pneumonia; IDSA = Infectious Diseases Society of America; MRSA = methicillin-resistant Staphylococcus aureus; PCR = polymerase chain reaction; VAP = ventilatorassociated pneumonia. * As defined by the 2007 ATS/IDSA CAP severity criteria guidelines. † Ampicillin þ sulbactam, 1.5 to 3 g every 6 hours; cefotaxime, 1 to 2 g every 8 hours; ceftriaxone, 1 to 2 g/d; or ceftaroline, 600 mg every 12 hours, and azithromycin, 500 mg/d, or clarithromycin, 500 mg twice daily. ‡ Levofloxacin, 750 mg/d, or moxifloxacin, 400 mg/d. § Per the 2016 ATS/IDSA HAP/VAP guidelines: vancomycin (15 mg/kg every 12 hours, adjust on basis of levels) or linezolid (600 mg every 12 hours). || Per the 2016 ATS/IDSA HAP/VAP guidelines: piperacillin–tazobactam (4.5 g every 6 hours), cefepime (2 g every 8 hours), ceftazidime (2 g every 8 hours), imipenem (500 mg every 6 hours), meropenem (1 g every 8 hours), or aztreonam (2 g every 8 hours). Does not include coverage for extended-spectrum b-lactamase–producing Enterobacteriaceae, which should be considered only on the basis of patient or local microbiological data. fluoroquinolone (levofloxacin or moxifloxacin) or a combination of a b-lactam (amoxicillin–clavulanate, cefpodoxime, or cefuroxime) with a macrolide or doxycycline. If the patient has received an antibiotic in the previous 3 months, antibiotics of the same class should be avoided. How long should outpatients continue antibiotic treatment? In general, it is important to keep antibiotic courses as short as possible to avoid adverse drug events and antibiotic resistance. The duration of therapy should be based on the patient's clinical response, severity of illness, and probable pathogen. Outpatients with mild to moderate CAP can be treated for as few as 3 to 5 days if clinical response is good, there has been no fever for 48 to 72 hours, and there are no signs of extrapulmonary infection (33). Persistent cough and sputum production are not reasons to prolong antibiotic therapy. April 2022 Annals of Internal Medicine How should clinicians follow patients during outpatient treatment? Up to 10% of patients initially managed at home do not respond to therapy and require hospitalization (34). The evidence base for home therapy is limited, but prudence dictates the need for careful follow-up. Patients should be told to measure their temperature orally every 8 hours and to report if it exceeds 38.3 C (101 F) or does not fall below 37.2 C (99 F) after 48 hours. Patients should be encouraged to drink 1 to 2 quarts of liquid daily and report if they cannot achieve this goal. Clinicians should instruct patients to report chest pain, severe or increasing shortness of breath, or lethargy. A follow-up visit, either in person or virtually, should be arranged in 24 to 48 hours to confirm the response to therapy. If the response is satisfactory, the patient should return for an examination in 10 to 14 days. At that time, In the Clinic ITC57 33. Dinh A, Ropers J, Duran C, et al; Pneumonia Short Treatment (PTC) Study Group. Discontinuing b-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC): a double-blind, randomised, placebo-controlled, noninferiority trial. Lancet. 2021;397:1195-203. [PMID: 33773631] 34. Tillotson G, Lodise T, Classi P, et al. Antibiotic treatment failure and associated outcomes among adult patients with community-acquired pneumonia in the outpatient setting: a real-world US insurance claims database study. Open Forum Infect Dis. 2020;7: ofaa065. [PMID: 32195289] © 2022 American College of Physicians pneumococcal and influenza vaccinations should be administered if they have not been previously. For patients whose symptoms resolve within 5 to 7 days, a follow-up CXR is not necessary (16). For smokers concerned about underlying lung cancer, routine screening with low-dose CT is appropriate. If the pneumonia is not resolving, additional imaging, laboratory testing, and microbiological work-up are indicated. 35. Centers for Medicare & Medicaid Services. Hospital Quality Initiative Overview. July 2008. 36. Meehan TP, Fine MJ, Krumholz HM, et al. Quality of care, process, and outcomes in elderly patients with pneumonia. JAMA. 1997;278:2080-4. [PMID: 9403422] 37. Kanwar M, Brar N, Khatib R, et al. Misdiagnosis of community-acquired pneumonia and inappropriate utilization of antibiotics: side effects of the 4h antibiotic administration rule. Chest. 2007;131:1865-9. [PMID: 17400668] 38. Horita N, Otsuka T, Haranaga S, et al. Betalactam plus macrolides or beta-lactam alone for community-acquired pneumonia: a systematic review and meta-analysis. Respirology. 2016;21:1193-200. [PMID: 27338144] 39. Martínez JA, Horcajada JP, Almela M, et al. Addition of a macrolide to a beta-lactam-based empirical antibiotic regimen is associated with lower in-hospital mortality for patients with bacteremic pneumococcal pneumonia. Clin Infect Dis. 2003;36:389-95. [PMID: 12567294] 40. Lujan M, Gallego M, Fontanals D, et al. Prospective observational study of bacteremic pneumococcal pneumonia: effect of discordant therapy on mortality. Crit Care Med. 2004;32:625-31. [PMID: 15090938] 41. Yu VL, Chiou CC, Feldman C, et al; International Pneumococcal Study Group. An international prospective study of pneumococcal bacteremia: correlation with in vitro resistance, antibiotics administered, and clinical outcome. Clin Infect Dis. 2003;37:230-7. [PMID: 12856216] What is the approach to antibiotic therapy for patients hospitalized with CAP outside the ICU? Patients should receive initial antibiotic therapy as soon as possible after diagnosis. Although therapy within 4 hours of arrival in the emergency department has been associated with reduced mortality, an undue emphasis on early therapy may lead to unnecessary use of antibiotics and associated complications (35, 36). In 1 study, the final diagnosis of pneumonia in patients suspected of having it in the emergency department decreased from 75.9% to 58.9% after initiation of a program to give patients antibiotics within 4 hours of arrival in the emergency department (37). Specific therapies should be guided by the diagnosis. Patients at risk for infection with methicillin-resistant S aureus (MRSA), DRSP, and resistant gram-negative organisms require extendedspectrum empirical therapy. Many risk factors have been identified for each of these infections, but they tend to be only weakly associated and should not be relied on when choosing therapy. Importantly, the previous designation of health care–associated pneumonia has been abandoned because it was not particularly associated with resistant infections and led to increased use of extended-spectrum antibiotics. The 2 consistently strong risk factors are previous isolation of the resistant organism, especially from the respiratory tract, and hospitalization within 90 days with administration of antibiotics. Despite multiple attempts to create models © 2022 American College of Physicians ITC58 In the Clinic to identify resistant organisms based on patient risk factors, none have been sufficiently validated for use in clinical practice. Such validation is important because the prevalence of resistant organisms is low and varies among hospitals. Recognizing this fact, the ATS/IDSA guidelines recommend that hospitals validate their own local risk factors or else treat patients on the basis of a history of resistant infections or recent hospitalization with antibiotics. If available, rapid nasal PCR for MRSA can be used to guide empirical therapy. Patients with influenza pneumonia should receive treatment with a neuraminidase inhibitor, even if they have been sick for more than 48 hours (12). Because co-infection is common, they should also receive antibiotics, at least until culture results are available. Such patients are at increased risk for S aureus infection but not for MRSA and may therefore be treated with standard antibiotics (10). For patients without risk factors for resistant bacteria, guidelines recommend treatment with either an intravenous or oral quinolone (levofloxacin, 750 mg/d, when renal function is normal, or moxifloxacin, 400 mg/d) or the combination of a b-lactam (cefotaxime, ceftriaxone, ampicillin–sulbactam, or high-dose ampicillin, but not cefuroxime) plus a macrolide or doxycycline (16). The addition of a macrolide to a b-lactam has been associated with reduced mortality, although this benefit may be limited to patients with severe pneumonia (38). Even those with bacteremic pneumococcal pneumonia seem to benefit from added macrolide coverage (39). Specific b-lactams, such as ceftriaxone and cefotaxime, are preferred if DRSP is suspected because they are effective at mean inhibitory concentrations up to 2 mg/L (40). However, 1 study showed increased mortality when cefuroxime was used in patients with bacteremic DRSP (41). An international study of 4337 hospitalized patients with CAP showed that approximately 20% had evidence of Annals of Internal Medicine April 2022 atypical pathogen infection and that therapy directed against these organisms decreased time to clinical stability, length of stay, and both total and CAPrelated mortality (42). Another study of 2209 hospitalized Medicare patients with bacteremic pneumonia found that therapy directed at atypical pathogens reduced 30-day mortality and 30-day readmission rate, but the benefits occurred only with macrolides and not with fluoroquinolones (43). Patients who have had a resistant organism in the past should receive therapy directed at the previously isolated organism. Therapy for suspected MRSA includes vancomycin (15 mg/kg every 12 hours, with adjustment based on levels) or linezolid (600 mg every 12 hours) but may be withheld if nasal PCR results are negative. Therapy for suspected gram-negative infections includes piperacillin–tazobactam (4.5 g every 6 hours), cefepime (2 g every 8 hours), ceftazidime (2 g every 8 hours), imipenem (500 mg every 6 hours), meropenem (1 g every 8 hours), or aztreonam (2 g every 8 hours). If culture results are negative at 48 hours and the patient is clinically stable, the antibiotic regimen may be deescalated. Although there are no randomized trials of deescalation after negative culture results, there is a strong evidence base from observational studies. A study of 165 U.S. hospitals found that among 14 170 patients who received extended-spectrum antibiotics, only 13% had them deescalated by hospital day 4. Deescalation seemed to be safe and was associated with lower odds of subsequent transfer to the ICU (adjusted odds ratio, 0.38 [95% CI, 0.18 to 0.79]), shorter hospital stay, and lower costs in propensity-matched analyses. Importantly, hospital deescalation rates ranged from 2% to 35%, and even hospitals in the top quartile of deescalation failed to deescalate more than 50% of their lowest-risk patients, leaving ample room for improvement (44). April 2022 Annals of Internal Medicine Patients whose only risk factor is recent hospitalization with antibiotic administration should have cultures obtained, but antibiotics against MRSA or Pseudomonas should be withheld unless culture results are positive or the patient's condition deteriorates. Which antibiotics should be given to patients admitted to the ICU? Patients in the ICU should receive empirical therapy with at least 2 antibiotics (16). Clinicians should assess for risk factors for Pseudomonas aeruginosa and treat those without risk factors with intravenous ceftriaxone or cefotaxime plus either azithromycin or a respiratory quinolone. Patients with risk factors should be treated with an intravenous, antipseudomonal b-lactam (cefepime, piperacillin–tazobactam, imipenem, meropenem) plus an intravenous quinolone effective against P aeruginosa (ciprofloxacin or highdose levofloxacin). Alternatively, an intravenous, antipseudomonal b-lactam combined with an aminoglycoside (amikacin, gentamicin, or tobramycin) plus either an intravenous macrolide (azithromycin or erythromycin) or an intravenous antipneumococcal quinolone (levofloxacin or moxifloxacin) should be used. In studies of patients admitted to the ICU with severe CAP, mortality was reduced when combination therapy was used; monotherapy, even with a quinolone, was not as effective. A 2012 meta-analysis of 28 observational studies involving nearly 10 000 critically ill patients found that macrolide use (generally in a combination regimen) was associated with an 18% reduction in mortality compared with nonmacrolide regimens and that a b-lactam–macrolide combination had a trend toward reduced mortality compared with a b-lactam–quinolone regimen (45). In patients with bacteremic pneumococcal pneumonia and critical illness, studies have found that mortality was lower with combination therapy than with monotherapy (46). In the Clinic ITC59 42. Arnold FW, Summersgill JT, Lajoie AS, et al; Community-Acquired Pneumonia Organization (CAPO) Investigators. A worldwide perspective of atypical pathogens in community-acquired pneumonia. Am J Respir Crit Care Med. 2007;175:1086-93. [PMID: 17332485] 43. Metersky ML, Ma A, Houck PM, et al. Antibiotics for bacteremic pneumonia: improved outcomes with macrolides but not fluoroquinolones. Chest. 2007;131:466-73. [PMID: 17296649] 44. Deshpande A, Richter SS, Haessler S, et al. De-escalation of empiric antibiotics following negative cultures in hospitalized patients with pneumonia: rates and outcomes. Clin Infect Dis. 2021;72:131422. [PMID: 32129438] 45. Sligl WI, Asadi L, Eurich DT, et al. Macrolides and mortality in critically ill patients with communityacquired pneumonia: a systematic review and meta-analysis. Crit Care Med. 2014;42:420-32. [PMID: 24158175] 46. Baddour LM, Yu VL, Klugman KP, et al; International Pneumococcal Study Group. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Respir Crit Care Med. 2004;170:440-4. [PMID: 15184200] © 2022 American College of Physicians 47. Girou E, Schortgen F, Delclaux C, et al. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA. 2000;284:2361-7. [PMID: 11066187] 48. Stern A, Skalsky K, Avni T, et al. Corticosteroids for pneumonia. Cochrane Database Syst Rev. 2017;12:CD007720. [PMID: 29236286] 49. Horby P, Lim WS, Emberson JR, et al; RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384:693-704. [PMID: 32678530] 50. Belforti RK, Lagu T, Haessler S, et al. Association between initial route of fluoroquinolone administration and outcomes in patients hospitalized for communityacquired pneumonia. Clin Infect Dis. 2016;63:1-9. [PMID: 27048748] 51. Fishbane S, Niederman MS, Daly C, et al. The impact of standardized order sets and intensive clinical case management on outcomes in community-acquired pneumonia. Arch Intern Med. 2007;167:1664-9. [PMID: 17698690] 52. Ciarkowski CE, Timbrook TT, Kukhareva PV, et al. A pathway for communityacquired pneumonia with rapid conversion to oral therapy improves health care value. Open Forum Infect Dis. 2020;7: ofaa497. [PMID: 33269294] 53. Graham WG, Bradley DA. Efficacy of chest physiotherapy and intermittent positive-pressure breathing in the resolution of pneumonia. N Engl J Med. 1978;299:624-7. [PMID: 355879] 54. Yang M, Yan Y, Yin X, et al. Chest physiotherapy for pneumonia in adults. Cochrane Database Syst Rev. 2013:CD006338. [PMID: 23450568] 55. Stefan MS, Priya A, Pekow PS, et al. The comparative effectiveness of noninvasive and invasive ventilation in patients with pneumonia. J Crit Care. 2018;43:190-6. [PMID: 28915393] What are the other components of ICU care for CAP? Hydration should be ensured and supplemental oxygen should be given to maintain oxygen saturation above 90%. Chest physiotherapy should be considered. Intubation and mechanical ventilation are required in patients with oxygen saturation below 90% on maximal mask oxygen, inability to clear secretions, inability to protect the airway, or hypercarbia. If the patient has only hypoxemia or hypercarbia and is alert and cooperative, noninvasive positive-pressure ventilation should be considered. This therapy is associated with fewer complications than endotracheal intubation, including ventilatorassociated pneumonia (47). Studies of steroids in CAP tend to be small and heterogeneous in nature (48). Many are subject to bias and report problematic outcomes, such as length of stay. Therefore, routine use of systemic corticosteroids is not recommended, but patients with refractory septic shock (16) or COVID-19 requiring ventilator support may benefit from steroids (49). When can clinicians transition hospitalized patients from intravenous to oral antibiotics? Switching to oral antibiotics is indicated once cough, sputum production, and dyspnea improve; the patient is afebrile on 2 occasions 8 hours apart; and they are able to take oral medications. This switch can be made as early as 24 to 48 hours after admission and can be done safely even if pneumococcal bacteremia has been documented. Longer durations of therapy are usually needed for patients infected with P aeruginosa or S aureus and for those with extrapulmonary complications, such as empyema or meningitis, but should be individualized to specific patient situations. An oral regimen that covers all organisms isolated in blood or sputum cultures and corresponds to the intravenous therapy should be selected. For some patients, this means a blactam–macrolide combination or qui- © 2022 American College of Physicians ITC60 In the Clinic nolone monotherapy. Patients who have responded to a b-lactam–macrolide combination can be continued on macrolide monotherapy unless culture results justify dual therapy. Quinolones have excellent oral bioavailability. For patients with a working gastrointestinal tract, there is little added benefit to intravenous quinolones (50). To facilitate a switch to oral therapy, hospitals should consider using a standing order set supplemented by antibiotic stewardship. Such programs have been shown to reduce the number of days patients receive intravenous therapy and shorten hospital stay (51). Gains seem to be maintained even after stewardship efforts are reduced, and the program can save money (52). What is the role of nondrug therapies? In outpatients, nondrug therapy consists of oral hydration. For hospitalized patients, nondrug therapies include intravenous hydration and oxygen for hypoxemia. Chest physiotherapy has not been widely studied but can improve outcomes in patients with pneumonia who have more than 30 mL of sputum per day and impaired clearance of secretions (53). A 2013 meta-analysis of 6 randomized trials involving 434 patients evaluated the following 4 types of chest physiotherapy: conventional chest physiotherapy, active cycle breathing, osteopathic manipulation, and positive expiratory pressure. No method reduced mortality, but osteopathic manipulation and positive expiratory pressure reduced the duration of hospital stay by 2.02 and 1.4 days, respectively (54). In severely ill patients, nondrug therapy can include noninvasive ventilatory support and mechanical ventilation for those with respiratory failure. One observational study found that noninvasive ventilation was associated with lower mortality, but only for patients with comorbid chronic obstructive pulmonary disease (COPD) or CHF (55). Annals of Internal Medicine April 2022 When should a consultation be requested for hospitalized patients, and which types of specialists or subspecialists should be consulted? An infectious disease consultation is appropriate if there are questions about initial antibiotic therapy or when the patient does not respond to initial therapy. Questions about appropriate site of care or the need for vasopressors or ventilatory support are appropriate indications for critical care consultation. Pulmonary or thoracic surgical consultation is appropriate for placement of a chest tube if a complicated parapneumonic effusion or empyema is found on thoracentesis because early therapy can reduce hospital stay and avoid complications. Cardiology consultation may be needed in cases of ischemia or CHF. In a study of 170 patients with pneumococcal pneumonia, 19.4% had at least 1 major cardiac event, including 12 with acute myocardial infarction, 8 with newonset atrial fibrillation or ventricular tachycardia, and 13 with newly diagnosed or worsening heart failure without other cardiac complications. Patients with cardiac events had significantly higher mortality (27.3% vs. 8.8%) (56). When can patients be discharged from the hospital, and how long should antibiotics be continued? Patients can be discharged once they are clinically stable (temperature ≤37.8 C, heart rate <100 beats/min, respiratory rate <24 breaths/min, oxygen saturation ≥90%, systolic blood pressure ≥90 mm Hg, and normal mental status) (57). Therapy may be continued after discharge, but the total duration should not exceed 5 to 7 days. In some cases, 3 days may be sufficient (33). Excess treatment is common, particularly after discharge, and is associated with increased incidence of adverse drug events (28). If switching to oral therapy, it is not necessary to observe the response in the April 2022 Annals of Internal Medicine hospital. In one study, clinically stable patients were observed on oral therapy before discharge, and no deterioration occurred (58). Another study compared patients who remained in the hospital for 1 day after the switch with those discharged on the same day and found no differences in mortality or 14-day readmission rate (59). Patients may be discharged on intravenous antibiotics as long as they are clinically stable; consultation with an infectious disease specialist can ensure that the duration and route of outpatient therapy are appropriate (60). Programs directed by infectious disease specialists seem to produce better outcomes at lower costs (61). What are the indications for followup CXR after discharge? Routine CXR before discharge is unnecessary, but patients who do not achieve clinical stability and those who deteriorate despite therapy require an aggressive evaluation, including CXR. As with outpatient pneumonia, if the patient has a good clinical response to therapy, CXR need not be repeated. How can patients prevent recurrent CAP? Patients should receive pneumococcal and influenza vaccinations; avoid smoking; and optimize treatment of comorbid illnesses, such as CHF and COPD. They should be evaluated for medical conditions that could predispose them to recurrent infection. One study found that 6% of patients with CAP had a new comorbid condition, including diabetes mellitus, cancer, COPD, and HIV infection (62). If pneumonia recurs in the same location, the possibility of bronchiectasis, aspirated foreign body, or endobronchial obstruction should be considered. Recurrent pneumonia or pneumonia with an unusual pathogen may signal immunodeficiency. In the Clinic ITC61 56. Musher DM, Rueda AM, Kaka AS, et al. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis. 2007;45:15865. [PMID: 17578773] 57. Mandell LA, Wunderink RG, Anzueto A, et al; Infectious Diseases Society of America. Infectious Diseases Society of America/ American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44 Suppl 2: S27-72. [PMID: 17278083] 58. Rhew DC, Hackner D, Henderson L, et al. The clinical benefit of in-hospital observation in ‘lowrisk’ pneumonia patients after conversion from parenteral to oral antimicrobial therapy. Chest. 1998;113:142-6. [PMID: 9440581] 59. Nathan RV, Rhew DC, Murray C, et al. In-hospital observation after antibiotic switch in pneumonia: a national evaluation. Am J Med. 2006;119:512.e1-7. [PMID: 16750965] 60. Sharma R, Loomis W, Brown RB. Impact of mandatory inpatient infectious disease consultation on outpatient parenteral antibiotic therapy. Am J Med Sci. 2005;330:60-4. [PMID: 16103785] 61. Shah A, Petrak R, Fliegelman R, et al. Infectious diseases specialty intervention is associated with better outcomes among privately insured individuals receiving outpatient parenteral antimicrobial therapy. Clin Infect Dis. 2019;68:1160-5. [PMID: 30247512] 62. Falguera M, Martín M, Ruiz-González A, et al. Community-acquired pneumonia as the initial manifestation of serious underlying diseases. Am J Med. 2005;118:37883. [PMID: 15808135] © 2022 American College of Physicians In a 2014 review of 12 studies, the 30-day readmission rate for patients with CAP varied from 16.8% to 20.1% (63). Pneumonia caused the readmission only 17.9% to 29.4% of the time; other common causes were exacerbations of CHF or COPD. Treatment... The most important clinical decisions in the treatment of CAP include determining the site of care, selecting antibiotic therapy, delivering supportive care, and determining the need for ventilatory support. Antibiotic therapy differs by site of care. However, all patients should receive timely empirical therapy directed at pneumococcus, atypical pathogens, and other organisms depending on risk factors. The PSI and the CURB-65 score aid decisions about hospital admission. Patients should be managed in the ICU if they require ventilatory or vasopressor support or close observation. Consultation should occur in cases of severe disease and when patients do not respond to initial therapy or have complications. Broad-spectrum empirical antibiotics should be deescalated promptly after negative culture results, and patients can be transitioned to oral antibiotics and discharged once they are clinically stable. Routine follow-up CXR is unnecessary if the patient is responding well. Patients should be offered pneumococcal, COVID-19, and influenza vaccinations and should be encouraged to avoid smoking. CLINICAL BOTTOM LINE Practice Improvement What measures do stakeholders use to measure the quality of care? 63. Prescott HC, Sjoding MW, Iwashyna TJ. Diagnoses of early and late readmissions after hospitalization for pneumonia. A systematic review. Ann Am Thorac Soc. 2014;11:1091-100. [PMID: 25079245] 64. Werner RM, Bradlow ET. Relationship between Medicare's Hospital Compare performance measures and mortality rates. JAMA. 2006;296:2694-702. [PMID: 17164455] 65. Lee RA, Centor RM, Humphrey LL, et al; Scientific Medical Policy Committee of the American College of Physicians. Appropriate use of short-course antibiotics in common infections: best practice advice from the American College of Physicians. Ann Intern Med. 2021;174:822-7. [PMID: 33819054] 66. Centers for Disease Control and Prevention. Core Elements of Hospital Antibiotic Stewardship Programs. Accessed at www.cdc.gov/antibioticuse/core-elements/ hospital.html on 10 January 2022. Process measures for pneumonia quality of care, including measurement of oxygenation, prompt initiation of appropriate antibiotics, drawing of blood cultures before antibiotic administration, providing smoking cessation counseling, and administration of influenza and pneumococcal vaccine, are no longer collected or publicly reported by the Centers for Medicare & Medicaid Services (CMS). Pneumonia is not one of the conditions for which CMS requires core measures. Instead, CMS reports risk-standardized mortality, readmission, and excess days in acute care for patients with pneumonia. Although attention to the previous © 2022 American College of Physicians ITC62 In the Clinic process measures represents good care, it may not affect these outcomes (64), which are influenced by various medical and social conditions. What do professional organizations recommend with regard to prevention and treatment? The ATS and IDSA issue joint guidelines on the treatment of CAP (16). The American College of Physicians has issued a guideline on appropriate use of short-course antibiotics, which includes treatment of CAP (65). The CDC publishes the ACIP recommendations for influenza, COVID-19, and pneumococcal vaccination and Core Elements of Antibiotic Stewardship (66). The recommendations in this article reflect these guidelines. Annals of Internal Medicine April 2022 Tool Kit Community-Acquired Pneumonia Patient Information https://medlineplus.gov/pneumonia.html https://medlineplus.gov/languages/ pneumonia.html Information and handouts in English and other languages from the National Institutes of Health's MedlinePlus. www.nhlbi.nih.gov/health/pneumonia www.nhlbi.nih.gov/health-topics/espanol/ neumonia Information in English and Spanish from the National Heart, Lung, and Blood Institute. www.cdc.gov/pneumococcal/index.html www.cdc.gov/pneumococcal/index-sp. html Information on pneumococcal disease in English and Spanish from the Centers for Disease Control and Prevention. Information for Health Professionals www.atsjournals.org/doi/full/10.1164/ rccm.201908-1581ST 2019 clinical practice guideline on diagnosis and treatment of adults with communityacquired pneumonia from the American Thoracic Society and the Infectious Diseases Society of America. www.cdc.gov/vaccines/vpd/pneumo/hcp/ index.html Pneumococcal vaccination information and resources from the Centers for Disease Control and Prevention. www.cdc.gov/pneumococcal/clinicians/ index.html Information on pneumococcal disease in English and Spanish from the Centers for Disease Control and Prevention. April 2022 Annals of Internal Medicine In the Clinic ITC63 In the Clinic In the Clinic © 2022 American College of Physicians In the Clinic Annals of Internal Medicine WHAT YOU SHOULD KNOW ABOUT PNEUMONIA What Is Pneumonia? Pneumonia is a serious infection of the lungs. Community-acquired pneumonia is when you develop pneumonia outside a hospital or nursing home. Pneumonia can be caused by bacteria, viruses, or fungi and can range from mild to severe. It is important that pneumonia be identified and treated quickly. What Are the Symptoms? Fever or chills A cough that produces a lot of mucus Chest pain that is worse with deep breathing Shortness of breath Feeling tired and weak Confusion What Are the Risk Factors? • Being age 65 years or older • Having other health conditions, like diabetes or lung, heart, liver, or kidney disease Drinking alcohol Smoking cigarettes Having the flu or COVID-19 Having a weakened immune system Pneumonia can be prevented by quitting smoking and by receiving vaccines. The pneumococcal, influenza, and COVID-19 vaccines have all been shown to prevent pneumonia and its complications. • • • • How Is It Diagnosed? • Your doctor will take a history; check your vital signs, including your oxygen level; and perform a physical examination. • You might be given a flu test or a COVID-19 test. • You might have other tests. A chest x-ray may be helpful to confirm the diagnosis. You may need to have a chest CT scan. Tests of the sputum (the mucus you produce when coughing) or urine may help your doctor learn what type of bacteria is causing your pneumonia. Blood tests may help determine the severity of the infection. How Is It Treated? • Treatment depends on how severe your pneu- • • • • • monia is. Your doctor will determine whether you can be treated at home or in the hospital. Most patients can be treated at home. Some who are very ill or have a risk for complications might need to stay in the hospital. If you have to stay in the hospital, your doctor will monitor your heart and breathing rates, and you might be given IV fluids or medicine. If your pneumonia is caused by bacteria, your doctor will prescribe antibiotics. Symptoms usually start to go away within 2 to 3 days of starting medicine. It is important to finish all of your antibiotics, even if you are feeling better. Follow up with your doctor 1 to 2 days after starting antibiotics to make sure you are responding well. Drink plenty of fluids and stay hydrated. Get plenty of rest. Feeling tired and coughing may last for a month or longer. Questions for My Doctor • • • • • Should I be treated at home or in the hospital? What medicine do I need to take? What can I do to help relieve my symptoms? When should I have a follow-up visit? How can I prevent another episode of pneumonia? For More Information American Lung Association www.lung.org/lung-health-diseases/lung-disease-lookup/ pneumonia MedlinePlus https://medlineplus.gov/pneumonia.html © 2022 American College of Physicians ITC64 In the Clinic Annals of Internal Medicine April 2022 Patient Information • • • • • • Appendix Table. Drug Treatments for CAP Agent Mechanism of Action Dosage Benefits Adverse Effects Notes Linezolid (Zyvox) Bacteriostatic; binds to 50S ribosomal subunit to inhibit bacterial protein synthesis 600 mg PO or IV every 12 h Penetrates well into the lung and is active against MRSA Myelosuppression, particularly thrombocytopenia, vomiting, diarrhea, seizures, hypoglycemia Drug interactions may lead to serotonin syndrome Do not use with tricyclic antidepressants, monoamine oxidase inhibitors, or selective serotonin reuptake inhibitors Monitor blood pressure Clindamycin* (Cleocin) Bacteriostatic; binds to 50S ribosomal subunit to inhibit bacterial protein synthesis 600 mg PO every 8 h Can inhibit toxin production by MRSA Diarrhea, esophagitis, hypersensitivity Can cause Clostridioides difficile– associated diarrhea Caution with asthma, severe hepatic disease Vancomycin (Vancocin) Bactericidal; inhibits cell wall and RNA synthesis 15–20 mg/kg IV every 8–12 h Active against MRSA, with extensive clinical experience Is not therapy for methicillin-susceptible Staphylococcus aureus Ototoxicity, nephrotoxicity, neutropenia, nausea, hypokalemia Avoid rapid infusion (causes histamine release) Avoid optimal extravasation Monitor trough concentrations In chronic kidney disease, individualize dose Bactericidal; interferes with peptidoglycan cross-linking and prevents formation of the bacterial cell wall Piperacillin–tazobactam: 3.375 mg IV every 4–6 h Cefepime: 1–2 g IV every 12 h Imipenem: 1 g IV every 8h Meropenem: 1 g IV every 8 h Active against pneumococci and Pseudomonas aeruginosa Anaphylaxis, rash, nausea, vomiting, diarrhea, phlebitis, seizures (high doses), hypokalemia (high doses), elevated liver enzymes, prolonged prothrombin time (especially if patient is using coumadin) Seizure potential greater with imipenem than meropenem Only use for patients with pseudomonal risk factors, although generally active against DRSP Can dose daily if patient has renal insufficiency Bactericidal; interferes with peptidoglycan cross-linking and prevents formation of the bacterial cell wall Cefuroxime: 500 mg PO twice daily Cefpodoxime: 400 mg PO twice daily Ceftriaxone: 1–2 g every 12–24 h (usually every 24 h) Cefotaxime: 1 g every 8h Active against pneumococci and Haemophilus influenzae, including b-lactamase–producing organisms Anaphylaxis, rash, nausea, vomiting, diarrhea, elevated liver function test results, interstitial nephritis, altered coagulation, pseudomembranous colitis Not to be used alone in CAP Combine with a macrolide Although cefuroxime can be used as oral therapy, it should not be used IV because it is not as active against DRSP as other cephalosporins Antibiotics for community-acquired MRSA Antipseudomonal b-lactams Piperacillin– tazobactam Cefepime Imipenem Meropenem Cephalosporins Cefuroxime Cefpodoxime Ceftriaxone Cefotaxime Continued on following page April 2022 Annals of Internal Medicine In the Clinic © 2022 American College of Physicians Appendix Table—Continued Agent Mechanism of Action Dosage Benefits Adverse Effects Notes Bacteriostatic; binds to 30S ribosomal subunit to inhibit bacterial protein synthesis 100 mg IV initially, then 50 mg IV every 12 h Infuse over 30–60 min Can be used for CAP, but only when there are no other options Penetrates well into respiratory secretions; active against pneumococcus and atypical pathogens, but not P aeruginosa Vomiting, diarrhea, hepatotoxicity, pancreatitis, anemia Increase in all-cause mortality Avoid with pregnancy With severe hepatic disease, use 25 mg for maintenance infusion Bacteriostatic; binds to 50S ribosomal subunit and inhibits bacterial protein synthesis Azithromycin: 500 mg IV or PO on day 1, followed by 500 mg IV or PO for 7–10 d for hospitalized patients (250 mg on days 2–5 for outpatients) Azithromycin in the microspheres oral extended-release formulation: 2 g PO on day 1 without followup dosing for outpatients Clarithromycin: 500 mg PO twice daily, or 1000 mg/d PO (extended-release preparation) for outpatients Covers pneumococcus, atypical pathogens, and H influenzae Nausea, vomiting, diarrhea, QT prolongation, dyspepsia (clarithromycin) Use as monotherapy only in patients without cardiopulmonary disease or modifying factors; otherwise, combine with a b-lactam Erythromycin is less expensive but is not recommended because of the need for more frequent dosing, more intestinal upset, and no coverage of H influenzae Bactericidal; interferes with peptidoglycan cross-linking and prevents formation of the bacterial cell wall Amoxicillin–clavulanate: 875 mg PO twice daily Ampicillin: 500–1000 mg PO 3 times daily Ampicillin–sulbactam: 1–2 g IV every 6 h Active against pneumococci and b-lactamase–producing H influenzae High doses (1 g 3 times daily) active against DRSP Anaphylaxis, rash, nausea, vomiting, diarrhea, phlebitis, seizures (high doses), hypokalemia (high doses), elevated liver enzymes, prolonged prothrombin time (especially if patient is using warfarin) Do not use alone in CAP Combine with a macrolide Bactericidal; interferes with bacterial DNA gyrase Kills bacteria in a concentrationdependent fashion Ciprofloxacin: 400 mg IV every 8 h Levofloxacin: 500–750 mg/d IV or PO Moxifloxacin: 400 mg/d IV or PO Active against P aeruginosa, atypical pathogens, and H influenzae Levofloxacin and moxifloxacin are the “respiratory quinolones,” with activity against DRSP, H influenzae, and atypical pathogens Seizures, hypersensitivity, photosensitivity, tendon rupture, nausea, vomiting, diarrhea, QT prolongation Only use ciprofloxacin in severe CAP Not always reliable against pneumococci, and should be combined with other agents if DRSP is possible If used in severe CAP, do not use as monotherapy Bacteriostatic; binds to 30S ribosomal subunit and interferes with bacterial protein synthesis 100 mg IV or PO twice daily Active against key bacterial and atypical pathogens Nausea, vomiting, diarrhea, photosensitivity Not always fully reliable against pneumococci Glycylcycline Tigecycline* (Tygacil) Macrolides Azithromycin Clarithromycin Penicillins Amoxicillin– clavulanate Ampicillin Ampicillin– sulbactam Quinolones Ciprofloxacin Levofloxacin Moxifloxacin Tetracyclines Doxycycline CAP = community-acquired pneumonia; DRSP = drug-resistant Streptococcus pneumoniae; IV = intravenously; MRSA = methicillinresistant Staphylococcus aureus; PO = orally. * Black box warning. © 2022 American College of Physicians In the Clinic Annals of Internal Medicine April 2022