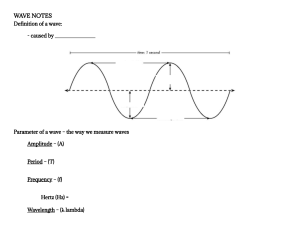
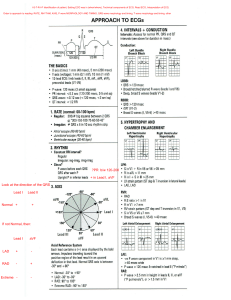
CV 468: EKG’s (a continuum) “That’s right sportsfan’s, Willy rides again…” Disclaimer: The information compiled in this powerpoint presentation do not express the views of anyone on payroll at VCOM nor do they reflect the views of the College itself. This information was put together for review and is intended as a high-yield review of EKG interpretation. This information is not complete therefore use this information merely as a supplement and at your own risk. George Mueller Review of Physiology SAN Conduction Phase 0 – upstroke, increased Ca conductance, inward Ca current Phase 3 – repolarization, increased K conductance, outward K current Phase 4 – slow depolarization, accounts for pacemaker activity, increased Na conductance, inward Na current (“funny current, If”) The PACEMAKER AVN Conduction The ionic basis for the AVN is the same as the SAN (see previous slide) Ventricular Conductance Phase 0 – upstroke, increased Na conductance, inward Na current Phase 1 – initial repolarization, increased K conductance, outward K current Phase 2 – plateau, transiently increased Ca + current (balances outward K) conductance, inward gNaCa Phase 3 – repolarization, decreased Ca conductance, increased K conductance, outward K current Phase 4 – resting membrane potential, inward and outward currents are balanced (IK1), approach K equilibrium This applies to the ventricles, atria, and the purkinje system. Refractory Periods Absolute – begins with the upstroke and ends after the plateau, reflects the time during which NO AP can be initiated Effective – slightly longer than ARP, period during which a CONDUCTED AP cannot be elicited Relative – period immediately after the ARP when repolarization is almost complete, AP CAN be elicited, but MORE than the usual inward current is required Put all this together Isoelectric line Waves, Intervals, Complexes, and Segments… P wave – atrial depolarization, does not include atrial repolarization (hidden in QRS) PR interval – beginning of P wave to beginning of Q wave (initial depolarization of ventricle), varies with conduction velocity of AVN (if decreased, PRI increases… heart block?) QRS complex – ventricular depolarization QT interval – beginning of Q wave to end of T wave, entire period of depolarization and repolarization of the ventricles ST segment – end of S ave to beginning of T wave, isoelectric, period when ventricles are depolarized R T wave – ventricular repolarization INTERVALS PRI – 0.12 to 0.20 sec QRS – 0.04 to 0.11 sec QTI – 0.3 to 0.4 sec (or no more than half to RRI) OR QTc = QT / √ RRI Positive P T Isoelectric Q S Negative EKG Interpretation (Basics) • • • • • RATE RHYTHM AXIS HYPERTROPHY INFARCTION IN THIS ORDER… and you cannot go wrong! 1) RATE INTRINSIC RATES SAN – 60 to 100 Atria – 60 to 80 AV JCT – 40 to 60 R wave on solid black line Pick an R wave that falls on a solid black vertical line and count until you reach the next one in sequence. Ventricles – 20 to 40 300 150 100 75 The next R wave falls just before the 75 mark, so the rate is just greater than 75, about 80 2) RHYTHM Is it REGULAR? Is the RRI at the same distance every time? THIS QUESTION BROUGHT TO YOU BY • • • • • • • 1st – check for P waves 2nd – check for QRS complex 3rd – look for a P wave before every QRS 4th – look for a QRS after every P wave 5th – check PR intervals (for AV blocks) 6th – check QRS intervals (for BBB) 7th – look for anything out of the ordinary, like extra beats This is the strip where you measure rate and rhythm If you are looking at a 12-lead EKG ALL of these measurement should be done on the long strip (at least 6 sec) at the bottom or top of the 12-lead EKG. You cannot accurately measure this from any of the shorter 3 second strips that comprise the 12 leads. More on the actual rhythms to come later… 3) AXIS Lead II follows the axis of the heart, thus it is usually the tallest and best lead to define all of this Clinical Tip: “White on Right, Smoke over Fire.” Electrical activity follows the anatomy of the heart. Look in Lead I & Lead aVF to determine if there is positivity (up) or negativity (down) in reference to the isoelectric line. NORMAL AXIS = Lead I & Lead aVF ↑ LEFT AXIS = Lead I ↑ & Lead aVF ↓ RIGHT AXIS = Lead I ↓ & Lead aVF ↑ EXTREME RIGHT AXIS = Lead I & Lead aVF ↓ + Ex-R LAD +I + Notice the Normal Axis follows LEAD II RAD Normal + aVF IT HELPS IF YOU CAN PICTURE THIS DIAGRAM ON A PT’S CHEST Lead I is UP (+) Lead aVF is UP (+) NORMAL AXIS Lead I is UP (+) Lead aVF is DOWN (-) CAUSES OF LAD LBBB / Left Anterior Hemiblock LVH Artificial Cardiac Pacing Inferior Wall MI (Right Coronary Artery) LEFT AXIS DEVIATION Hyperkalemia WPW (Right-sided accessory pathway) Pulmonary HTN (Right-sided heart failure) Tricuspid Atresia (Right side) ASD Lead I is DOWN (-) Lead aVF is UP (+) RIGHT AXIS DEVIATION CAUSES OF RAD RVH RBBB Anterior / Lateral Wall MI Normal Variant (peds, tall adults) Left Posterior Hemiblock VSD Key points about axis deviations 1 Vectors point AWAY from INFARCTIONS No blood supply, no electrical activity gets through necrotic tissue, therefore they act as stop signs and the electrical vectors and pointed in the opposing directions Key points about axis deviations 2 Vectors point TOWARDS the HYPERTROPHY More muscle means more electrical activity to depolarize the whole segment Axis Rotation (AKA – “R wave progression”) Think about where the V leads are. V1 is R parasternal border and they move in numerical progression to V6 which is L midaxillary. So if you think about the normal axis (vector) of the heart as going toward the L and wrapping around your chest to match the anatomy of the heart…the amplitude of the QRS should be increasing (more positive) from V1 to V6 (R to L). The TRANSITIONAL ZONE (NORMAL) is between V3 and V4 where the amplitude is most isoelectric (there is about equal positivity and negativity on either side of the isoelectric line) ---- THIS IS A ROTATION IN THE HORIZONTAL PLANE! The same rules apply in the horizontal plane as they do in the frontal plane (axis deviation) ---TOWARD HYPERTROPHY, AWAY FROM INFARCTION. RIGHTWARD ROTATION – RVH or a LATERAL WALL MI (Isoelectric leads moved to V1/V2) LEFTWARD ROTATION – LVH or an INFERIOR WALL MI (R coronary a) (Isoelectric leads moved to V5/V6) NORMAL EKG USE THIS AS A REFERENCE TOOL Each small block = 0.1mm Each small block horizontally = 0.04 sec (big block = 0.2 s) Each small block vertically = 0.1mV (big block = 0.5mV) 4) HYPERTROPHY RIGHT VENTRICULAR HYPERTROPHY (RVH) CRITERIA • R wave is bigger than the S wave in V1, but the R wave gets progressively smaller from V1 to V6 • S wave persists in V5 and V6 • Negative (discordant) T wave in V1 • RAD with wide QRS complex • Rightward rotation in the horizontal plane LOOK FOR A HUGE R WAVE IN V1 Enlarged RV adds more vectors to the right side 1) Rightward R wave Progression 2) Right Axis Deviation LEFT VENRICULAR HYPERTOPHY (LVH) Normally the S wave in V1 is very deep…with LVHyou have more electricity going down the patient’s left side (AWAY FROM +V1 electrode), therefore the S wave is even deeper in V1 Lead V5 is sitting directly over the LV, so there is more electricity going to the +V5 electrode…HUGE R WAVE IN V5 CRITERIA • (S wave in V1) + (R wave in V5) > 35mm • LAD with wide QRS complex • Leftward rotation of horizontal plane • Inverted T wave slants down gradually but up rapidly RIGHT ATRIAL HYPERTROPHY (RAH) CRITERIA Large, diphasic P wave with tall initial component (>2.5mm in Lead II and/or >1.5mm in V1) It is often “peaked” LEFT ATRIAL HYPERTROPHY (LAH) CRITERIA Large, diphasic P wave with a wide terminal component (often “notched”) and the P wave duration is > 0.12 sec in Lead II 5) Ischemia With ischemia the cells become more positive in their resting voltage (due to channel leakage of Ca++), making the subendocardium more positive; since the endocardium is further away from the precordial leads than the more negative myocardium. This is reflected as a ST depression. Ischemia – inverted T waves (typically symmetric inversion) – easier to see them in the V leads. 5) Injury & Infarction Injury Indicates the acuteness of an infarct…ST segment ELEVATION denotes injury. ST segment elevation (J point elevation) tells you that the MI is ACUTE Infarction 5) NON-Q-WAVE (Non-transmural) – ST segment elevation without pathologic Q waves 10) Q-WAVE (Transmural) – ST segment elevation with pathologic Q waves Pathologic Q Waves 1st deflection of QRS that is greater than 1/3 the entire QRS amplitude Q waves can be normal, they are just small and called ‘q’ waves ANTERIOR POSTERIOR INFERIOR LATERAL INFERIOR WALL MI ST ELEVATION – Leads II, III, aVF Reciprocal Changes??? RIGHT CORONARY ARTERY RCA SUPPLIES SAN/AVN – BRADYCARDIA? ANTEROLATERAL WALL MI ST Elevation – Leads I, aVL, V1-V6 Anterior Component – V1-V4 Lateral Component – I, aVL, V5, V6 LEFT CORONARY A & BRS POSTERIOR WALL MI We have no leads on the posterior thorax, therefore all you will see is the reciprocal change in leads V1 (mostly) but up through V3 possibly…what is reciprocal change? ST segment DEPRESSION. Posterolateral branch of RCA (75%) or Distal Left Circumflex (25%) MIRROR TEST???? MI THERAPY • • • • • • • • • MONA (Morphine, O2, NTG, ASA) IV Fluids Thrombolytics (tPA) Heparin Plavix Metoprolol Enzymes CXR Call the Cath Lab / Cardiologist ISCHEMIA THERAPY NTG Beta-blockers Plavix (Clopidrogel) Heparin (UFH or LMWH) Glycoprotein IIb/IIIa Inhibitor Cardiac Cath PERICARDITIS Diffuse ST elevation BUNDLE BRANCH BLOCKS RIGHT BBB - the right ventricular firing is late so R-R’ is in V1 LEFT BBB - the left ventricular firing is delayed so R-R’ is in the V6 CRITERIA • Wide QRS Complex > 0.12 sec must be present • RBBB – V1/V2 R-R’ • LBBB – V5/V6 R-R’ RBBB LBBB Also see HUGE DEEP S waves in V1-3 HYPERKALEMIA CRITERIA 2) PEAKED T WAVES 3) Flat P waves 4) Wide QRS Etiology – renal failure, acidosis, rhabdo TREATMENT 2) Ca Chloride / Gluconate 3) Glucose 4) Insulin 5) Albuterol 6) Kaexalate 7) NaHCO3 EXTREME HYPERKALEMIA – sinusoidal waves CRITERIA 2) Flat to inverted T waves 3) Prominent U waves TREATMENT Ummm…K+ (KCl) HYPOKALEMIA RHYTHMS SINUS/ATRIAL RHYTHMS Normal Sinus Rhythm Regular rhythm P:QRS = 1:1 Rate 60-100 Rate < 60 TX – ATROPINE, PACING, EPI, DOPAMINE Rate > 100 Irregular rhythm but P waves are of different morphology and the PRI varies depending on where/when it fires Looks like NSR but is slightly irregular (all else applies) Arrest – this would be an escape beat (jct/vent) SAN fires but it can’t exit the SAN Sinus Exit Block/Arrest SVT Rate 150-250, regular, narrow QRS TX – ADENOSINE, DILT Flutter waves (sawtooth / picket fence), can be reg/irreg, atrial rate usually 300 (ventricular rate 150 for 2:1) TX – ADENOSINE, DILT, AMIO, VERAPAMIL, DIG Irregularly-irregular, QRS is normal Anything that is irregularly-irregular is AFIB until proven otherwise Irregular, rate 100-250, 2 or more ectopic P waves with different morphologies, PRI vary, QRS is normal TX - DILTIAZEM AKA - PSVT Sinus rhythm interrupted by a period of SVT Wolff Parkinson White CRITERIA 2) QRS < 0.10 sec 3) PRI < 0.12 sec 4) Delta Wave TX – ADENOSINE, PROCAINAMIDE DO NOT GIVE CALCIUM CHANNEL BLOCKERS If you do this you will block the inherent conductance of the AVN which is fine, it just so happens that the extranodal pathway (Bundle of Kent) is faster and thus conducts before the normal AVN. If you do this you set the patient up for nasty rythms (VF/VT, etc) LONG QT SYNDROME QTc = QT / √RR The QTI should not be more than ½ the RR TX – BETA-BLOCKERS AVN BLOCKS PRI > 0.20 sec PRI gets progressively longer until a P wave gets blocked thru the AVN QRS? Going, going, gone… PPI are regular, PRI can be normal/long, but a P wave will get blocked QRS? QRS? TX (2°AVBII / 3°AVB) – PACING, If brady, follow that algorithm PPI normal, RRI normal, but there are no P’s associated with QRS complexes…atria not talking to ventricles P in QRS JUNCTIONAL RHYTHMS Junctional means the start point in the AV junction (not the SAN)…therefore there are no P waves OR retroconducted P waves (inverted)…and they can occur anywhere (before, during, or after the QRS) TX – ADENOSINE, DILT Junctional Tachycardia Normal inherent rate is 40-60, but by definition of a rate between 60-100 is normal, so it is called ACCELERATED, and if the rate is greater than 100, it is called TACHYCARDIC PREMATURE BEATS Bigeminy – there is 1 PVC for every normal beat Trigeminy – 1 per 2 Quadrigeminy – 1 per 3 By definition these are simply ectopic beats that occur early…the cadence is not affected as you see normal beat after the premature beat is in line where it should have come if everything was normal ESCAPE BEATS Atrial These are usually benign, unless the patient is symptomatic. They occur after a long hesitation (pause) and then there is a spontaneous discharge from the corresponding tissue. It must occur later in the rhythm than expected Junctional VENTRICULAR RHYTHMS USUALLY BAD!!! May be irregular, wide and bizarre QRS complexes, rate 150-250 (pulses? mono/polymorphic?) TX – AMIODARONE, SYNC CARDIOVERSION (PULSE), DEFIBRILLATION (PULSELESS) Random electrical activity (coarse/fine?) “Twisting of the Points,” often preceded by a long QTI TX – MgSO4 Purkinje cell discharge at their intrinsic rate of 20-40 (if faster, can be accelerated IVR), wide/bizarre AKA – “dead” TX – PACING, ATROPINE, EPI, or CALL IT MISCELLANEOUS If the P wave hits the AVN during the absolute refractory period, the signal will not go any further…no P gets through means no QRS Widening and distortion of the QRS, short PRI usually…these are typically just smaller in amplitude than the normal conducted rhythms (this is just one example) R on T Phenomenon T wave here R wave here Usually results in very bad rhythms…VF/VT PACED RHYTHMS Atrial Pacemaker Look for the pacing spikes at the onset of the P wave or QRS. Make sure there is a T wave to follow the QRS to ensure repolarization (especially important for external pacing). Ventricular Pacemaker CPR PEA TACHY CP BRADY PEA