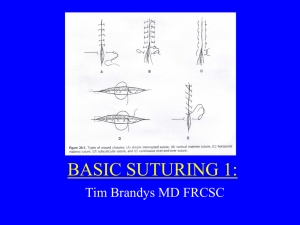
emedicine.medscape.com eMedicine Specialties > Otolaryngology and Facial Plastic Surgery > Wound Healing & Care Sutures and Needles Stephen Y Lai, MD, PhD, Assistant Professor, Departments of Otolaryngology and Pharmacology, University of Pittsburgh Medical Center Daniel G Becker, MD, Clinical Associate Professor, Department of Otorhinolaryngology-Head and Neck Surgery, Division of Facial Plastics and Reconstructive Surgery, University of Pennsylvania; Richard F Edlich, MD, PhD, FACS, FASPS, FACEP, Distinguished Professor of Plastic Surgery, Biomedical Engineering and Emergency Medicine, University of Virginia Health Care System, Charlottesville, Virginia; Director of Trauma Prevention, Education, and Research, Trauma Specialists, LLP, Legacy Verified Level I Shock Trauma Center for Children and Adults at Legacy Emanuel Hospital, Portland, Oregon Updated: May 4, 2009 Introduction The goals of wound closure include obliteration of dead space, even distribution of tension along deep suture lines, maintenance of tensile strength across the wound until tissue tensile strength is adequate, and approximation and eversion of the epithelial portion of the closure. Methods for mechanical wound closure include staples, tape, adhesive, and sutures. Each method has specific indications, advantages and disadvantages, and special considerations. The subject of this article is the suture closure of wounds. Similar to other methods of wound closure, suture closure permits primary wound healing. Tissues are held in proximity until enough healing occurs to withstand stress without mechanical support. An extensive review of wound healing and the factors that influence this process are available elsewhere (eg, see the eMedicine articles Incision Placement; Wound Closure Technique; Wound Healing, Nerve; and Wound Healing, Skin). Suture material is a foreign body implanted into human tissues; it elicits a foreign body tissue reaction. During wound closure, a sterile field and meticulous aseptic technique are critical to minimize the risk of wound infection. Other complications of wound healing, such as hypertrophic scars, wide scars, and wound dehiscence, may result from patient factors (eg, nutritional status), incorrect suture selection, or a technique that results in excessive tension across the wound. Skillful wound closure requires not only knowledge of proper surgical techniques but also knowledge of the physical characteristics and properties of the suture and needle. The goal of this article is to review the types of sutures and needles for wound closure and to discuss principles that influence suture and needle selection. For excellent patient education resources, visit eMedicine's Procedures Center. Also, see eMedicine's patient education article Suture Care. Suture Qualities Ideal suture characteristics The ideal suture has the following characteristics: Sterile All-purpose (composed of material that can be used in any surgical procedure) Causes minimal tissue injury or tissue reaction (ie, nonelectrolytic, noncapillary, nonallergenic, noncarcinogenic) Easy to handle Holds securely when knotted (ie, no fraying or cutting) High tensile strength Favorable absorption profile Resistant to infection Unfortunately, at present, no single material can provide all of these characteristics. In different situations and with differences in tissue composition throughout the body, the requirements for adequate wound closure require different suture characteristics. Essential suture characteristics All sutures should be manufactured to assure several fundamental characteristics, as follows: Sterility Uniform diameter and size Pliability for ease of handling and knot security Uniform tensile strength by suture type and size Freedom from irritants or impurities that would elicit tissue reaction Other suture characteristics The following terms describe various characteristics related to suture material: Absorbable - Progressive loss of mass and/or volume of suture material; does not correlate with initial tensile strength Breaking strength - Limit of tensile strength at which suture failure occurs Capillarity - Extent to which absorbed fluid is transferred along the suture Elasticity - Measure of the ability of the material to regain its original form and length after deformation Fluid absorption - Ability to take up fluid after immersion Knot-pull tensile strength - Breaking strength of knotted suture material (10-40% weaker after deformation by knot placement) Knot strength - Amount of force necessary to cause a knot to slip (related to the coefficient of static friction and plasticity of a given material) Memory - Inherent capability of suture to return to or maintain its original gross shape (related to elasticity, plasticity, and diameter) Nonabsorbable - Surgical suture material that is relatively unaffected by the biological activities of the body tissues and is therefore permanent unless removed Plasticity - Measure of the ability to deform without breaking and to maintain a new form after relief of the deforming force Pliability - Ease of handling of suture material; ability to adjust knot tension and to secure knots (related to suture material, filament type, and diameter) Straight-pull tensile strength - Linear breaking strength of suture material Suture pullout value - The application of force to a loop of suture located where tissue failure occurs, which measures the strength of a particular tissue; variable depending on anatomic site and histologic composition (fat, 0.2 kg; muscle, 1.27 kg; skin, 1.82 kg; fascia, 3.77 kg) Tensile strength - Measure of a material or tissue's ability to resist deformation and breakage Wound breaking strength - Limit of tensile strength of a healing wound at which separation of the wound edges occurs Suture size The United States Pharmacopeia classification system was established in 1937 for standardization and comparison of suture materials, corresponding to metric measures. The 3 classes of sutures are collagen, synthetic absorbable, and nonabsorbable. Size refers to the diameter of the suture strand and is denoted as zeroes. The more zeroes characterizing a suture size, the smaller the resultant strand diameter (eg, 4-0 or 0000 is larger than 5-0 or 00000). The smaller the suture, the less tensile strength of the strand. Suture Material and Structure Natural sutures Natural sutures can be made of collagen from mammal intestines or from synthetic collagen (polymers). Tissue reaction and suture antigenicity lead to inflammatory reactions, especially with natural materials.1,2 Monofilament versus multifilament sutures Monofilament suture is made of a single strand. This structure is relatively more resistant to harboring microorganisms. The monofilament sutures exhibit less resistance to passage through tissue than multifilament suture. Great care must be taken in handling and tying monofilament suture because crushing or crimping of this suture can nick or weaken the suture and lead to undesirable and premature suture failure. Multifilament suture is composed of several filaments twisted or braided together. These materials are less stiff but have a higher coefficient of friction. Multifilament suture generally has greater tensile strength and better pliability and flexibility than monofilament suture. This type of suture handles and ties well. Because multifilament materials have increased capillarity, the increased absorption of fluid may act as a tract for the introduction of pathogens. Absorbable versus nonabsorbable sutures Absorbable sutures provide temporary wound support, until the wound heals well enough to withstand normal stress. Absorption occurs by enzymatic degradation in natural materials and by hydrolysis in synthetic materials. Hydrolysis causes less tissue reaction than enzymatic degradation. The first stage of absorption has a linear rate, lasting for several days to weeks. The second stage is characterized by loss of suture mass and overlaps the first stage. Loss of suture mass occurs as a result of leukocytic cellular responses that remove cellular debris and suture material from the line of tissue approximation. Chemical treatments, such as chromic salts, lengthen the absorption time. Importantly, note that loss of tensile strength and the rate of absorption are separate phenomena. The surgeon must recognize that accelerated absorption may occur in patients with fever, infection, or protein deficiency and may lead to an excessively rapid decline in tensile strength. Accelerated absorption may also occur in a body cavity that is moist or filled with fluid or if sutures become wet or moist during handling prior to implantation. Nonabsorbable sutures elicit a tissue reaction that results in encapsulation of the suture material by fibroblasts. The United States Pharmacopeia classification is as follows: Class I - Silk or synthetic fibers of monofilament, twisted, or braided construction Class II - Cotton or linen fibers or coated natural or synthetic fibers in which the coating contributes to suture thickness without adding strength Class III - Metal wire of monofilament or multifilament construction Suture Characteristics Absorbable Sutures The absorbable surgical sutures are made from either "natural" or synthetic polymers. Natural Collagen: The collagen sutures are derived from the submucosal layer of ovine small intestine or the serosal layer bovine small intestine "gut." This collagenous tissue is treated with an aldehyde solution, which cross-links and strengthens the suture and makes it more resistant to enzymatic degradation. Suture materials treated in this way are called plain gut. Surgical gut, plain: Tensile strength is maintained for 7-10 days postimplantation (variable with individual patient characteristics), and absorption is complete within 70 days. This type of suture is used for (1) repairing rapidly healing tissues that require minimal support and (2) ligating superficial blood vessels. Surgical gut, fast-absorbing: This type of suture is indicated for epidermal use (required only for 5-7 d) and is not recommended for internal use. Surgical gut, chromic (treated with chromium salt): Tensile strength is maintained for 10-14 days. The absorption rate is slowed by chromium salt (90 d). Tissue reaction is due to the noncollagenous material present in these sutures. Also, patient factors affect rates of absorption and make tensile strength somewhat unpredictable. Salthouse and colleagues demonstrated that the mechanism by which gut reabsorbs is the result of sequential attacks by lysosomal enzymes.3 Natural fiber absorbable sutures have several distinct disadvantages. First, these natural fiber absorbable sutures have a tendency to fray during knot construction. Second, there is considerably more variability in their retention of tensile strength than is found with the synthetic absorbable sutures. A search for a synthetic substitute for collagen sutures began in the 1960s. Soon, procedures were perfected for the synthesis of high molecular weight polyglycolic acid, which led to the development of the polyglycolic acid sutures.3 Synthetic Chemical polymers are absorbed by hydrolysis and cause a lesser degree of tissue reaction following placement. Polyglactin 910 (Vicryl): This synthetic suture is a braided multifilament suture coated with a copolymer of lactide and glycolide (polyglactin 370). The water-repelling quality of lactide slows loss of tensile strength, and the bulkiness of lactide leads to rapid absorption of suture mass once tensile strength is lost. The suture is also coated with calcium stearate, which permits easy tissue passage, precise knot placement, and smooth tie-down. Tensile strength is approximately 65% at 14 days postimplantation. Absorption is minimal for 40 days and complete in 56-70 days. These sutures cause only minimal tissue reaction. Vicryl sutures are used in general soft tissue approximation and vessel ligation. Another similar suture material is made from polyglycolic acid and coated with Polycaprolate (Dexon II). This material has a similar tensile strength and absorption profile. Poliglecaprone 25 (Monocryl): This synthetic suture is a monofilament suture that is a copolymer of glycolide and e-caprolactone. The suture has superior pliability, leading to ease in handling and tying. Tensile strength is high initially, 50-60% at 7 days, and is lost at 21 days. Absorption is complete at 91119 days. Poliglecaprone 25 sutures are used for subcuticular closure and soft tissue approximations and ligations. Polysorb Copolymers of glycolide and lactide were synthesized to produce a Lactomer copolymer that is used to produce a new braided absorbable suture, Polysorb. The glycolide and lactide behaved differently when exposed to tissue hydrolysis. Glycolide provides for high initial tensile strength, but hydrolyzes rapidly in tissue.4 Lactide has a slower and controlled rate of hydrolysis, or tensile strength loss, and provides for prolonged tensile strength in tissue. 4 The Lactomer copolymer consists of glycolide and lactide in a 9:1 ratio. The handling characteristics of the Polysorb sutures were found to be superior to those of the Polyglactin 910 suture.4 Using comparable knot construction and suture sizes, the knot breaking strength Polysorb sutures was significantly greater than that encountered by Polyglactin 910 sutures. In addition, the mean maximum knot rundown force encountered with the Polysorb sutures was significantly lower than that noted with the Polyglactin 910 sutures, facilitating knot construction. The surfaces of the Polysorb sutures have been coated to decrease their coefficient friction.5 The Polysorb suture is coated with an absorbable mixture of caprolactone/glycolide copolymer and calcium stearyl lactylate. At 14 days postimplantation, nearly 80% of the United States Pharmacopeia (USP) tensile strength of these braided sutures remains. Approximately 30% of their USP tensile strength is retained at 21 days. Absorption is essentially complete between days 56 and 70. Drake et al studied the determinants of suture extrusion following subcuticular closure by synthetic braided absorbable sutures in dermal skin wounds.6 Miniature swine were used to develop a model for studying suture extrusion. Standard, full-thickness skin incisions were made on each leg and abdomen. The wounds were closed with either sized 4-0 Polysorb or Vicryl sutures. Each incision was closed with 5 interrupted, subcuticular, vertical, loops secured with a surgeon's knot. The loops were secured with 3-throw knots in one pig, 4-throw knots in the second pig, and 5-throw knots in the third pig. The swine model reproduced the human clinical experience and suture extrusion, wound dehiscence, stitch abscess, and granuloma formation were all observed. The cumulative incidence of suture extrusion over 5 weeks ranged from 10-33%. Vicryl sutures had a higher cumulative incidence of suture extrusion than that of the Polysorb sutures (31% vs 19%). With Polysorb sutures, the 5-throw surgeon's knot had a higher cumulative incidence of suture extrusion than the 3-throw or 4throw surgeon's knot square, 30% versus 17% and 10%, respectively. This swine model offers an opportunity to study the parameters that influence suture extrusion. Poliglecaprone 25 (Monocryl): This synthetic suture is a monofilament suture that is a copolymer of glycolide and e-caprolactone. The suture has superior pliability, leading to ease in handling and tying. Tensile strength is high initially, 50-60% at 7 days, and is lost at 21 days. Absorption is complete at 91119 days. Poliglecaprone sutures are used for subcuticular closure and soft tissue approximations and ligations. Polydioxanone (PDS II): This is a polyester monofilament suture made of polydioxanone. This suture provides extended wound support and elicits only a slight tissue reaction. Tensile strength is 70% at 14 days and 25% at 42 days. Wound support remains for up to 6 weeks. Absorption is minimal for the first 90 days and essentially complete within 6 months. This material has a low affinity for microorganisms (like other monofilament). PDS II suture is used for soft tissue approximation, especially in pediatric, cardiovascular, gynecologic, ophthalmic, plastic, and digestive (colonic) situations. Another similar suture material is made from polytrimethylene carbonate (Maxon). This material has a similar tensile strength and absorption profile. Sanz et al randomized 210 rats into one of five study groups to compare three absorbable sutures with a new synthetic absorbable suture, Maxon. They evaluated Maxon, Vicryl, chromic catgut and PDS II with respect to tissue inflammatory reaction, knot security, suture tensile strength, and suture absorption. The results indicated that Maxon and PDS II elicited a lower degree of chronic inflammation when compared with Vicryl and chromic catgut. The tensile strengths of Maxon and Vicryl significantly exceeded those of PDS II and chromic catgut during the critical period of wound healing. Maxon and PDS II retained a larger percentage of tensile strength during the long postoperative period, whereas Vicryl and chromic catgut were mostly absorbed. The authors concluded that Maxon was an excellent addition to the armamentarium of the surgeon. 7 Caprosyn The latest innovation in the development of monofilament absorbable sutures has been the rapidly absorbing Caprosyn suture. Caprosyn monofilament synthetic absorbable sutures are prepared from Polyglytone 621 synthetic polyester, which is composed of glycolide, caprolactone, trimethylene carbonate, and lactide. Implantation studies in animals indicate that Caprosyn suture retains a minimum of 50-60% USP knot strength at 5 days postimplantation, and a minimum of 20-30% of knot strength at 10 days postimplantation. All of its tensile strength is essentially lost by 21 days postimplantation. Pineros-Fernandez et al recently have compared the biomechanical performance of Caprosyn suture with that of chromic gut suture.8 The biomechanical performance studies included quantitative measurements of wound security, strength loss, mass loss, potentiation of infection, tissue drag, knot security, knot rundown, as well as suture stiffness. Both Caprosyn and chromic gut sutures provided comparable resistance to wound disruption. Prior to implantation, suture loops of Caprosyn had significantly greater mean breaking strength than suture loops of chromic gut. Three weeks after implantation of these absorbable suture loops, the sutures had no appreciable strength. The rate loss of suture mass of these 2 sutures was similar. As expected, chromic gut sutures potentiated significantly more infection than did the Caprosyn sutures. The handling properties of the Caprosyn sutures were far superior to those of the chromic gut sutures. The smooth surface of the Caprosyn sutures encountered lower drag forces than did the chromic gut sutures. Furthermore, it was much easier to reposition the Caprosyn knotted sutures than the knotted chromic gut sutures. In the case of chromic gut sutures, it was not possible to reposition a two-throw granny knot. These biomechanical performance studies demonstrated the superior performance ofthe syntheticCaprosyn sutures compared with chromic gut sutures and provide compelling evidence of why Caprosyn sutures are an excellent alternative to chromic gut sutures. The examples listed above represent only some of the available synthetic absorbable sutures. Depending on the anatomic site, surgeon's preference, and the required suture characteristics, other types of synthetic absorbable suture are available. Nonabsorbable sutures Natural Surgical silk: This suture is made of raw silk spun by silkworms. The suture may be coated with beeswax or silicone. Many surgeons consider silk suture the standard of performance (superior handling characteristics). Although classified as a nonabsorbable material, silk suture becomes absorbed by proteolysis and is often undetectable in the wound site by 2 years. Tensile strength decreases with moisture absorption and is lost by 1 year. The problem with silk suture is the acute inflammatory reaction triggered by this material. Host reaction leads to encapsulation by fibrous connective tissue. Surgical cotton: This is made of twisted, long, staple cotton fibers. Tensile strength is 50% in 6 months and 30-40% by 2 years. Surgical cotton is nonabsorbable and becomes encapsulated within body tissues. Surgical steel: This is made of stainless steel (iron-chromium-nickel-molybdenum alloy) as a monofilament and twisted multifilament. It can be made with flexibility, fine size, and the absence of toxic elements. Surgical steel demonstrates high tensile strength with little loss over time and low tissue reactivity. The material also holds knots well. Surgical steel suture is used primarily in orthopedic, neurosurgical, and thoracic applications. This type of suture also may be used in abdominal wall closure, sternum closure, and retention. This material can be difficult to handle because of kinking, fragmentation, and barbing, which renders the wire useless and may present a risk to the surgeon's safety.9 The cutting, tearing, or pulling of other patient tissues is also a risk. Surgical steel in the presence of other metals or alloys may cause electrolytic reactions and, therefore, is not a safe choice in these circumstances. The size of the steel wires is classified by the Brown and Sharpe gauge, ie, 18 (largest diameter) to 40 (smallest diameter). The standard United States Pharmacopeia classification is also used to denote wire diameter. Synthetic Nylon: This is a polyamide polymer suture material available in monofilament (Ethilon/Monosof) and braided (Nurolon/Surgilon) forms. The elasticity of this material makes it useful in retention and skin closure. Nylon is quite pliable, especially when moist. Of note, a premoistened form is available for cosmetic plastic surgery. The braided forms are coated with silicone. Nylon suture has good handling characteristics, although its memory tends to return the material to its original straight form. Nylon has 81% tensile strength at 1 year, 72% at 2 years, and 66% at 11 years. The material is stronger than silk suture and elicits minimal acute inflammatory reaction. Nylon is hydrolyzed slowly, but remaining suture material is stable at 2 years, due to gradual encapsulation by fibrous connective tissue. Polyester fiber (Mersilene/Surgidac [uncoated] and Ethibond/Ti-cron [coated]): This suture material is formed from polyester, a polymer of polyethylene terephthalate. The multifilament braided suture also comes coated with polybutilate (Ethibond) or silicone (Ti-cron). The coating reduces friction for ease of tissue passage and improved suture pliability and tie-down. The suture elicits minimal tissue reaction and lasts indefinitely in the body. Polyester fiber sutures are stronger than natural fibers and do not weaken with moistening. The material provides precise consistent suture tension and retains tensile strength. This suture is commonly used for vessel anastomosis and the placement of prosthetic materials. Polybutester Suture (Novafil): The polybutester is a block copolymer that contains butylene terephthalate and polytetramethylene ether glycol. The polybutester suture has unique performance characteristics that may be advantageous for wound closure.10 This monofilament synthetic nonabsorbable suture exhibits distinct differences in elongation compared with other sutures. With the polybutester suture, low forces yield significantly greater elongation than is seen in the other sutures. In addition, its elasticity is superior to the other sutures, allowing the suture to return to its original length once the load is removed. Coated Polybutester Suture (Vascufil): The clinical performance of polybutester suture has been enhanced by coating its surface with a unique absorbable polymer (Vascufil).11 The coating is a polytribolate polymer that is composed of 3 compounds: gylcolide, ε-caprolactone, and poloxamer 188. Coating the polybutester suture markedly reduces its drag force in musculoaponeurotic, colonic, and vascular tissue. Polypropylene (Prolene): This monofilament suture is an isostatic crystalline stereoisomer of a linear propylene polymer, permitting little or no saturation. The material does not adhere to tissues and is useful as a pull-out suture (eg, subcuticular closure). Polypropylene also holds knots better than other monofilament synthetic materials. This material is biologically inert and elicits minimal tissue reaction. Prolene is not subject to degradation or weakening and maintains tensile strength for up to 2 years. This material is useful in contaminated and infected wounds, minimizing later sinus formation and suture extrusion. Surgipro II : A polypropylene suture has been developed that has increased resistance to fraying during knot rundown, especially with smaller diameter sutures. These sutures are extremely inert in tissue and have been found to retain tensile strength in tissues for as long as 2 years. These sutures are widely used in plastic, cardiovascular, general, and orthopedic surgery. They exhibit a lower drag coefficient in tissue than nylon sutures, making them ideal for use in continuous suture closure.12 Suture Selection Much of the process regarding suture selection depends on surgeon training and preference. A wide variety of suture materials are available for each surgical location and surgical requirement. Generally, the surgeon selects the smallest suture that adequately holds the healing wound edges. The tensile strength of the suture should never exceed the tensile strength of the tissue. As the wound heals, the relative loss of suture strength over time should be slower than the gain of tissue tensile strength. Aesthetic concerns are at a premium in the anatomic regions of the head and neck, such as the eyelid, periorbital area, nose, pinna, lip, and vermillion. In these areas, tensile strength requirements tend to be less, and smaller suture sizes are preferred. However, the mobility of the lip and vermillion requires a relatively higher suture tensile strength. The activity and mobility of the face, anterior and posterior neck, scalp, superior trunk, and nasal and oral mucosa demand higher tensile strength requirements in suture selection. Additionally, major musculocutaneous flaps tend to be closed under significant tension, requiring maximal long-term tensile strength. Certain general principles can be applied to suture selection. Sutures are no longer needed when a wound has reached maximum strength. Therefore, consider nonabsorbable suture in skin, fascia, and tendons (slowly healing tissues), while mucosal wounds (rapidly healing tissues) may be closed with absorbable sutures. Because the presence of foreign bodies in contaminated tissues may facilitate infection, special consideration of suture selection in these locations, such as a contaminated posttraumatic wound, is imperative. Multifilament sutures are more likely to harbor contaminants than monofilament sutures; thus, monofilament sutures are generally preferable in potentially contaminated tissues. Use the smallest inert monofilament suture materials, such as nylon or polypropylene, in this setting. Optimal suture size is generally the smallest size necessary to achieve the desired tension-free closure. If wound tension is high, smaller-diameter sutures may actually injure tissues by cutting through them. Therefore, closely match the tensile strength of the suture and tissue. Emphasizing that the performance of needles and sutures should be evaluated in a selection program by a healthcare resource management group purchasing organization is important.12 Unfortunately, only Consorta, Inc. (Rolling Meadows, Illinois) has had the leadership to do such a surgical suture and needle product evaluation. In this expanded evaluation program, 42 Consorta shareholder hospitals enrolled 1,913 surgeons to participate in an observational study of the clinical performance of surgical sutures and needles produced by Covidien. In these 30 day studies, the surgeons found that the needles and sutures were clinically acceptable in 98.1% of the evaluations. Surgical glove selection Surgeons who use sutures and needles should wear sterile surgical gloves without cornstarch. In 2008, 13 health professionals filed a citizen's petition to the Food and Drug Administration (FDA) to ban cornstarch powder on medical gloves.13 Cornstarch has been documented to promote wound infection, to cause serious peritoneal adhesions and granulomatous peritonitis, and to be a well-documented vector of the latex allergy epidemic. Because the FDA allows 1.5% of the surgical gloves to have holes, these holes allow the transmission of blood with deadly borne viral infections to be transmitted between the patient and the surgeon. Consequently, the use of the Biogel double-glove hole indication system should be used to detect the location and presence of holes in the gloves, allowing the surgeon to change the gloves when a hole is detected.14 After surgery has begun, one of the major causes of glove holes is surgical needle penetration through the glove, which can be detected by the double-glove hole indication system. Needle Qualities Surgical needles are produced from stainless steel alloys, which have excellent resistance to corrosion. 12 All true stainless steels contain a minimum of 12% chromium, which allows a thin, protective surface layer of chromium oxide to form when the steel is exposed oxygen. Since their development during the early 1960s, high nickel maraging stainless steels have found extensive use in structural materials in many applications that require a combination of high strength and toughness. The basic principle of maraging consists of strengthening FeNi martensitic matrices by the precipitation of fine intermetallic phases, such as Ni 3 Ti. These precipitates are so small that they are only evident on transmission electron microscopy. They strengthen the metal by preventing the planes of atoms in the stainless steel from sliding over each other. A high nickel maraging stainless steel, like S45500, is composed of 7.5-9.5% nickel, 0.8-1.4% titanium, and 11-12.5% chromium. In contrast, S42000 stainless steel is composed of 12-14% chromium without nickel or titanium. Scientists have successfully used the concept of high nickel maraging stainless steels (S45500) to develop stainless steel wires with superior strength and ductility for use as surgical needles. Surgical needles made of a high nickel maraging stainless steel have a greater resistance to bending and breakage than stainless steels without nickel. Wound closure and healing is affected by the initial tissue injury caused by needle penetration and subsequent suture passage. Needle selection, surface characteristics of the suture (eg, coefficient of friction), and suturecoating materials selected for wound closure are important factors that must be considered by the surgeon. Ideal surgical needle characteristics High-quality stainless steel Smallest diameter possible Stable in the grasp of the needle holder Capable of implanting suture material through tissue with minimal trauma Sharp enough to penetrate tissue with minimal resistance Sterile and corrosion-resistant to prevent introduction of microorganisms or foreign materials into the wound Needle performance characteristics and definitions Strength - Resistance to deformation during repeated passes through tissue (Increased needle strength results in decreased tissue trauma.) o Ultimate moment - Measure of maximum strength determined by bending the needle to 90° o Surgical-yield moment - Amount of angular deformation that can occur before permanent needle deformation occurs Ductility - Resistance (of a needle) to breakage under a given amount of deformation/bending Sharpness - Measure of the ability of the needle to penetrate tissue (Factors affecting sharpness include the angle of the point and the taper ratio, ie, ratio of taper length to needle diameter.) Clamping moment - Stability of a needle in a needle holder, determined by measuring the interaction of the needle body with the jaws of the needle holder Anatomy of a Needle Point This portion of the needle extends from the tip to the maximum cross-section of the body. Body This part of the needle incorporates most of the needle length. The body of the needle is important for interaction with the needle holder and the ability to transmit the penetrating force to the point. The needle factors that affect this interaction include needle diameter and radius, body geometry, and stainless steel alloy. These components determine the needle-bending moment, ultimate moment, surgical-yield moment, and needle ductility. Swage The suture attachment end creates a single, continuous unit of suture and needle. The swage may be designed to permit easy release of the needle and suture material (pop-off). Channel swage: A needle is created with a channel into which the suture is introduced, and the channel is crimped over the suture to secure it into place. The diameter of the channel swage is greater than the diameter of the needle body. Drill swage: Material is removed from the needle end (sometimes with a laser), and the needle is crimped over the suture. The diameter of the drill swage is less than the diameter of the needle body. Nonswaged: Alternatively, the suture may be passed through an eye, similar to that found in a sewing needle. In a closed-eye configuration, the shape may be round, oblong, or square. In a French (split or spring) eye, a slit is in the end of the needle with ridges that catch and hold the suture in place. Several disadvantages are associated with the use of a nonswaged needle. Tissue passage of a double strand of suture leads to more tissue trauma. In a swaged needle, the suture is less likely to become unthreaded prematurely. Also, decreased handling helps maintain suture integrity. Swaged sutures are not subject to suture fraying or damage due to sharp corners in the eye of eyed needles. Needle coating The needle may be coated with silicone to permit easier tissue passage. The coating helps reduce the force needed to make initial tissue penetration and the frictional forces as the body of the needle passes through the tissue. Needle measurements Chord length: This is the linear distance from the point of the curved needle to the swage (bite width). Needle length: The distance measured along the needle from the point to the swage is termed needle length. Needle length, not chord length (bite width), is the measurement supplied on suture packages. Radius: This is the distance from the body of the needle to the center of the circle along which the needle curves (bite depth). Diameter: The gauge or thickness of the needle wire is considered the diameter. Point types Cutting: The needle has at least 2 opposing cutting edges (the point is usually triangular). This type is designed for penetration through dense, irregular, and relatively thick tissues. The point cuts a pathway through tissue and is ideal for skin sutures. Sharpness is due to the cutting edges. o Conventional cutting: This type of needle has 3 cutting edges (triangular cross-section that changes to a flattened body). The third cutting edge is on the inner, concave curvature (surface-seeking). o Reverse cutting: The third cutting edge is on the outer convex curvature of the needle (depthseeking). These needles are stronger than conventional cutting needles and have a reduced risk of cutting out tissue. The needles are designed for tissue that is tough to penetrate (eg, skin, tendon sheaths, oral mucosa). Reverse-cutting needles are also beneficial in cosmetic and ophthalmic surgery, causing minimal trauma. o Side-cutting (spatula): These needles are flat on the top and bottom surfaces to reduce tissue injury. The needles allow maximum ease of penetration and control as they pass between and through tissue layers. Side-cutting needles were designed initially for ophthalmic procedures. Taper-point (round needle): This type of needle penetrates and passes through tissues by stretching without cutting. A sharp tip at the point flattens to an oval/rectangular shape. The sharpness is determined by taper ratio (8-12:1) and tip angle (20-35°). The needle is sharper if it has a higher taper ratio and lower tip angle. The taper-point needle is used for easily penetrated tissues (eg, subcutaneous layers, dura, peritoneum, abdominal viscera) and minimizes potential tearing of fascia. Beveled, Conventional Cutting Edge Needles: A new beveled, conventional cutting edge needle, has been developed with superior performance characteristics over those of other conventional cutting edge needles. It is composed of a unique stainless steel, ASTM 45500, that has been heat-treated after the curving process to enhance the resistance to bending. The angle of presentation of its cutting edge has been decreased to enhance needle sharpness. On the basis of the results of experimental and clinical studies done by Kaulbach et al, this needle is recommended for closure of lacerations. 15 Blunt-point: This type of needle dissects friable tissue rather than cuts it. The point is rounded and blunt, ideal for suturing the liver and kidneys. Additionally, blunt needles are being developed for more conventional uses in an effort to reduce needlestick injuries. Body types Straight: This body type is used to suture easily accessible tissue that can be manipulated directly by hand. The straight-body needle is also useful in microsurgery for nerve and vessel repair. Examples of straight-body needles include the Keith needle, which is a straight cutting needle used for skin closure of abdominal wounds, and the Bunnell needle, which is used for tendon/GI tract repair. Half-curved ski: This type of needle is rarely used in skin closure because it is difficult to handle. The straight portion of the body does not follow the curved point, resulting in an enlarged curved point, which makes the needle difficult to handle. Curved: The needle has a predictable path through tissue and requires less space for maneuvering than a straight needle. The semicircular path is the optimal course for sutures through tissue and provides an even distribution of tension. Body curvature is commonly a quarter-inch, three eighthsinch, half-inch, or five eighths-inch circle. The three eighths–inch circle is used most commonly for skin closure. The half-inch circle was designed for confined spaces, and more manipulation by the surgeon is required (ie, increased wrist motion is required). Compound curved: This needle curvature was originally designed for anterior segment ophthalmic surgery. The body has a tight 80° curvature at the tip, which becomes a 45° curvature throughout the remainder of the body. A microvascular compound curved needle also may facilitate vessel approximation in microvascular surgery. Needle–Needle Holder Interaction and Selection Criteria The stability of the needle within the needle holder affects needle control and performance. The jaws of the needle holder must be appropriate to the needle size to hold it securely and prevent rocking, turning, and twisting. An ovoid cross-section of the needle body often maximizes both the surface contact with the needleholder jaws and the bending moment of the needle. The needle-holder handle must be appropriate for the depth needed for placement of the suture. The difference between the length of the handle and the jaw creates a mechanical advantage for exerting force through the needle point. The needle-holder clamping moment is the force applied to a suture needle by a needle holder. The jaws of the needle holder contact a curved needle at 1 point on the outer curvature and 2 points along the inner curvature. The force against the needle creates a moment arm, which acts to flatten the curvature of the needle. Technically speaking, the needle-holder clamping moment must be less than the surgical yield of the needle, or the needle will bend and ultimately may break. A bent needle takes a relatively traumatic path through soft tissue and may cause increased soft tissue injury. Repetitive injury by the needle holder also may cause the needle to break. If the broken portion of the needle is not identified and retrieved immediately, surgery may be delayed in efforts to find it. The need for intraoperative radiology and other potential difficulties may ensue. Recent studies by Abidin et al demonstrated that the sharp edges of smooth needle holder jaws cut the smooth surface of monofilament sutures, weakening their strength.16 When the smooth tungsten carbide inserts of needle holders clamped 6-0 monofilament nylon suture with the first opposing teeth of the needle holder ratchet mechanism interlock, there was a significant reduction in suture breaking strength. This sutural damage can be prevented by mechanical grinding the outer edges of the smooth tungsten carbide inserts, resulting in a rounded edge. Clamping the suture with the smooth jaws of the needle holder was atraumatic with no demonstrable damage to the suture’s breaking strength.16 Selection criteria No standardized sizing system or nomenclature is available for needles or needle holders. The main consideration in needle selection is to minimize trauma. A taper needle is sufficient for tissues that are easy to penetrate. Cutting needles are typically reserved for tough tissues. As a general guide, select tapered sutures for all closures except skin sutures. The length, diameter, and curvature of the needle influence the surgeon's ability to place a suture. The needle-body diameter ideally matches the suture size. References 1. Tera H, Aberg C. Tissue holding power to a single suture in different parts of the alimentary tract. Acta Chir Scand. 1976;142(5):343-8. [Medline]. 2. VanWinkle W Jr, Hastings JC. Considerations in the choice of suture material for various tissues. Surg Gynecol Obstet. Jul 1972;135(1):113-26. [Medline]. 3. Salthouse TN, Williams JA, Willigan DA. Relationship of cellular enzyme activity to catgut and collagen suture absorption. Surg Gynecol Obstet. 1981;129:691-6. 4. Lin KY, Farinholt HM, Reddy VR, Edlich RF, Rodeheaver GT. The scientific basis for selecting surgical sutures. J Long Term Eff Med Implants. 2001;11(1-2):29-40. [Medline]. 5. Faulkner BCGear AG, Hellewell TB, Mazzarese PM, Watkins FH, Edich RF. Biomechanical performance of a braided absorbable suture. Surg gynecol Obstet. 1981;153:497-507. 6. Drake DB, Rodeheaver PF, Edlich RF, Rodeheaver GT. Experimental studies in swine for measurement of suture extrusion. J Long Term Eff Med Implants. 2004;14(3):251-9. [Medline]. 7. Sanz LE, Patterson JA, Kamath R, Willett G, Ahmed SW, Butterfield AB. Comparison of Maxon suture with Vicryl, chromic catgut, and PDS sutures in fascial closure in rats. Obstet Gynecol. 1988;71:41822. [Medline]. 8. Pineros-Fernandez A, Drake DB, Rodeheaver PA, Moody DL, Edlich RF, Rodeheaver GT. CAPROSYN*, another major advance in synthetic monofilament absorbable suture. J Long Term Eff Med Implants. 2004;14(5):359-68. [Medline]. 9. Edlich RF, Drake DB, Rodeheaver GT, Winters KL, Greene JA, Gubler KD, et al. Syneture stainless STEEL suture. A collective review of its performance in surgical wound closure. J Long Term Eff Med Implants. 2006;16(1):101-10. [Medline]. 10. Rodeheaver GT, Nesbit WS, Edlich RF. Novafil. A dynamic suture for wound closure. Ann Surg. Aug 1986;204(2):193-9. [Medline]. 11. Rodeheaver GT, Shimer AL, Boyd LM, Drake DB, Edlich RF. An innovative absorbable coating for the polybutester suture. J Long Term Eff Med Implants. 2001;11(1-2):41-54. [Medline]. 12. Szarmach RR, Livingston J, Edlich RF. An expanded surgical and needle evaluation and selection program by a healthcare resource management group purchasing organization. J Long Term Eff Med Implants. 2003;13(3):155-70. [Medline]. 13. Edlich RF, Long WB 3rd, Gubler KD, Rodeheaver GT, Thacker JG, Borel L, et al. Citizen's Petition to Food and Drug Administration to ban cornstarch powder on medical gloves: Maltese cross birefringence. Am J Emerg Med. Feb 2009;27(2):227-35. [Medline]. 14. Edlich RF, Wind TC, Heather CL, Thacker JG. Reliability and performance of innovative surgical double-glove hole puncture indication systems. J Long Term Eff Med Implants. 2003;13(2):6983. [Medline]. 15. Kaulbach HC, Towler MA, McClelland WA, Povinelli KM, Becker DG, Cantrell RW. A beveled, conventional cutting edge surgical needle: A new innovation in wound closure. J Emerg Med. 1990;8:253-63. [Medline]. 16. Abidin MR, Towler MA, Thacker JG, Nochimson GD, McGregor W, Edlich RF. New atraumatic rounded-edge surgical needle holder jaws. Am J Surg. 1989;157:241-2. [Medline].