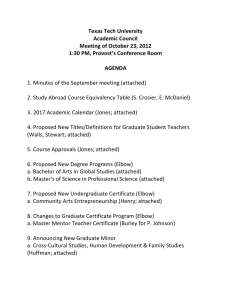
Shoulder & Elbow. ISSN 1758-5732 E INVITED REVIEW Management of the post-traumatic stiff elbow Odhrán Murray, Duncan Macdonald, Tom Nunn, Jane McEachan & Lech Rymaszewski Department of Trauma and Orthopaedics, Glasgow Royal Infirmary, Glasgow, UK ABSTRACT Received Received 31 October 2011; accepted 31 October 2011 Keywords Elbow, post-traumatic, stiffness, arthroylsis, contracture, ankylosis Conflicts of Interest None declared Correspondence Lech Rymaszewski, Department of Trauma and Orthopaedics, Glasgow Royal Infirmary, Castle Street, Glasgow G4 0SF, UK. Tel.: 0141 211 5334. E-mail: omurray32@gmail.com Restriction of elbow motion after trauma is a well-recognized problem. Most cases improve with time and use, although significant stiffness may persist and interfere with function. Over the last 20 years, surgical procedures have been reported that can safely improve the range of motion in most patients. A wide variety of different operative procedures and postoperative regimes have been described, with comparable results. Surgical techniques range from arthroscopic procedures, through increasingly extensive open releases, up to those requiring a dynamic external fixator to provide stability. Postoperative passive stretching with manipulation or splinting is often advocated, although evidence of effectiveness is lacking. We provide an overview of the current literature, and propose a new surgical guide to aid with the management of stiff elbows. DOI:10.1111/j.1758-5740.2011.00167.x INTRODUCTION Stiffness is the most common clinical problem after elbow trauma, in contrast to instability, which is comparatively rare. Loss of extension of up to 30◦ is the most common outcome, although this is usually well tolerated, with automatic compensation by moving closer to the object. By contrast, loss of flexion significantly affects function if the hand cannot reach the head and mouth, and this restriction cannot be overcome (Fig. 1). Most activities of daily living can be performed with a 100◦ arc of movement of 30◦ to 130◦ of flexion and 50◦ to 50◦ of pronation/supination [1]. Other causes of stiffness as a result of osteoarthritis, inflammatory arthritis, neuromuscular and congenital disorders and their management are beyond the scope of the present review. This review focuses on the post-traumatic elbow stiffness, and presents a surgical guide for performing arthrolysis. Aetiology The pathoanatomy of elbow stiffness has been classified into ‘intrinsic’ and ‘extrinsic’ conditions [2]. Intrinsic refers to intra-articular incongruity or adhesions, whereas extrinsic refers to heterotopic ossification or contracture of the caspulo-ligamentous structures of the elbow joint. However, because significant post-traumatic stiffness usually follows intra-articular fractures, which frequently have both intrinsic and extrinsic features, this classification system is of limited value in the management or prognosis of these cases. Natural history Restriction of motion is almost inevitable immediately after elbow trauma, although, in the vast majority of cases, movement spontaneously improves with time and use, until a functional range is achieved (i.e. the natural history is usually benign). Unlike 38 the shoulder, which can be effectively held by the side without impairing hand function, a fixed elbow is impractical. Most patients, therefore, will mobilize their elbow early after trauma, simply with the aim of performing necessary everyday tasks. CLINICAL EVALUATION AND INVESTIGATIONS History. A careful history is essential to establish an accurate diagnosis and to understand the individual patient’s problems and expectations. Information obtained and recorded should include: • • • • • • • Age, occupation and hand dominance. The history of injury, subsequent management and complications. Duration of stiffness and whether static. Degree of stiffness: impact on occupation, activities of daily living and recreational pursuits. Pain: qualify the nature of the pain (e.g. end of range, constant, activity related, etc.) and quantify in various scenarios (e.g. using a visual analogue scale at rest/at night/during lifting/performing tasks with repeated movements). Ulnar neuropathy: pain, weakness/clumsiness, paraesthesia or altered sensation, which may need to be addressed at surgery. Locking/mechanical symptoms: as a result of loose bodies. Patient reported outcome measurements (PROMs) PROMs are very useful to evaluate and monitor progress (e.g. the Disabilities of the Arm, Shoulder and Hand or Oxford scores). Evaluation of pain is important because it is well recognized as having a very strong influence on both physician-rated and patientrated quantitative measures of elbow function. It is important to © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 E Murray et al. Management of the post-traumatic stiff elbow (A) (B) Fig. 2 Positive ‘grip and grind’ test. Pain on pronation/supination when loading the radio-capitellar joint (e.g. turning a stiff handle) can be confirmed with axial loading by clenching the fingers during forearm rotation. Fig. 1 (A) Loss of extension of up to 30◦ is common after elbow trauma, although is usually well tolerated. The main effect is to limit reach, by a few centimetres, distance y, with automatic compensation by moving slightly closer to the object. (B) By contrast, a 30◦ loss of flexion from 130◦ to 100◦ greatly affects function because the hand cannot reach the head and mouth: distance x is three times greater than distance y and this restriction cannot be overcome. appreciate that pain may be strongly influenced by psychosocial aspects. Doornberg et al. therefore recommend evaluation of pain separately from objective measures of elbow function in physicianbased elbow ratings [3]. Examination Inspection may reveal deformity, muscle wasting, previous scars, prominent metalwork or signs of inflammation. The elbow is largely subcutaneous and its anatomy can be palpated intimately for abnormalities. If a patient is being assessed for surgery, the range of motion (ROM) should be accurately assessed on serial visits, preferably with a long-arm goniometer [4] by the same examiner, to ensure that improvement is not gradually occurring. Hard endpoints ± pain at the extremes of motion indicate a bony block, whereas soft endpoints are indicative of soft-tissue contracture. Restriction of forearm rotation and/or ‘grip and grind’ pain at the radiocapitellar joint elicited by axially loading and rotating the forearm (Fig. 2) is usually the result of a previous radial head fracture, which may need to be excised at surgery. Investigations Routine anteroposterior and lateral X-rays are the mainstay of imaging. Osteophytes, loose bodies, heterotopic ossification, malunion/non-union and erosion are easily identified on a plain X-ray. Although computed tomography and magnetic resonance imaging are increasingly being used to investigate complex contractures, the actual surgical procedure usually remains unaltered. The initial approach is determined by the original injury and subsequent surgery, including the presence of metalwork, and the definitive pathology only determined at operation. Occasionally, imaging may be helpful to establish the relationship of neurovascular structures with heterotopic bone. Nerve conduction studies should be undertaken in the presence of neurological dysfunction. TREATMENT Conservative Early, active mobilization is essential for preventing post-traumatic elbow stiffness. Most elbow injuries are stable, and spontaneously achieve a functional ROM through early mobilization and resumption of daily activities within the limits of discomfort. Most unstable injuries can be similarly mobilized after stabilization with a variety of techniques, including internal fixation, soft-tissue repair, radial head (or occasionally total elbow) replacement or dynamic external fixation. Immobilization for more than 2 weeks is rarely required, even after closed reduction of dislocated elbows demonstrating instability during examination under anaesthesia [5]. Prolonged immobilization should be avoided (>3 weeks) because the chances of developing significant stiffness are increased [6,7]. Physiotherapy is often routinely prescribed, although this frequently only consists of reassurance and advice regarding active exercises. Passive stretching with manipulation or a variety of © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 39 E Murray et al. Management of the post-traumatic stiff elbow splints have been promoted [8], although this remains controversial. Splinting regimens include: • Static splints. Resting splints can be manufactured to maintain the elbow at the end-point of extension and/or flexion, and are used during the rehabilitation period when resting, especially at night. The patient can then start to mobilize from the end of range position in the morning rather than spend several hours getting back to this point. • Turnbuckle splints. These have been designed on the principle of incremental displacement, which causes stress relaxation of the soft tissues through plastic deformation [9]. A major disadvantage is that the patient has to wear a splint for a significant period of time during the day and night, thus restricting normal function, and possibly the ability to work for several months. Gelinas et al. recommended splinting for 18 hours out of 22 hours, although many of their patients could not fully cooperate with this rigorous regime [10]. • Dynamic hinged splints. These splints use adjustable springs to apply constant load, initially applying very low forces, which are gradually increased within the limits of the patient’s symptoms. In theory, the soft tissues can be stretched very gently over a maximum period of time, avoiding pain and spasm. However, evidence to the benefit of this device in the elbow is very limited. There is considerable variation in the degree of force applied to the elbow during passive stretching, ranging from rapid application of significant force (i.e. a manipulation) to a splint applying a very small force over a prolonged period. The problem is that this method may produce soft-tissue tearing, or at least plastic deformation of the soft tissues, to produce greater motion. Caution is required to avoid provoking pain, inflammation and muscle spasm, which are all counterproductive to effective rehabilitation and may result in increased stiffness. Elbow splints tend to slip down and require constant adjustment to allow unconstrained elbow flexion in the correct axis. Passive stretching techniques can therefore be expensive, labour intensive and time consuming for the patient. In addition, genetic factors must influence the tendency to scar, although the effect cannot be quantified as yet. Clinical measurement, even with a long-arm goniometer, has a significant inter-observer error band of 7◦ of extension and 6◦ of flexion [4], which raises the possibility of some reports overstating claims of effectiveness of a particular treatment or subsequent arthrolysis. Only small cohort series reporting good results with passive stretching exist, with no control groups to compare to the improvement with natural history. The evidence for such modalities adding value over active movement alone is therefore weak, although patients often choose a particular regime according to their own preferences and recommendations of others. Surgical Indications and contraindications. Surgery should be considered in the presence of significant stiffness and functional limitation that is not improving after at least 6 months of conservative 40 management. There are few absolute contraindications to arthrolysis as long as the patient is fit enough to undergo surgery and has been fully appraised of the potential risks and benefits. A functional hand is essential because the elbow is merely a link in a lever system that positions the hand in space. Patients who have had a neurological injury and lack sufficient power of elbow flexion and extension are unlikely to benefit from arthrolysis. Surgical release of post-traumatic stiff elbows was rarely performed until approximately 15 years to 20 years ago because the procedure was generally considered to be ineffective in restoring motion. However, subsequent to numerous reports of successful procedures [11–40], arthrolysis is now regarded as a reliable, rewarding, evidence-based operation, with low risk of complications. The results in the recent literature are broadly similar, reporting that elbow motion improves in almost all patients, with a mean gain of approximately 50◦ , and that the majority achieve the functional arc of 30◦ to 130◦ [20–39]. The key principles common to almost all studies are the achievement of as much movement as possible at surgery and early motion postoperatively, which requires adequate pain control (Fig. 3). Arthroscopic surgery Arthroscopy of the elbow has been gaining popularity and there are increasing reports of arthrolysis being performed using this technique. Advocates of this technique consider that it offers the advantages of improved visualization of the anatomy, minimal incisions, reduced pain, shorter hospital stay and accelerated rehabilitation [41–43]. It does, however, have several disadvantages. Early reports frequently show evidence of iatrogenic injury to neurovascular structures around the elbow [44–46]. The ulnar nerve is at particular risk because it passes through the cubital tunnel and in close proximity to the capsule of the medial joint line. Within this tightly confined space, it is at risk from shavers, debriders, increased pressure and thermal injury [43]. Other nerves that have been damaged include the radial, median and the posterior and anterior interosseous nerves [44,47]. In addition, there are limitations to arthroscopy, such as the inability to remove metalwork, perform ulnar nerve release or transposition, and Fig. 3 The key factors for a successful arthrolysis: achievement of as much movement as possible at surgery and early motion postoperatively, which requires adequate pain control. Intra Op, intra-operative; Post Op, postoperative. © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 E Murray et al. Management of the post-traumatic stiff elbow difficulty in dealing with heterotopic ossification, joint incongruity or intra-articular adhesions. O’Driscoll classified contractures as simple or complex [48]. Simple contractures have normal anatomy and a mild/moderate contracture (≤ 80◦ ), and had no or minimal prior surgery, no prior ulnar nerve transposition, no or minimal metalwork or heterotopic ossification. O’Driscoll emphasizes that most post-traumatic elbow stiffness fail to meet one or more of these criteria and arthroscopic release of complex contractures should only be performed by surgeons with substantial experience in this field in view of the high likelihood of complications [48]. Ulnar neuritis is common in association with elbow contracture either pre- or postoperatively once elbow flexion improves [27,30] and should be addressed with an ulnar nerve release via an open approach. Although rehabilitation is potentially quicker after arthroscopy, there is little evidence of improved results, with a possibility of less improvement compared in open surgery [49], unless performed by an expert. Open arthrolysis The primary aim of arthrolysis is to achieve as much ‘on-table’ movement as possible; ideally full because the final ROM is likely to be slightly less and never more than achieved at surgery. Maximum ROM is achieved by using an extensile approach, using supplementary incisions, if necessary. A variety of open surgical approaches have been reported [20–40], each with specific advantages and disadvantages. The specific approach is determined by the pre-operative assessment of the pathology and the personal preference of the surgeon. The exact location and extent of any soft-tissue contracture, bony impingement, joint incongruity and intra-articular adhesions are defined at surgery. All constraints must be addressed with an extensile approach until, ideally, a full range of congruous movement is achieved. A direct posterior approach, taking care to raise thick, viable skin flaps, will give access to both the medial and lateral ‘columns’. Alternatively, a lateral skin incision will also allow adequate exposure and can be supplemented by a small medial incision to decompress the ulnar nerve and, if required, release the posterior band of the medial collateral ligament. We have recently introduced a new surgical guide [50] EFG system (‘extension, flexion, grip and grind’) to help identify and address the pathology in a sequential manner (Fig. 4), as well as record it in a systematic way that allows comparison between different series. Access to the anterior compartment is usually gained through a lateral ± medial approach, according to the preference of the surgeon. Contraction of the anterior capsule is almost universally present and requires release (‘E1’), so that a finger may easily be permitted beneath the lax anterior tissues of the fully extended elbow. The anterior capsule can simply, safely and effectively be released from the distal humeral ± its coronoid attachment as necessary. By contrast, partial or complete capsulectomy risks radial nerve injury because it passes anterior to the radial head at the lateral edge of brachialis, separated only by a thin layer of fat [51] and offers no advantage to capsulotomy alone. If restriction to full extension persists, bony impingement in the posterior compartment must be addressed (‘E2’). Access may be gained laterally ± medially under the triceps or by splitting the triceps. Olecranon tracking within its fossa is assessed, and osteophytes around the olecranon and fossa removed. (Removal of 6 mm of osteophyte from the olecranon/coronoid tips will improve extension/flexion by 30◦ respectively; millimetres become centimetres). Additional scar tissue, loose bodies and callus may be removed from the distal humerus to deepen and widen the fossa to accept the olecranon in terminal extension. Finally, if a satisfactory ROM cannot be achieved, a complete release of the lateral ligament allows the joint to be subluxed with supination and any intra-articular pathology addressed (‘E3’). It is safe to sublux the elbow joint [50] provided that the soft tissues are reattached to the lateral condyle. Adhesions are debrided and articular congruity restored by contouring with a high-speed burr. Motion should be then be checked by fully pronating the forearm to stabilize the elbow, and ensuring a full, smooth and congruous arc, as even minor impingement(s) tend to be unforgiving. Limitations to flexion are addressed in a similar manner. Because the anterior compartment is opened before the posterior compartment, bony impingement is addressed first (‘F1’). Osteophytes and abnormal bone are excised from the tip of the coronoid with care. Excessive removal of the true coronoid, especially if the radial head has also been excised, may result in instability. The coronoid fossa and supra-capitellar region are cleared in a similar fashion to the olecranon fossa, as noted above. Further gains in flexion are achieved by releasing posterior soft tissue contractures (‘F2’). The posterior capsule is released from its origin at the distal humerus and olecranon fossa. Additionally, the posterior band of the medial collateral ligament may restrict flexion. The posterior band forms part of the cubital tunnel floor and can only be accessed by ulnar nerve decompression and gentle mobilization, or formal transposition. After bony and soft tissue correction of the anterior and posterior compartments, intra-articular limitations to flexion (‘F3’) are addressed simultaneously with extension (‘E3’), with subluxation of the joint after a complete lateral ligament release. Restriction of forearm rotation or a positive pre-operative ‘grip and grind’ test is addressed by radial head excision (‘G1’). Debridement of the radial head alone may result in adhesions and/or maltracking with a poor outcome. If forearm rotation remains limited, stripping radial neck adhesions may on occasion be successful (‘G2’). A proximal radioulnar synostosis may be excised with the radial head intact (‘G3a’) or absent (‘G3b’). Removal of scar tissue or bone between the radial tuberosity and ulna in the absence of the radial head carries the highest incidence of recurrent stiffness because the supinator tends to draw the radius and ulna together. Ulnar nerve management. A cubital tunnel release is routinely performed to formally decompress the ulnar nerve if a medial approach is used. Access to the posterior band of the medial collateral ligament and posterior capsule is gained through the bed of the ulnar nerve. It is important to retain fascial attachments of the fat to the medial epicondyle aiming to prevent subluxation of the nerve postoperatively. Extension of the medial approach for access to the © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 41 E Management of the post-traumatic stiff elbow Murray et al. Fig. 4 EFG surgical guide. E, Extension; F, Flexion; G, Grip and Grind. The pathology responsible for elbow stiffness is addressed sequentially with an extensile approach until, ideally, a full range of motion has been achieved. 42 © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 E Murray et al. Management of the post-traumatic stiff elbow anterior capsule on the medial side can be performed by elevating a flap of brachialis/pronator teres, which will allow visualization of the anterior capsule, anteromedial humeroulnar joint and coronoid process. Transposition of the ulnar nerve is performed if the bed of the ulnar nerve is distorted or the nerve subluxes on flexion. Interpositional arthroplasty. Interposition arthroplasty involves resurfacing the elbow joint with an allograft, such as achilles tendon or fascia lata. The distal humeral articular surfaces are deepened and contoured after an extensive soft-tissue release. A dynamic external fixator is then applied to protect the graft for approximately 4 weeks [52]. Interpositional arthroplasty is considered to be useful in the younger patient with more than 50% loss of the articular surface, although significant complications have also been reported, especially instability [33,52]. There is no evidence that interpositional arthroplasty adds value over arthrolysis alone in terms of ROM, functional scores or pain relief at midterm follow-up at 4 years and 5 years [23,33,52]. Total elbow replacement (TER) TER should be viewed as a salvage procedure, which is only to be used in the older, less active patients. The techniques of TER are beyond the scope of the present review, although a linked prosthesis is recommended in the presence of severe deformity, poor bone stock or instability. Mansat and Morrey demonstrated that improvements in ROM can be obtained using TER, although with high complications rates (seven of thirteen), including two deep infections [53]. Implant survival rates for TER in the stiff elbow are worse than those for rheumatoid arthritis, especially in younger patients, with 75% of failures occurring in those aged <65 years [54]. REHABILITATION There is wide agreement that early mobilization after elbow arthrolysis is important. This requires adequate pain control and a stable elbow. If there is a risk that the elbow will be unstable postoperatively, then a dynamic external fixator can be used for 1 weeks to 2 weeks until the elbow regains stability. In the immediate postoperative period, the pain can be considerable and will inhibit early movement unless adequately controlled. Brachial plexus blockade allows prolonged analgesia when administered continuously through a catheter for 48 hours to 72 hours [55]. Adjuvant pain control can be delivered via a patient-controlled analgesia system with opiates. These methods have been shown to be very effective, although they require a 24-hour team approach to pain control. Whenusingabrachialplexusblockforpostoperativepaincontrol, a degree of motor blockade often results, and active movement is not possible. Continuous passive movement (CPM) is an excellent way of ensuring early mobilization of the elbow. A major benefit may be psychological because the patient can see their joint moved painlessly through an improved arc of movement. However, there is little evidence that the use of CPM improves the overall outcome. There can be no further gain in ROM from that obtained on the operating table. Physiotherapy is not considered to be essential in the recovery period, apart from offering support and reassurance to patients that it is safe to use their arm in activities of daily living. On discharge from hospital, the ROM is likely to be less than achieved in theatre as a reselt of swelling restricting the end of range movement. Passive stretching has been used by some surgeons, although there is no evidence that it alters the eventual outcome; the most important factor is the ROM obtained at surgery. In a series by Higgs et al., 70 patients underwent open arthrolysis followed by inpatient CPM with brachial plexus blockade for 48 hours [40]. No passive stretching was used, and the arc of movement continued to improve over the next 12 months by a mean of 40◦ compared to the pre-operative measurement. These results are similar to other series that use passive stretching. Other aids to rehabilitation include static, dynamic and turnbuckle splints; however, there is little evidence of any benefit, with similar risks to splinting as outlined above. OUTCOME/COMPLICATIONS OF OPEN ARTHROLYSIS Arthrolysis improves the range of elbow movement between 21◦ and 66◦ [50,51,56], as well as health status and disability scores. However, the degree of improvement does not necessarily correlate with the improvement in ROM because final pain levels are an important predictor of general health status and disability scores in this population [50,51,56]. Reports of complications from open arthrolysis vary from 0% to 44%, although most of the complications reported are relatively minor [18,22,24–36,50,51]. Wound infection, dehiscence, haematoma and seroma are the commonest problems and are more likely in more complex cases. Patient disappointment in their gain in movement may occur, although this should be minimized with adequate pre-operative information. Limited further gain may be obtained with a revision arthrolysis, although lower outcome and functional scores have been reported [28,29]. Ulnar neuritis can occur after improvement in flexion is obtained [27,30]. It has been suggested that asymptomatic ulnar compression may be present prior to elbow release and, with the sudden increase in elbow flexion, tension on the tethered nerve can give rise to clinical neuropathy. Although there is no conclusive evidence, routine decompression of the ulnar nerve is recommended if pre-operative flexion is less than 120◦ [48]. Instability rarely occurs after arthrolysis after complete release of the lateral ligament. If subluxation occurs, a dynamic external fixator will restore stability and allow mobilization. CONCLUSION Most patients will achieve a functional ROM within 9 months to 12 months after elbow trauma, although, if significant stiffness with restriction of function persists, surgery may be indicated. The simplest, safest surgical approach should be chosen that allows access to the soft tissue and bony pathology for release/debridement. The EFG surgical guide provides a simple method of addressing the stiffness in a systematic manner and allows grading of the pathology. There is little evidence of added value with arthroscopic surgery or interposition arthroplasty © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 43 E Murray et al. Management of the post-traumatic stiff elbow compared to open surgery. The choice of skin incision(s) will vary according to previous surgery and the personal preference of the surgeon. A lateral surgical approach is safe and reliable and a medial approach can be added to address medial side pathology, as well as release/transposition of the ulnar nerve. Postoperative pain control is imperative to allow early mobilization. Functional improvement in ROM is usually obtained and maintained in the medium term. References 1. Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg (Am) 1981; 63:872–7. 2. Morrey BF. Post-traumatic contracture of the elbow: operative treatment including distraction arthroplasty. J Bone Joint Surg (Am) 1990; 72A:601–18. 3. Doornberg JN, Ring D, Fabian LM, et al. Pain dominates measurements of elbow function and health status. J Bone Joint Surg Am 2005; 87:1725–31. 4. Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJ. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg 1988; 7:573–80. 5. Josefsson PO, Gentz CF, Johnell O, Wendeberg B. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. A prospective randomized study. J Bone Joint Surg Am 1987; 69:605–8. 6. Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Simple dislocation of the elbow in the adult. Results after closed treatment. J Bone Joint Surg Am 1988; 70:244–9. 7. Protzman RR. Dislocation of the elbow joint. J Bone Joint Surg Am 1978; 60:539–41. 8. Bhat AK. Static progressive stretch therapy with turn buckle orthosis in the treatment of elbow stiffness: a prospective clinical study. J Orthop Surg 2010; 18:76–9. 9. Green DP, McCoy H. Turnbuckle orthotic correction of elbow flexion contractures after acute injuries. J Bone Joint Surg Am 1979; 61:1092–5. 10. Gelinas JJ, Faber KJ, Patterson SD, King GJ. The effectiveness of turnbuckle splinting for elbow contractures. J Bone Joint Surg Br 2000; 82:74–8. 11. Urbaniak JR, Hansen PE, Beissinger SF, et al. Correction of posttraumatic flexion contracture of the elbow by anterior capsulotomy. J Bone Joint Surg (Am) 1985; 67:1160–4. 12. Morrey BF. Post-traumatic contracture of the elbow: operative treatment including distraction arthroplasty. J Bone Joint Surg (Am) 1990; 72:601–18. 13. Husband JB, Hastings H. The lateral approach for operative release of post-traumatic contracture of the elbow. J Bone Joint Surg (Am) 1990; 72:1353–8. 14. Gates HS, Sullivan FL, Urbaniak JR. Anterior capsulotomy and continuous passive motion in the treatment of post-traumatic flexion contracture of the elbow: a prospective study. J Bone Joint Surg (Am) 1992; 74:1229–34. 15. Amillo S. Arthrolysis in the relief of post-traumatic stiffness of the elbow. Int Orthop 1992; 16:188–90. 16. Boerboom AL, De Meyier HE, Verburg AD, et al. Arthrolysis for post-traumatic stiffness of the elbow. Int Orthop 1993; 17:346–9. 17. Modabber MR, Jupiter JB. Reconstruction for post-traumatic conditions of the elbow joint. J Bone Joint Surg (Am) 1995; 77:431–46. 18. Cohen MS, Hastings H II. Post-traumatic contracture of the elbow: operative release using a lateral ligament sparing approach. J Bone Joint Surg (Br) 1998; 80:805–12. 19. Mansat P, Morrey BF. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg (Am) 1998; 80:1603–15. 44 20. Wada T, Ishii S, Usui M, et al. The medial approach for operative release of post-traumatic contracture of the elbow. J Bone Joint Surg (Br) 2000; 82:68–73. 21. Olivier LC, Assenmacher S, Setareh E, et al. Grading of functional results of elbow joint arthrolysis after fracture treatment. Arch Orthop Trauma Surg 2000; 120:562–9. 22. Bae DS, Waters PM. Surgical treatment of posttraumatic elbow contracture in adolescents. J Pediatr Orthop 2001; 21:580–4. 23. Stans AA, Maritz NGJ, O’Driscoll SW, et al. Operative treatment of elbow contracture in patients twenty-one years of age or younger. J Bone Joint Surg (Am) 2002; 84:382–7. 24. Marti RK, Kerkhoffs GMMJ, Maas M, et al. Progressive surgical release of a posttraumatic stiff – elbow technique and outcome after 2–18 years in 46 patients. Acta Orthop Scand 2002; 73:144–50. 25. Yamamoto K, Shishido T, Masaoka T, et al. Clinical results of arthrolysis using postero-lateral apprach for post- traumatic contracture of the elbow joint. Hand Surg 2003; 8:163–72. 26. Aldridge JM III, Atkins TA, Gunneson EE, Urbaniak JR. Anterior release of the elbow for extension loss. J Bone Joint Surg (Am) 2004; 86:1955–60. 27. Park MJ, Kim HG, Lee JY. Surgical treatment of post-traumatic stiffness of the elbow. J Bone Joint Surg (Br) 2004; 86:1158–62. 28. Gosling T, Blauth M, Lange T, et al. Outcome assessment after arthrolysis of the elbow. Arch Orthop Trauma Surg 2004; 124:232–6. 29. CikesA, JollesBM, FarronA. Open elbow arthrolysis for posttraumatic elbow stiffness. J Orthop Trauma 2006; 20:405–9. 30. Ring D, Adey L, Zurakowski D, et al. Elbow capsulectomy for posttraumatic elbow stiffness. J Hand Surg (Am) 2006; 31:1264–71. 31. Tan V, Daluiski A, Simic P, et al. Outcome of open release for post-traumatic elbow stiffness. J Trauma 2006; 61:673–8. 32. Gausepohl T, Mader K, Pennig D. Mechanical distraction for the treatment of posttraumatic stiffness of the elbow in children and adolescents. J Bone Joint Surg (Am) 2006; 88:1011–21. 33. Mader K, Koslowsky TC, Gausepohl T, et al. Mechanical distraction for the treatment of posttraumatic stiffness of the elbow in children and adolescents. Surgical technique. J Bone Joint Surg (Am) 2007; 89(Suppl.):26–35. 34. Sharma S, Rymaszewski LA. Open arthrolysis for post-traumatic stiffness of the elbow: results are durable over the medium term. J Bone Joint Surg (Br) 2007; 89:778–81. 35. Brinsden MD, Carr AJ, Rees JL. Post-traumatic flexion contractures of the elbow: operative treatment via the limited lateral approach. J Orthop Surg Res 2008; 10:39. 36. Nolla J, David Ring D, Lozano-Calderon S, et al. Interposition arthroplasty of the elbow with hinged external fixation for posttraumatic arthritis. J Shoulder Elbow Surg 2008; 17:459–64. 37. Ruch DS, Shen J, Chloros GD, et al. Release of the medial collateral ligament to improve flexion in post- traumatic elbow stiffness. J Bone Joint Surg (Br) 2008; 90:614–18. 38. Kulkarni GS, Kulkarni VS, Shyam AK, et al. Management of severe extra-articular contracture of the elbow by open arthrolysis and a monolateral hinged external fixator. J Bone Joint Surg (Br) 2010; 92:92–7. 39. Park MJ, Chang MJ, Lee YB, Kang HJ. Surgical release for posttraumatic loss of elbow flexion. J Bone Joint Surg Am 2010; 92:2692–9. 40. Higgs ZCJ, Danks BA, Sibinski M, et al. Elbow arthrolysis for posttraumatic stiffness. J Bone Joint Surg (Br), in press. 41. Kelly EW, Bryce R, Coghlan J, et al. Arthroscopic debridement without radial head excision of the osteoarthritic elbow. Arthroscopy 2007; 23:151–6. 42. Ball CM, Meunier M, Galatz LM, et al. Arthroscopic treatment of posttraumatic elbow contracture. J Shoulder Elbow Surg 2002; 11:624–9. 43. Kim SJ, Shin SJ. Arthroscopic treatment for limitation of motion of the elbow. Clin Orthop 2000; 375:140–8. 44. Kelly EW, Morrey BF, O’Driscoll SW. Complications of elbow arthroscopy. J Bone Joint Surg Am 2001; 83:25–34. © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 E Murray et al. Management of the post-traumatic stiff elbow 45. Haapaniemi T, Berggeren M, Adolfsson L. Complete transection of the median and radial nerves during arthroscopic release of posttraumatic elbow contracture. Arthroscopy 1999; 15:784–7. 46. Dumonski ML, Arciero RA, Mazzocca AD. Ulnar nerve palsy after elbow arthroscopy. Arthroscopy 2006; 22:577.E1–3. 47. Schneider longterm results of elbow arthroscopy in 67 patients. Acta Orthopaedica Belgica 1994; 60:378–83. 48. O’Driscoll SW. Clinical Assessment and Open and Arthroscopic Surgical Treatment of the Stiff Elbow. In: Jupiter JB, ed. The stiff elbow, Monograph Series 33, Chapter 2. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2006. 49. Kelberine F, Bonnomet F, Aswad R, et al. Elbow arthroscopy. Rev Chir Orthop Reparatrice Appar Mot 2006; 92:32–45. 50. Murray O, Nunn T, McEachan J, Rymaszewski L. Treatment by open surgical techniques. In: Stanley D, Trail I, eds. Operative elbow surgery. Ch 29. 2011:417–35. 51. Morrey BF. The Stiff Elbow with Articular Involvement. In: Jupiter JB, ed. The stiff elbow, Monograph Series 33, Chapter 3, Rosemont, IL: American Academy of Orthopaedic Surgeons, 2006. 52. Cheng SL, Morrey BF. Treatment of the mobile, painful arthritic elbow by distraction interposition arthroplasty. J Bone Joint Surg (Br) 2000; 82:233–8. 53. Mansat P, Morrey BF. Semiconstrained total elbow arthroplasty for ankylosed and stiff elbows. J Bone Joint Surg (Am) 2000; 82:1260–8. 54. Throckmorton T, Zarkadas P, Sanchez-Sotelo J, et al. Failure patterns after linked semiconstrained total elbow arthroplasty for posttraumatic arthritis. J Bone Joint Surg (Am) 2010; 92:1432–41. 55. Parikh RK, Rymaszewski LR, Scott NB. Prolonged postoperative analgesia for arthrolysis of the elbow joint. Br J Anaesth 1995; 74:469–71. 56. Lindenhovius AL, Jupiter JB. The posttraumatic stiff elbow: a review of the literature. J Hand Surg [Am] 2007; 32:1605–23. © 2011 British Elbow and Shoulder Society Shoulder and Elbow © 2011 British Elbow and Shoulder Society. Shoulder and Elbow 2012 4, pp 38–45 45