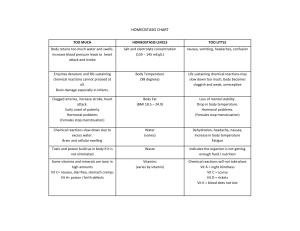
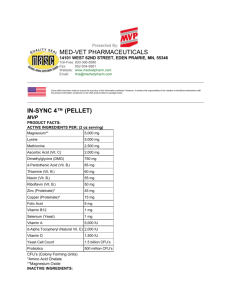
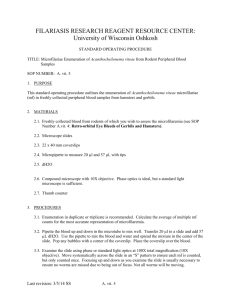
T1- Energy Among 6 nutrients, only macronutrients (carbs, protein, fat) can provide energy RNI (Recommended Nutrient Intake) 1. Nutrients: o A component in food that an organism uses to survive & grow o Amount required is affected by: Age Sex Physiological condition o Hence, it’s imp for us to know RNI at dif age group 2. Who come out with RNI? o Technical Sub-Committee (1969) Representative from different background IMR PHT of MOH WHO University of Malaya o Obj: provide advice on dietary aspects of the proposed Applied Nutrition Pilot Project o 1st meeting: 20/9/2002 o Outcome: RNI book published in 2005 o They need to review & revise RNI from time to time due to Advances in scientific knowledge Deteriorating state of health of the nation 3. Definition of RNI o Daily intake which meets the nutrient requirements of almost all apparently healthy individuals in an age- & sex-specific population group 4. how they come out with ideal body height & weight? o Calculate average value from healthy population done by local researchers 5. Usage of RNI o Policy maker Plan and monitor national related activity Campaign New policy o Program planner Health promotion activity o Food industry & marketing o Clinical practitioner dietitians o Researcher Energy Requirement 6. Affected by: 1. Genders a. Women < men i. Men more lean body mass ii. 2. Growth a. Infant, children vs adults, elderly 3. Age a. Lower in adulthood i. Hormones influence appetite, body weight, metabolism change with age ii. Hence young ppl 4. Physical activity a. Various activities are clustered accrd to the typical intensity of a day’s effort b. Physical activity factor for various levels of intensity 5. Body composition a. Tall > short i. Larger surface area b. More hairy i. More basal metabolism c. Hence, Asian < western i. They taller and more hairy than Asian ppl ii. Hence Malaysia come out with their own set of RNI not using RDA, cause body composition is different Method calculating basal energy need: Direct method= calculate the energy lost as heat from body Indirect = oxygen consumption o Metabolic process not only produce heat, but also consume oxygen Regulation of Food Intake 1. Physiological aspects 色香味+口感 o o o o Sensation (mouthfeel) Appearance Texture (soft, hard, crispy) Smell (olfaction) & gustation (taste) Some chemical can be taste at lower conc than others We can compare with the relative taste indices Higher indices lower conc to be detected able to provide more intense taste. o o o Reference compound index=1 The higher the index, the sweeter/ sourer Fructose is sweeter than sucrose Citric acid is less sour than HCl 2. Psychological aspects o Causes to make healthy food choice i. Knowledge 1. Level of education a. Dietitian > business students .. b. Nutrition savvy ii. Motivational factors 1. Conducive to proper food choice a. Intrinsic factors i. Belief abt health & nutrition ii. Cognitions (thoughts) positive iii. Goal setting, action plants iv. Self-monitoring & management v. contracting b. Extrinsic factors i. Praise ii. External Reward 1. Give you iphone if you follow healthy diet iii. Support frm others iv. Food available (proper/improper) v. Physical activity vi. Models of proper behaviors 2. Conflicting with proper food choice a. Time: i. travel 1. Impossible to eat healthily as we wanna try out all the tasty food within short periods of the time b. Job, association c. Characteristic of the regimen/plan i. Cost ii. Complexity d. Personal, family, cultural practices e. Social occasion i. Friend ii. Parties iii. Celebration iii. Affective influence (**Feelings & attitudes) 1. Emotional states a. Boredom b. Fear, anxiety c. Depression d. Happiness e. Stress f. weather 2. Physical condition a. Threat to health b. Fatigued or rested c. State of health d. Severity of illness Types and Food Sources: Nutritional Interest Energy-yielding nutrients o Nutrients that break down to yield energy the body can use o 3 ORGANIC NUTRIENTS: (contain “c” in the structures) Carbs Fat Protein o Inorganic nutrients: Water mineral Macronutrients CFP o Body needs in relatively large amount (no need yield energy) Grams/ day Water o o o Consider macronutrients in this course But unlike CFP can’t provide energy Hence some article or books may not put water under macronutrients Calories: o o o o o o Energy released from CFP Calories Measured in kilocalories 1 kcal = 1000 cal 1 kcal = the amt of heat necessary to increase the temp of 1 kg of water 1C Carbs = 4kcal/g Protein= 4kcal/g Fat= 9kcal/g Alcohol (not a nutrient) =7kcal/g Will interfere the body growth and metabolism All the CPF acetyl CoA enter TCA cycle o Micronutrients vitamins & minerals Body requires in small amounts o Mg/ microgram per day Vitamin vs minerals: o o Similarity: Micronutrients Non-energy yielding nutrients DIFFERENCE: Vitamin is organic, mineral is inorganic Carbohydrate: Types: I. Simple carbs a. Monosaccharides: i. All contain same chemical formula C6H12O6 with dif chemical structure (arrangement) ii. Glucose, fructose, galactose b. Disaccharides i. Mono condensation disaccharide ii. Types: 1. Maltose 2. Sucrose= table sugar 3. Lactose= milk sugar II. Complex Carbs a. Oligosaccharides i. 3-10 sugar units ii. Eg: 1. Raffinose 2. Stachyose 3. Verbascose iii. Found mostly in beans, peas, whole grains iv. Human digestive enzyme X hydrolyze them prebiotic b. Polysaccharide: i. More than 10 units of monosac linked ii. Types: 1. Glycogen a. X be found in plant-based food b. Little in meat c. Almost X be found in food food isn’t a significant source of glycogen 2. Starch a. Amylopectin i. branched b. Amylose i. unbranched 3. Fiber Digestion and Absorption of Carbohydrates Ultimate goal: glucose absorption & use In mouth: Salivary amylase Hydrolyze starch to shorter polysaccharides maltose At neutral pH Very little carbs digestion take place here Stomach: Bolus mixed with stomach acid & protein digesting enzymes Acid inactivates salivary amylase Fibers delay gastric emptying Satiety & fullness SI: (most carbs digest at proximal SI) Starches: Pancreatic amylase I. Breakdown starch at 1-4 linkages to shorter glucose chains & maltose Brush border of enterocyte enzymes I. Break disaccharide & oligosaccharide mono o Maltase o Sucrase o Lactase Broken monosac absorbed into bloodstream via capillaries of villi portal vein to liver Fibers: Hydrogen positioned on the beta side of the oxygen enzyme X break the bond (sterospecificity of enzymes) LI (focus on fibers) Fibers attract water softens stools for passage wo straining GI bac ferment some fibers I. Generate water, gas, SCFA Consumption of large amt of lactose (esp lactase deficiency), fructose, stachyose, raffinose, alcohol sugars Unabsorbed in SI pass to colon Increase gas and loose stools Absorption: Active transport: When glucose & galactose at low luminal conc involve specific receptors SGLT1 (sodium dependent-glucose/galactose cotransporter) need Na+ to facilitate the process I. the glucose/galactose binding site is available only when the transport protein bound a Na+ ** this is why sodium-glucose drink are used to rehydrate diarrhea or athletes lost too much fluid Facilitated diffusion: High luminal conc all monosac use GLUT 2 (Na-independent) I. Esp after large carb meal increase intestinal glucose conc II. Facilitated transporter GLUT2 Fructose I. Specific facilitative transporter = GLUT5 II. Relative slow absorption than glucose & galactose (actively absorbed) o Can result in a smaller increment of blood glucose Fructose is better than glucose/galactose Hence fruits sugar is better than other sugar Metabolism Primary: in liver Non-insulin dependent All sugar carried directly first to liver Fructose & galactose can be converted into glucose derivatives same fate as glucose= I. stored as liver glycogen II. circulate in blood control BGlvl III. catabolize for energy accd to liver energy demand IV. if sugar intake exceed body oxidative & storage capacity convert into fat little/ no galactose & fructose found in blood * Fructose: I. Only liver has the receptors for fructose only liver can use fructose to produce energy o High-fructose diet increase risk of fatty liver Secondary: muscle & adipose tissue Insulin-dependent Metabolism & Utilization of Carbohydrates Glucose is key player (fuel for all cells) Metabolic pathways: Glycogenesis: synthesis of glycogen Glycogenolysis: breakdown of glycogen Glycolysis: oxidation of glucose ATP Gluconeogenesis: production of glucose frm non-carb intermediates I. Lactate, pyruvate, glycerol, certain Amino acid Hormone: Insulin= anabolism , store CFP Glucagon= catabolism 1. Storing glucose as glycogen Liver storage (1/3 of total body glycogen) Condensation into glycogen I. Eat BG rise insulin increase and process glucose condense into glycogen stored in liver Hydrolysis for release of glucose when needed I. Imp during hunger immediately breakdown int glucose for utility II. Directly Release glucose into blood Imp in maintaining blood glucose homeostasis III. But only provide 5% of the energy? Muscle storage: (2/3 of total body glycogen) Cannot directly contribute to blood glucose lvl I. It only provides energy within the muscle cells during muscle contraction - X released into blood II. Bcs it lacks the enzyme that converts phosphorylated glucose back to free glucose Selfish only breakdown during exercise Although the conc of glycogen in liver is higher than muscle, muscle stores most of the glycogen (~75%) as muscle make up a much greater portion of the body’s weight Storage depends on PA of individual I. Can increase glycogen concentration in muscle by increasing physical training 2. Glucose for energy Glycolysis 1Glucose 2pyruvate (3carbon compounds) Aerobic pathway: I. Pyruvate enter mitochondria TCA cycle/ Krebs cycle complete oxidized into H2O + CO2 + large amt of energy Anaerobic: I. Pyruvate lactate + small amt energy o The extra lactate leave muscle cell liver convert into glucose (gluconeogenesis) II. Happens due to lack of O2 / high cellular metabolism o High intensity exercise III. ** the major metabolic pathway for RBC as they X have mitochondria Fuels most of body’s cells Esp: brain, nerve cells, RBC only use glucose as fuel Cellular breakdown of glucose 3. Making glucose from protein Body would make glucose from other source of nutrients when we lack of glucose Gluconeogenesis Synthesis of glucose from noncarb precursor I. Amino acid II. glycerol III. Lactate Primary site: I. Liver (most) II. Kidney Body proteins source: liver & skeletal muscles Reverse the glycolytic pathway Consume ATP Synthesize glucose It has to be regulated! Or else too many ammonia and urea produced affect kidney function 4. Ketone bodies from fat fragments ** only during starvation You don’t eat anything (not only not enough glucose like the gluconeogenesis) I. Fat (breakdown) ketone body provide energy Ketone body may accumulate in our blood if more that our body required lead to ketosis interfere acid-base balance not good for our body How to prevent this ketosis? I. Daily intake of >= 50-100g carbs for protein sparing (preserve protein) & prevention of ketosis o Body prefer glycogen > protein > fat o Starvation metabolism changes step: i. Most of this glucose can be synthesized through gluconeogenesis from glycerol, lactate, and selected amino acids during the early phase of starvation. ii. as the starvation continues, the body attempts to protect its protein component and the amino acid substrates for gluconeogenesis become less available. iii. This, coupled with the rising ketone level (ketones can cross the blood–brain barrier), serves to induce the utilization of the ketones by the brain as a metabolic fuel. iv. after 48 h of starvation, Proteolysis is suppressed by rising levels of growth hormone as the body attempts to conserve its body proteins. The initial proteolysis, however, serves to provide the needed amino acids for the synthesis of enzymes needed for survival (enzymes needed for energy mobilization and conservation). Once these mechanisms are established, body protein is conserved. 5. Using glucose to make fat If glycogen capacity is full in liver & muscle Extra glucose fat as storage Glucose Homeostasis Glucose supply steadily in blood stream Source: intestine & liver (secondary: kidney during starvation may gluconeogenesis) Cond: Low BG dizzy & weak High BG fatigue Regulating hormone: Insulin Glucagon I. Bring glucose out from storage 3. The storage capacity of muscle and liver for glycogen is full, hence insulin may also stimulate glucose convert into fat I. Hence don’t consume more than our RNI for carbs as it will be stored as fat. Failure in blood glucose regulation Diabetes hypoglycemia diabetes =chronic disorder of carbs metabolism, usually resulting from insufficient / ineffective insulin I. o Clinical: use fasting BG to confirm diabetic status of ppl (repeated fasting BG) T1DM I. Cause: pancreas failed to produce enough insulin o Mainly due to genetics II. Tend to develop at young age III. Cant be prevented IV. Need insulin therapy T2DM I. Cause: insulin resistance o Due to environmental factors II. Tend to develop at older age III. Can be prevented with lifestyle changes IV. Can be managed with lifestyle modifications alon if diagnosed early Hypoglycemia =abnormally low BG conc I. low blood glucose level (70 mg/dl or less) caused by I. the administration of excessive insulin or insulin secretagogues, II. too little food, delayed or missed meals or snacks, III. increased exercise or other physical activity IV. alcohol intake without food Symptoms: I. Weak, rapid heartbeat, sweating, anxiety, hunger, trembling o Hypoglycemia can be difficult to diagnose because these typical symptoms can be caused by many different health problems besides hypoglycemia. For example, adrenaline (epinephrine) released as a result of anxiety and stress can trigger the symptoms of hypoglycemia. Cause I. Medication II. Pancreatic tumor III. Overuse of insulin o If diabetes IV. alcohol abuse o reduce glucose secretion frm liver recommendation: I. replacing refined carbs with fiber-rich o we wanna keep blood glucse lvl as stable as possible o sugar stimulate insulin release further reduce the blood glucose lvl o Inborn Errors of Carbohydrate Metabolism Affect the catabolism & anabolism of carbs Lactose Intolerance A type of digestive disorder I. Absence of enzyme lactase in SI no absorption II. Bcm nutrients for gut microbiota in colon (fermentation) o produce large amt of SCFA & gases (methane, CO2, hydrogen) bloat, diarrhea, abdominal cramps III. Unabsorbed lactose act osmotically attract water increase fecal water diarrhea IV. The hydrogen gas may be absorbed by body and exhaled in the breath diagnose lactose intolerance with breath analyzed for hydrogen gas production after lactose intake Types: i. PRIMARY (adult) lactose intolerance I. II. Common o Related to genes Cause: o Decrease in lactase production with age After weaning, our lactase may decrease ii. Secondary lactose intolerance III. IV. Rare Cause: o Illness (stomach bug/ celiac disease) o Inflammation in gut wall temporary decline in lactase Solution I. Chew tablet (food enzyme dietary supplement) Beano o o natural enzyme alpha-galactosidase break down carbs in beans into simple sugar easier to digest Hereditary Fructose Intolerance Inability to convert fructose glucose due to deficiency of “fructose-1-phosphate aldolase” I. This enzyme is found in liver, kidney & mucous membrane of SI II. Causing Intracellular accumulation of fructose-1-phosphate toxic liver cell death Symptoms: (when eating fructose accumulation) I. Nausea, bloating, abs pain, diarrhea, vomiting II. hypoglycemia o accumulation may inhibit of glycolysis & gluconeogenesis fructose-1-phosphase cant be broken down to maintain blood sugar trapping of phosphate reduce ATP production III. toxic effect if repetitive ingestion of fructose o on liver, kidney, SI Infants I. Failure to thrive II. if you notice when infant is introduced with fruits and experience those symptoms then it may be due to fructose intolerance repetitive consumption of fructose-containing food kidney/ liver damage food contain fructose I. sucrose, sorbitol II. fruits Dietary Fiber Hipsley=non-digestible constituents making up the plant cell wall latest def= fraction of edible part of plants/their extracts/ analogous carbs, that are resist to digestion & absorption in the SI, usually with complete/partial fermentation in the LI types: Function: Health benefit approved by FDA: I. along with a decreased consumption of fats (<30% of calories), an increased consumption of dietary fiber from fruits, vegetables and whole grains may reduce some types of cancer a. Increase fiber consumption i. = six or more “one-ounce equivalents”, with three ounces derived from whole grains. A one-ounce equivalent would be consistent with one slice of bread, ½ cup oatmeal or rice, or five to seven crackers b. 1 ounce – 28g II. c. Diets low in saturated fat & chol & increase in F&V & whole grain reduce risk of CHD ~25-35g/d of which 6g are soluble fiber Water-holding/hydration capacity and viscosity = the ability to bind water and form viscous, slow-moving solution within GIT Factors: Soluble > insoluble Degree of processed Coarse > fine Effect: 1. Delay gastric empty Postprandial satiety Slow down digestion and carbs and lipid are not digest in stomach 2. Reduce mixing of GI content with digestive enzyme Reduce enzyme function Form a physical barrier trapping nutrient to touch with enzyme 3. Decreased nutrient diffusion rate attenuate blood glucose response Thicken the unstirred water layer by the viscous fiber solution retard the rate of diffusion of nutrients into enterocyte Certain fiber affect the release of hormone Fiber: gums, pectin, beta-glucan, psyllium , resistant starch Hormone: glucagon like peptide 1 & insulin I. GLP1 o Promote tissue utilization of glucose o High fiber increase GLP1 reduce insulin needs o This is beneficial for DM who is insulin resistant II. Application: o Some DM friendly food may midified the starch of the food to resistant starch So that DM can enjoy cabrs without excessive elevation in blood glucose conc and inslin needs 4. Increase transit time slower the movement of the food Soluble delay, insoluble increase If shorten decrease nutrient absorption Adsorption or Binding Ability The ability to bind to substances such as enzymes / nutrients in GI effect: 1. diminished absorption of lipids fiber adsorb FA, chol, bile acid cannot form micelles X be absorbed bcs need to be in micelles form to be transported across the unstirred water layers excreted in feces 2. increased fecal bile acid excretion fiber-bound bile acid X be reabsorbed to enterophepatic recirculation excrete in feces 3. lowered serum cholesterol concentrations (hypocholesterolemia properties) a. increase excretion of bile acid & chol in feces a. decreased hepatic chol promote removal of LDL from blood to increase hepatic chol to form new bile acid b. production of SCFA a. inhibit FA & chol synthesis 4. altered mineral, carotenoid, and phytochemical absorption some fibers (hemicellulose, pectin, gums) + fructose, galactose, oligosaccharides form catonic bridges with minerals in GIT the overall effect (negative/positive) depend on the degree of fermentability or accessibility to bacterial enzymes in the colon acidic environment generated by fermentation aids in mineral solubility I. Ca, Mg, Zn, Fe bound to fiber may be released in colon absorbed Negative effect on I. Carotenoid II. Phytochemicals Improve phytochemical absorption through bacterial action I. Polyphenol as conjugated glycosides may be converted unconjugated by bacterial action II. Aglycone are better absorbed Fermentable fibers a. Prebiotics Not all fermentable fibers are prebiotic = promote the colonic growth or activity of selected health-promoting species of bacteria Include: Fructans (inulin, oligofructose, fructooligosaccharides) Galactose Lactulose Soybean oligosaccharides (raffinose, stachyose, verbascose) b. SCFA Acetic, butyric, propionic acides Roles: Increase water & Na absorption in colon Mucosal cell differentiation & proliferation Acidify luminal environment Provision of energy Inhibit chol synthesis Improve colonic blood flow Enhance immune function Nonfermentable fiber a. Detoxification Insoluble fiber adsorb hydrophobic carcinogen to prevent their interaction with colonic mucosa b. Increased fecal volume Dietary carbohydrates and dental caries Dental caries (tooth decay) = activity of certain species of bac that live in dental plague Streptococcus mutans & S.sobrinus Stage: I. Initial demineralization i. Enamel: hardest tissue in our body 1. Made of minerals ii. When enamel exposed to acid lose minerals II. Enamel decay i. White spots on tooth darken to brownish color ii. Small hole form in teeth Formation of cavities/ dental caries III. Dentin decay i. Dentin: tissue lie under enamel ii. (softer) sensitive to damage from acid faster rate of tooth decay IV. Pulp damage i. Pulp: innermost layer of tooth ii. Contain many nerves & bv imp to keep the tooth healthy iii. Damage tooth pain V. Abscess formation i. Abscess: a pocket of pus forming at the bottom of the tooth ii. Swelling of gum, face, jaw, fever, swallon Main cause: High-sugar food I. Bac ferment sugar producing acid II. Food Factor: o Time of food in mouth o Stickiness o Frequency of sugar consumption Nutritive & Non-nutritive Sweeteners Artificial sweeteners Non-nutritive sweeteners Insignificant energy virtually no energy Eg: Aspartame Cyclamate Saccharin Sucralose Stevia Herbal products Derived from the leaves GRAS safety Sugar alcohols Used in commercial food products Normally will label as “sugar-free” =/ calorie free Nutritive sweeteners: sugar alc still provide kcal, but fewer than sugar benefit: lower glycemic response body absorb sugar alc slower side effect: intestinal gas abs discomfort diarrhea ** o food label have to mention” excess consumption have a laxative effect” eg: relative sweetness: o compare the sweetness of sugar alc > table sugar o smaller than 1 less sweet than table sugar isomalt half of the sweetness of table sugar but the energy also half of it macam no dif lo xylitol same sweet as table sugar with half of the kcal of sugar but have some side effect like diarrhea! o T1- protein Why 0 sugar still got kcal? Substitution of sugar alcohol (nutritive sweetener) Amino acids: ~20 amino acids with different side groups a protein Source: Animal Meat, poultry, fish, eggs, dairy products (except butter, sour cream, cream cheese) Plant Grains, grains product, legumes, vegetable Endogenous protein presented to digestive tract Desquamated mucosal cells Digestive enzyme & glycoprotein frm digestive secretion Structure: Central carbon + at least 1 amino group (-NH2) + at least 1 carboxy grp (-COOH) + 1 side chain (R group) All have same structure but different side groups That’s why have dif Size, shape, electrical charge 1. Essential amino acids Human body X synthesize at all/ insufficient quantity to meet its needs Obtained from diet VILLa HM = Ten Thousands Pounds 2. Nonessential amino acids Can be syn in body From Nitrogen & fragments of carbs/ fat 3. Conditionally essential amino acids: (6) Under special condition Nonessential AA conditionally essential AA When the need for it exceeds the body’s ability to produce it Liver disease (cirrhosis) Neonates born prematurely immature organ function X synthesis some nonessential AA Phenylketonuria PKU How to know the content of amino acid in food? Use HPLC Digestion & absorption Ultimate goal: Absorb & utilize AA The purpose of protein digestion is to liberate the amino acids from the consumed proteins in babies: protein can be absorbed in intact Prior to gut closure, the neonate can absorb some proteins. Most of these proteins are immunoglobulins. 1. Mouth: a. Protein is crushed & moistened b. No real action of digestion 2. Stomach a. HCL i. Denature protein: (Partial hydrolysis of protein ) 1. Uncoils (denatures) protein’s tangled strands so that the digestive enzymes can attack the peptide bonds 2. Peptide bonds not affected ii. Activate enzyme pepsinogen pepsin 1. Unactivated enzyme= zymogen / proenzyme b. Pepsin: i. Convert large polypeptides smaller polypeptides & some AA ii. Works under pH <~3.5 3. Small intestine: a. Hormone: i. Secretin + cholecystokinin 1. Stimulate secretion of pancreatic juice a. Bicarbonate, electrolytes, water, proenzyme (X active in pancreases) 2. Stimulate enterocyte secrete mucus-rich secretion + enteropeptidase b. Enteropeptidase i. Activate trypsin trypsin activate other proenzyme c. Pancreatic & intestinal protease i. Further hydrolyze polypeptides short peptide chains, tripeptides, dipeptides, AA d. Enzyme peptidase i. Secrete frm membrane surface of intestinal cell ii. Split most dipeptides, tripeptides single amino acid 4. Absorption a. Site: i. duodenum ii. upper jejunum b. metabolites: i. amino acids 1. less effective absorption than peptide 2. EAA absorb faster than NAA 3. Neutral > basic/acidic 4. Branched > smaller AA 5. Ingesting large amt of one AA impair absorption of other AAs a. Bcs they may be using the same carrier system ii. peptide 1. more rapid absorption than AA 2. majority of AA is absorbed in peptide form into enterocyte 3. enterocyte breakdown peptide AA intracellularly release to blood c. mechanism: i. Specific carriers (most) 1. Transport AA into intestinal cells 2. Most of them are Na-dependent transporter ii. (few) paracellular absorption 5. In enterocytes, AA a. may be used for energy b. synthesize needed compounds i. structural proteins ii. nucleotides iii. apoproteins necessary for lipoprotein (chylomicron) formation iv. new digestive enzymes v. hormones vi. nitrogen-containing compounds c. unused aa transport across cell membrane into the surrounding fluid where they enter the capillaries Transport to i. Primary: liver 1. Monitor & adjust rate of metabolism (cata/ anabolism) 2. Main site for catabolism of EAA a. Except BCAA tend to be utilized by muscle & heart ii. Other: kidney, other organ Metabolism & utilization 1. Protein turnover (PT) & the amino acid pool (AAP) PT: the degradation & synthesis of protein (2 process) Occur within each cell AA pool The made up of AA in this pool is relatively constant Despite difference in protein intake & rate of degradation of tissue protein Source of AA pool (mix tgt) Dietary protein Endogenous AA from breakdown of body tissue AA pool includes: AA in plasma AA in cytosol of body cells Regardless of the source (protein breakdown / dietary protein), all AA can be Used to make NEAA protein nitrogen-containing compounds neurotransmitter hormones glucose fatty acids ketones Stripped of their N used for energy 2. Nitrogen balance (assessment of protein needs) Amt of nitrogen consumed (N in) as protein as compared with the amt of N excrete (N out) in a given period of time Only protein contains N atom, carbs & fat X have Protein contains ~ 16% Nitrogen To estimate protein requirement Calculation Nitrogen intake = protein intake * 0.16 protein intake(g)/ 6.25 Nitrogen loss (U)urine (F)feces (S)skin nitrogen balance/ status = In − [(U − Ue) + (F − Fe) + S]. e= endogenous = losses of nitrogen of subject under nitrogen-free diet Output Nitrogen equilibrium N in = N out Positive nitrogen N in > N out o When our body need extra protein o Pregnant, growing infants, children, adolescents, ppl recovering frm protein deficiency / illness Negative nitrogen N in < N out o Due to protein breakdown (muscles) to produce energy o Starvation, suffering from severe stress (burns, injuries, infections) Disadvantage: Nitrogen balance =/ amino acid balance Overestimate true nitrogen retention rates in body Due to Incomplete collection & measurement of losses 3. Using amino acids to make other compounds a. Tyrosine (precursor= phenylalanine no enzyme converts p T in PKU) i. Neurotransmitters (nervous system message) 1. Norepinephrine 2. Epinephrine ii. Pigment melanin 1. In melanocytes in skin, eye, hair cells 2. Imp for hair, eye, skin color iii. Hormone thyroxin 1. In thyroid gland + iodine 2. Metabolic rate b. Tryptophan i. Precursor for vit niacin (not very efficient) ii. Precursor for serotonin 1. Appetite regulator iii. Precursor of melatonin 1. In pineal gland 2. Regulate circadian rhythms & sleep 4. Using AA for energy & glucose AA not used for synthesizing other compound deaminated carbon unit (keto acid) used for energy Keto acid= Gluconeogenesis Protein can use to make glucose to provide energy Under carb deficiency + deplete glycogen This process should be avoided la will break down muscle 5. Using AA to make fat Excess glucose will store as glycogen (storage phase) but X storage phase for protein stored as fat Energy & Protein intake exceed needs + carbs intake is adequate store as fat Excess AA can convert to fat & stored for later use Amino Acid Catabolism: Involve 2 process: transamination & deamination (-NH2) Deamination o Removal of amino grp (-NH2) from an AA (“Normally” essential AA ) Products: Ammonia NH3 o Needed to provide N for synthesis of NAA from keto acid Keto acid o Use to produce a particular NAA o Transamination: (synthesis of NEAA) Catalyze by aminotransferases/transaminases o Cofactor: B6 (pyridoxal phosphate PLP) o High conc in lover, normally low serum lvl Liver damage high serum AST & ALT Amino group excrete or use for N-containing comp production Keto acid Produce energy (when diet inadequate in energy) Gluconeogenesis Only glucogenic AA o = catabolism of AA must yield pyruvate or intermediates of TCA cycle o Not all types of AA can be used to synthesis glucose o Some of the carbon skeleton of certain type of AA can be used to produce glucose Oxaloacetate Carbon Skeleton of aspartate Pyruvate Carbon Skeleton of alanine Bth Oxa anf pyruvate are used to produce glucose Primarily in liver, but also kidney & SI Speed up by high glucagon conc (due to low blood glucose) o In between meals o Fasting cause liver glycogen storage deplete o Infection/ trauma/injury o Ketogenesis: Ketogenic AA o Catabolism of AA must generate acetyl-CoA or acetoacetate used to form keto bodies Fatty acid production Excess energy & protein intake + adequate carbohydrate intake A new nonessential amino acid A is formed Utilization: 1. Growth & maintenance (anabolism) Building blocks for most body structures Replace dead/ damaged cells Life span of skin cell: 30days New cells made largely of protein grow frm underneath replace old skin cells Muscle cells make new proteins to grow larger & stronger in response to exercise Factor affecting anabolism: Anabolic substances promote protein synthesis & prevent protein degradation Growth hormone Insulin o ** the anabolic effect of insulin is greater extend if both cabrs & protein ar coingested vs ingested alone individually. Catabolic gluconeogenesis, ureagenesis Glucagon Cortisol o Infection/trauma Epinephrine 2. Enzymes Facilitate chemical reactions w/o being changed in the process catalyst 3. Hormones Some hormones are proteins Various endocrine glands release hormones in response to changes that challenge the body The blood carries hormone target tissue elicit responses restore/maintain normal conditions Exp: Catecholamines tyrosine Melatonin tryptophan Growth hormone promote growth Insulin/glucagon Thyroxin (tyrosine + Iodine) regulate body metabolic rate Calcitonin & parathyroid hormone regulate blood Ca Antidiuretic hormone regulate fluid & electrolyte balance 4. Regulators of fluid balance Protein (albumin) helps attract & keep water inside a particular area contribute to osmotic pressure Critical illness / protein malnutrition plasma protein leak into tissue attract water fluid accumulation tissue swelling edema A diminished capacity to deliver nutrients & O2 to cells & remove wastes 5. Acid-base regulators (buffer) Maintain blood pH at 7.35-7.45 or other cellular pH Protein negative charges on surfaces Attract H+ By accepting & releasing H+ protein maintain acid-base balance of blood & body fluid Extreme of acidosis & alkalosis coma & death 6. Transporters Transport protein carry Esp for vit & minerals Na+, K+-ATPase pump Nutrients Amino acid transporter in intestinal cell brush border Oxygen , Co2 Hemoglobin TG, Chol Lipoprotein Other transporter Albumin Relatively long half-life (14-18days) indicator of protein status Transthyretin / prealbumin Retinol-binding protein Vit A 7. Structural Element a. Contractile protein i. Actin ii. Myosin b. Fibrous protein i. Collagen ii. Elasin iii. Keratin 8. Antibodies 9. Acute Phase Responders Liver synthesis Acute phase protein in response to infection (sepsis), injury, inflammation Eg: C-reactive protein 10. Role: used to evaluate inflammation in patients clinically Dramatically increase within few hours of inflammation Fibronectin Orosomucoid Sitmulate IR Promote wound healing Chelating/ remove free Fe to prevent used by bacteria for growth Source of energy provide energy & glucose starvation / insufficient carbs intake Gluconeogenesis Body breaks down its tissue protein to make AA available for energy / glucose production Losing lean body tissue Ketogenic: The catabolism of the AA must generate non-TCA cycle intermediates which are used for ketone bodies formation such as Acetyl CoA Acetoacetate Glucogenic The catabolism must yield selected intermediates of TCA cycle to be converted into glucose Pyruvate Oxaloacetate Succinyl CoA Nutritive values of proteins Protein quality of diet affect how children grow & adult maintain their health Affect by: a. Digestibility i. Protein source & other food eaten with it 1. Animal: 90-99% 2. Plant: 70-90% b. Amino acid composition i. Supply enough EAA High quality protein: Dietary protein containing all EAA needed to support the body’s work Protein from animal Limiting amino acid: The indispensable / essential AA that is present in the lowest quantity in the food Deficiency: Protein deficiency rarely occurs alone. Instead, it is often coupled with insufficient energy intake. They differ in the severity of energy deficiency as shown in the figure below. 1. Marasmus Condition: Chronic period of insufficient energy & protein, vitamins & minerals intake Vulnerable ppl: Infant (6-18 month) cessation of breastfed In overpopulated & impoverished areas Characteristic Extremely thin matchstick limbs like old ppl Muscle wasting Adipose tissue wasting Prominent bones Indicators of visceral protein status Within normal range/ just below normal range (not decreased to extent seen in kwashiorkor) Complication: Impair brain development & learning ability Affect ppl in rapid growth Decrease synthesis of key hormone Growth hormone is made of protein Little / no fat under skin Reduce metabolism & btemp Mental & behavioral development retardation Growth ceases= stunt Good appetite possible 2. Kwashiorkor Acute PEM= A sudden & recent deprivation of food Condition: Typically ingest enough energy (usually as carbs) Insufficient protein Characterized by: Inadequate visceral protein status High insulin level prevents protein breakdown to form visceral protein Low total protein conc in blood o Albumin o Retinol-binding protein o Prealbumin Consequence: Edema in limbs & abdomen Low protein conc water diffuse frm blood to interstitial spaces 1st appear at legs face all over body Muscle mass, adipose mass may be normal Carbs intake stimulate insulin production storage hormone prevent fat metabolism inhibit ketogenesis limiting adaptation to starvation Fatty liver X synthesis transport protein of lipids out of liver Reduce tyrosine for melanin loss hair color Inadequate protein synthesis skin patchy & scaly Loss of appetite Susceptible population Children 1-3yo Developing country Extreme cases significantly increase protein need Burns Sepsi Trauma Following major surgery Kwashiorkor vs Marasmus 3. Cachexia A muscle loss & wasting condition that is associated with an underlying illness Cancer AIDs Multiple sclerosis Tuberculosis Altered metabolic adaptation proinflammatory cytokines & resting energy expenditure Loss of body weight, fatigue, weakness & loss of appetite Inborn Errors of Protein Metabolism Cause: Mutation in genes encoding key enzyme in AA metabolic pathway Total loss / partial loss of catalytic activity More than 50 AA metabolic disorder majority are very rare Autosomal recessive inheritance 1. Phenylketonuria (PKU) \ Inability of body to utilize phenylalanine (EAA) Due to defective activity of phenylalanine hydroxylase to convert phenylalanine Tyrosine Consequence: Buildup of phenylalanine & its metabolites (phenylacetate, phenylpyruvate, phenylacetate) in blood & other body fluid hyperphenylalaninemia Blood tyrosine conc diminish Blood phenylalanine level Normal: ~1 mg/dL PKU: ~ 6-80mg/dL (usually > 30mg/dL) Sign & symptom Mild severe Classic PKU most severe form * infant with classic PKU appear normal until they are a few months old w/o treatment permanent intellectual disability seizure delayed development behavioral prob psychiatric disorder musty/mouse-like odor hypopigmentation no tyrosine to form melanin albinism 白化病 eczema treatment low intake of phenylalanine & aspartame aspartame nonnutritive sweetener made of aspartic acid + phenylalanine supplement of tyrosine 2. Homocystinuria Autosomal recessive disease Characterized by: Eye Myopia ectopia lentis dislocated lense Skeletal system Too tall, slender Osteoporosis Vascular system Thromboembolism CNS Developmental delay Seizure Psychiatric problem Other Hypopigmentation of skin, hair Cause: Genetical cause: Deficiency of enzyme cystathionine beta-synthase (vit B6 requiring enzyme) o Convert homocysteine cysteine o accumulation of homocysteine & its metabolite in urine & blood Deficiency of MTHDF o methionine remethylation defects o Convert homocysteine methionine o Folate & vitamin B12 dependent Abnormal cobalamin metabolism non-genetical cause deficiency of cobalamin B12 deficiency of pyridoxine B6 Methionine catabolism 1. Methionine is converted into SAM (S-adenosyl methionine) a. SAM is a principal methyl doner in body b. Needed to synthesis of other substances c. Used to methylate DNA 2. The removal/ donation of methyl grop from SAM SAH (S-adenosyl homocysteine) 3. SAH homocysteine 4. Homocysteine can be converted ack to methionine in 2 ways: a. Betaine-dependent reaction i. Generated in liver from choline ii. Provide methyl group to homocysteine b. Vitamin B12 (as methylcobalamin) + folate (as 5-methyl tetrahydrofolate)-dependent reaction i. Methylcobalamin get the methyl frop from 5-methyl tetrahydrofolate (coenzyme form of folate) ii. Methylcobalamin provides the methyl group to homocysteine to form methionine Methionine is the precursor of cysteine (conditionally EAA) 5. Homocysteine + serine –(cystathionine-synthase + vitamin B6) cystathionine a. Vitamin B6 in coenzyme form (OKO) are needed for this process 6. Cystathionine cysteine Methionine homocysteine –X cysteine o homocysteine can be reconverted into methionine with the help of (methyl donor) Folate Betaine Choline oxidized to form betaine o Homocysteine cysteine Require Vit B6 ** may be seen in patients with cobalamin B12 & folate deficiency cause: i. deficiency of cobalamin ii. deficiency of folate iii. deficiency of cystathionine beta-synthase w/o treatment: dislocated lenses cataract muscle weakness elevated homocysteine may interfere collagen corss-linking in bone increase fracture risk thrombosis due to homocysteine delay in the development & hypercoagulability treatment Vitamin B6 therapy aids in homocysteine cysteine low dose of folic acid or folate + B12 supplement help in reversion of homocysteine --> methionine but the amt need to be controlled bcs it aids in both direction of o methionine homocysteine Unlike betaine, only aids in one direction o homo --> methionine cysteine supplement methionine-free amino acid formula + cysteine supplement drinks betaine provide alternate remethylation pathway of homocysteine methionine a low protein diet 7. Maple syrup urine disease =branched-chain ketoaciduria Autosomal recessive disease Due to Deficiency of enzyme branched-chain alpha-keto acid dehydrogenase (BCKAD) Needed to metabolize BCAA (mostly in skeletal muscle) o Leucine, isoleucine, valine Imp for muscle protein metabolism for energy & growth Characterized by: Neurological & developmental delay Within brain, BCAA metabolism maintain glutamate level o BCAA transamination form glutamate o Glutamate neurotransmitter within CNS imp for brain development & cognitive function o Leucine accumulation is neurotoxin Maple syrup odor to urine Feeding problem Nausea, anorexia Roles Valine mental health & muscle coordination Leucine regulate glucose in skeletal muscle & maintain the amt of muscle protein Isoleucine hemoglobin formation & regulate blood sugar level W/o treatment Sweet-smelling urine Neurological damage Poor feeding Vomiting Dehydration Lethargy Hypotonia Seizure Ketoacidosis Pancreatitis Coma Treatment Diet low in BCAA (not completely cut off) Thiamin supplement Thiamin is needed for BCKAD as coenzyme T3- Fat Lipid Insoluble in water Type: Triglyceride: Fat in food Made up: o 1 glycerol o 3 fatty acids Phospholipids Made of: o 1 glycerol o 2 fatty acids o 1 phosphate group Hydrophilic sol in water Make phospholipid sol in hydrophobic/hydrophilic environment Emulsifier Sterol Multiple ring structure No fatty acids Found in o Animal Cholesterol o Plant Phytosterol Food source: Visible Marbling in meat Butter Oil invisible fat in whole milk eggs whole grain baked products convenience food Fatty acids: An organic acid Consist of: Carboxylic acid (-COOH) alpha end Methyl grp (-CH3) omega end Differentiate by: Carbon chain length Degree of saturation 1. Carbon chain length Most naturally occurring FA even numbers of Carbon Classified: Long chain (12-24C) Most of your food is LCFA Medium chain (6-10C) coconut Short-chain (<6 c) Carbon Chain length lower, melting point lower liquid 2. Degree of Saturation Saturation= Whether or not a fatty acid chain is filled to capacity with hydrogen atoms SFA only single bonds between C fully loaded with H Point of unsaturation = where H atoms are missing on the chain More saturated FA solid More unsaturated FA liquid in room temp Visible & invisible fat Butter is visible fat which we will straight relate to fat but walnut as invisible fat also very high in fat Plant higher in unsaturated FA animal higher in saturated FA Essential FA Needed by the body but not made by it in amt sufficient to meet physiological needs 2 EFA Linoleic acid n-6 Alpha-linolenic acid n-3 Cell X possess enzymes to Make o-6 & 3 FA frm scratch Convert o-6 o=3 or vice versa Whereas o-6 can be converted to other complex FA via (but the conversion rate is very slow X solely depend on the dietary O-6 for arachidonic acid) Elongation Desaturation Omega-6 FA Primary member: linoleic acid (precursor for complex O6FA) When body get LA frm diet make other members of O-6 family Conditionally essential FA When LA deficient all other FA derived frm LA conditionally EFA need to obtain frm diet Types: (major 4 still many more types) Omega 3 FA Primary member: alpha-linolenic acid Can be converted into EPA (eicosapentaenoic acid) 20C 8-21% CONVERSION DHA (Docosahexaenoic acid) 22C 0-9% conversion Can be considered conditionally EFA ** imp for : Eyer & brain Normal growth & cognitive development Conversion competes with the same enzymes in omega 6 pathway (elongase, desaturase) further decrease the conversion rate ** food source effective way to maintain O-3 & O-6 bod supplies Type: EFA deficiency 1. Skin a. Scaly, dry skin 2. Weight a. Decrease 3. Circulation a. Heart enlargement; decreased capillary resistance (lower blood pressure at periphery); increased permeability 4. Kidney a. Enlargement; intertubular hemorrhage 5. Lung a. Cholesterol accumulation 6. Endocrine glands a. Adrenals: weight decreased in females and increased in males b. Thyroid: reduced weight 7. Reproduction a. Females: irregular estrus and impaired reproduction and lactation b. Males: degeneration of semini-ferrous tubules 8. Metabolism a. Changes in fatty acid composition of most organs b. Increase in cholesterol levels in liver, adrenals, and skin c. Decrease in plasma cholesterol d. Changes in swelling of heart and liver mitochondria and uncoupling of oxidative phosphorylation e. Increased triglyceride synthesis and release by the liver Digestion & Absorption: GI tract receives 50-100 TG 4-8g phospholipid 200-350mg cholesterol 1. Mouth a. Lingual lipase released (not actioned) i. Acid-stable (stomach HCl) b. Physical state: Mastication of food mix lingual lipase with food 2. Stomach (2-4hours) a. Physical state: churning of stomach mix food with HCl separate lipid particles exposing more surface area for enzyme action & emulsion formation i. Lipid-protein complexes are cleaved by 1. HCL denaturation 2. attack of gastric protease b. Gastric lipase i. Minimally breakdown triglyceride (only 30%) diglyceride & fatty acid 1. Bcs most of the lipid floats above the watery content of swallowed food c. Activation of lingual lipase i. Limited effect due to tendency of lipid to coalesce & form a separate phase ii. Digested lipid by them release single fatty acid (short/medium chain FA) + diacylglycerol 1. Imp for infant a. Milk= main source mostly s/mcfa b. Immature duodenal lipase 2. Less imp for adult a. Mix diet iii. The Released diacylglycerol + s/mcfa emulsifier/surfactants stabilize emulsion produce chyme expelled into duodenum 3. Small intestine: a. Hormone: (stimulate by chyme’s entry) i. Cholecystokinin stimulate gall bladder to contract release bile ii. Pancreozymin stimulate pancreas pancreatic juice (lipase) b. Physical state: i. Bile salt (not bile) = emulsifying agent due to its amphipathic properties further Disperse lipid droplet frm stomach micelles facilitate hydrolysis of glycerides by pancreatic lipase (Such molecules tend to arrange themselves on the surface of small fat particles, with their hydrophobic ends turned inward and their hydrophilic regions turned outward toward the water phase. This chemical action, together with the help of peristaltic agitation, converts the fat into small droplets with a greatly increased surface area.) 1. Bile salt impart negative charge to lipid attract pancreatic lipase 2. c. Pancreatic lipase i. Remove the fatty acids of triglyceride monoglyceride & a glycerol, fatty acid An inhibitor of gastric and pancreatic lipase, orlistat, has been developed to reduce the absorption of dietary triacylglycerols. It is marketed both as Xenical, a prescription-only product, and Alli, an over-the-counter product. The rationale for use is that when the hydrolysis of TAG is restricted, less dietary fat will be absorbed, resulting in decreased caloric intake. Xenical inhibits the absorption about 30% or by 200 kcal from fat per day. d. Absorption: i. Stabilized by the polar bile salt, the micellar particles are sufficiently water soluble to penetrate the unstirred water layer that bathes the enterocytes of the small intestine Micelles transfer digested products brush border 1. SCFA simple diffusion through epithelial cells blood 2. LCFA/ monoglyceride unpack frm micelles simple diffusion in cell, repacked into triglyceride packaged + fat-sol vitamin as chylomicron lacteal of villus circulate in lymphatic circulation left at left subclavian vein hepatic vein liver a. Chylomicron= large TAG-rich spherical particles containing TAG, cholesteryl esters, phospholipids (PL), and vitamins A and E in the core and a monolayer of PL, free cholesterol, and protein on the surface 4. Large intestine: a. Some fat & cholesterol trapped in fiber (adsorbent) exist in feces i. Esp soluble fiber able to form gel-like consistency of chyme 5. Bile: a. Metabolism & Utilization: 1. Adipose cells store fat after meals Chylomicrons circulate reach tissue that using lipid as fuel TG hydrolyze by lipoprotein lipase frm lipoprotein Fatty acid, diglycerides, monoglycerides enter adipose cell TG reassembled inside adipose cells To store energy 2. Using fat for energy Energy deprivation stored TG released glycerol & FA directly into blood Body cell use these compounds to yield energy, CO2, water Catabolism of TAG & FA Glycerol + 3 FA Glycerol o Used for energy by liver and other tissue having enzyme glcerokinase Convert to glycerl phosphate enter glycolytic pathway at the level of dihydroxyacetone phosphate enter energy oxidation or glyconeogenesis Fatty acid o Very rich source of energy o Mechanism = beta-oxidation o Step: Enter the cell of metabolizing tissue activated by coenzyme A Mitochondrial transfer of Acyl CoA Oxidation of FA is in mitochondria SCFA can pass directly in LCFA need the help of carnitine (carrier molecule) Beta-oxidation Yielding acetyl CoA Acetyl CoA then enter krebs cycle to produce energy Ketone bodies formation o Other than direct oxidation through kreb cycle, acetyl-Co A may follow other catabolic routes in the liver to make ketone bodies Acetoacetate, beta-hydroxybutyrate, acetone o KB are not oxidized in the liver, but transported by blood to other tissue that contain enzyme to reconvert KB back to acetyl CoA to enter krebs cycle o This is a “overflow” pathways for acetyl CoA Giving another way for liver to distribute the fuel to peripheral cells Eg: o Accelerated fatty acid oxidation o Low carb intake o Impaired carbs used o DM o Starvation o Why low carbs leat to KB ? Without oxidation of glucose, the supply of oxaloaxetate is reduced Oxa is needed to bind with acetyl-CoA to enter kreb cycle As low carb also induce FA oxidation overload with acetyl-CoA, but cannot enter kreb cycle directly only can form ketone body to lower acetyl-CoA 3. Insulating & protecting >=30% body weight = adipose tissue o Visceral fat= protect vital organs o Subcutaneous fat= insulate body from extreme temp & keep internal climate under control Pads the hands & buttocks Prevent friction 4. Regulating & signaling Hormones Adipose tissue secretes hormone leptin to regulate appetite Reproductive health infertile Sustain nerve impulse transmission, memory storage & tissue structure 5. Maintain cell membranes Cell membrane is made of o Phospholipid bilayer Cholesterol 1. Food source: Dietary chol= main steroid frm animal tissues Top 5 o Egg & its dish o Chicken o Beef & its dish o Burgers o Cheese Source contribute to liver cholesterol pool o Dietary (exogenous) Transport as chylomicron o De novo (endogenous) Transport as VLDL, LDL, HDL It is not an energy-producing nutrient The main excretion pathway o Via bile excretion 2. Function Precursor of other steroids o Cholesterol is the most common sterol in animals and is the precursor for other steroids. a. bile acids b. steroid sex hormones (estrogens, androgens, and progesterone) c. the adrenocortical hormones; d. vitamin D (cholecalciferol) form & maintain cell membrane & structures o particularly of nerve cell nerve cell insulation 3. Relationship with chronic diseases Dietary cholesterol raise blood cholesterol increase CVD o Effect is not as strong as SFA & trans fat Chol found in all animal food o Eat less fa from animal food lower dietary chol + SFA Transport of lipids Lipoproteins o Clusters of lipid associated with proteins that serves as transport vehicles for lipid in blood 1. Chylomicron: Largest & least dense not synthesized by liver but enterocyte Role: o Transport dietary lipids frm SI to tissues o The role of the chylomicron is to deliver dietary lipid mostly to tissues other than the liver, such as muscle and adipose tissue (80%). Much of the remaining lipid (20%) is delivered to the liver in the form of chylomicron remnants transported by the blood throughout all tissues in the body--> intravascular hydrolysis at certain tissue sites (lipoprotein lipase) at endothelial cell surface of the small blood vessels and capillaries primarily in adipose tissue and muscle (but not in the liver) The part of the chylomicron that is left following this lipolytic action = chylomicron remnant (a smaller particle, relatively lower in triacylglycerol, but richer in cholesterol and cholesteryl esters) removed from the bloodstream by hepatocyte endocytosis 2. VLDL Role: Transport lipid frm liver to tissues is made of endogenous TAG chylomicron remnant cholesterol carried back by LDL from previous cycle that carried out by last VLDL but not deposited in the body tissue The removal of TAG frm VLDL continues until a cholesterol-rich LDL particle remains. Undeposited VLDL (yellow dots) LDL will carry back to the cycle again to get a chance to be deposited If still not deposited LDL carried back to liver to be made again into VLDL HDL carried back to liver to be excreted Cloud-circled one = similar The chylomicron remnant enters into the hepatocyte in the same manner as LDL The fasting serum VLDL is very low Bcs is quickly metabolized into IDL/ LDL 3. HDL Role: carry chol out of bloodstream into liver (reverse cholesterol transport) Made by liver to take up the chol that is not deposited back to liver To be made into other useful metabolite To make vit D etc.. For other usage 4. LDL Transport Chol & other lipid frm liver to tissues Bind 60% of the blood chol Provide chol for dif tissue to make Membraine Convert to other metabolite such as hormone These tissue has to have LDL receptor One of them is endothelium fatty plague When VLDL has distributed the TG content to other tissue, the remaining bcm LDL cholesterol rich LDL is one of the major lipoprotein during fasting serum The concentration of cholesterol Liver in fat metabolism: 1. site of synthesis of lipoprotein (the other is enterocyte--> chylomicron) 2. synthesize new lipids from nonlipid precursors (glucose/ AA) 3. take up & catabolize dietary lipid (in the form of chylomicron remnants/ MCT/LDL)--> repack them into HDL/ VLDL forms high carbs (esp simple sugar) --> accelerate hepatic TAG production frm glucose --> observe hypertriacylglycerolemia in healthy ppl when they consume high simple sugar diet Cholesterol and cholesteryl esters from the chylomicron remnant may be used in several ways 1. converted to bile salts and secreted in the bile 2. secreted into the bile as neutral sterol (such as cholesterol or cholesteryl ester) 3. incorporated into VLDL or HDL and released into the blood beneficial effect of omega 3, 6, 9 fatty acids replace both SFA & trans fat with mono & polyUFA heat disease prevention low rate of heart disease in Mediterranean region olive oil 1. MUFA & phytochemicals (rich in virgin olive oil) Omega 3 reduce risk of heart disease & stroke 1. Prevent blood clots 2. Protein against irregular heartbeats 3. Lower blood pressure 4. Healthy immune system 5. Defend against inflammatory disorder American heart association recommendation: 1. 2 serving of fatty fish a week Grill, bake, broil X fried & frozen fried reduce omega 3, increase trans & SFA 2. Combine with physical activity Supplement of fish oil 1. Routine supplementation is not recommended 2. Overdosage: >3g perday Complication Increase bleeding time Interfere with wound healing Raise LDL Suppress immune function Trans fatty acids characteristic: linear shape like saturated FA How it's made: o During the dehydrogenation process, electronic shifts cause remaining, unhydrogenated cis double bonds to revert to a trans configuration that is energetically more stable Zero trans-fat: o use a blend of natural oils containing a chain length and unsaturation level that provide the desired properties without any hydrogenation o labeling regulations = >0.5 g of trans fat/ serving --> can result in consuming more than the recommended level impact: o even more unfavorable than SFA o increase LDL & chol + lower HDL Ketosis a metabolic process occurs when body begins to burn fat for energy o liver produce ketones supply to ketone-using tissue to be used as energy condition: o X enough carbohydrate Common o Diabetes Impaired insulin production intracellular glucose deficiency o Ketogenic diet Outcome: o Bad breath (acetone) o Increase ketones in blood o Appetite suppression Low insulin o Initial short-term fatigue o Digestive issue o Insomnia o Short-term decrease in performance o Ketonuria o Weight loss o Increased focus & energy Dietary lipids & Atherosclerosis Excess intake of SFA, trans-fat, chol CVD Saturated fat o Increase LDL-cholesterol more SFA --> increase chylomicron remnant + unused up VLDL--> increase formation of LDL circulating in the blood Trans-fat o Increase LDL o Decrease HDL Cholesterol o Effect of increase blood chol increase risk of CvD not so strong as SFA & trans fat o The reason why chol is considered the culprit for CVD is due to that it is the major component of fatty plague o But dietary chol only has minor influence on blood chol conc in most ppl Bcs compensatory mechanism like HDL activity in scavenging excess chol Down-regulation of chol synthesis by dietary chol o Genetic also play a vital role Some is hypo/hyperesponders to chol Dietary Lipids & Cancer Lesser relationship between lipid intake & initiate cancer development o But promote cancer once it has arisen Differ in Types of cancer: o Breast cancer Weak & inconclusive evidence More convincing evidence= body fat contributes to the risk o Colon cancer Limited evidence Differ in types & combination of fat o SFA or fat from meat increase cancer risk o Fat from milk. Fish not implicate in cancer risk O-3 suppress inflammation may protect against some cancer Dietary advice to reducte cancer risk = same as for reduction of heart disease o Replace SFA with USF + increase O-3 Fat Substitutes 1. Fat replacers ingredients that replace some or all of the functions of fat & may /may not provide energy o Less than 9kcal/g a. Carbs-based Thickeners / stabilizers o Soup & salad dressings b. Protein-based Creamy feeling o Ice cream & yogurts c. Fat-based Emulsifiers & heat stable o shortenings 2. Artificial fat o o o = zero-energy fat replacers that are chemically synthesized to mimic the sensory & cooking qualities of naturally occurring fats but resistant to digestion Olestra A sucrose mol with 6-8 fatty acids X breakdown by digestive enzyme Concern of FDA Is olestra toxic? No reports of cancer or birth defects Affect nutrient absorption & health of digestive tract? It binds some fat-sol vit & carries them out of body o Hence products with olestra need to fortify with fat-sol vit May experience digestive distress o Initially FDA required warning label of olestra now no need T4- Vitamin A Fat soluble vitamins: Similar to fat in metabolism and transportation Require bile to form micelles Store in adipose tissue… Introduction 1st vitamin identified as essential micronutrients =a term for the biologically active compound retinol & its provitamin (precursor) carotenoids Food sources Carotenes (pro-vitamin A) are found in plant o But more than 600 members of carotene family of pigment found, only 550-60% can be converted into vitamin A than can be used by our body Plant source (pro-vitamin A) o o Animal (vitamin A) o nomenclature & structure Vitamin A not just single compound many forms If they have the same similar chemical structure provide the possible activity in body Exp: o Natural: Retinol Retinal Carotene (alpha, beta, gamma) o Synthetic: Retinyl acetate Retinyl palmitate Chemical structure: o Essential if a compound is to have vitamin activity Any changes reduce vitamin A activity o Consist: Beta-ionone ring Oxidation o Reduce vit ac Demethylation o Reduce vit ac Side chain= Isoprenoid chain Length may affect the vitamin activity too long/ short lost activity Saturation o Unsaturated bond saturated may reduce activity Isomerization o Reduce the vit activity ** all these 7 structures are carotenoids as they can be found in colored plant, but not all of them are provitamin o Potency: For a chemical comp o be characterized as vit A, need 2 structures: o Beta ionone ring o Isoprenoid side chain For exp: o Beta carotene (most potent) In body, it will be split into 2 as it is symmetrical produce 2 vitamin A Because ut has 2 beta ionone rings, and the side chain can be divided into 2 o Alpha carotene The right ring is not original beta ionone ring has been hydrogenated cannot undergoes vitamin A activity only left side has the vit A activity not so potent compare to beta carotene which can produce 2 vit A o Beta-Cryptoxanthin Has the potential to bcm provitamin be converted into functional vitamin A in the body as it has a proper beta ionone ring o For lycopene, lutein, zeaxanthin not provitamin A They don’t have beta-ionone ring ** carotenoid can be classified as: o Provitamin A carotenoid Beta- carotene Alpha- carotene Gamma- carotene Beta- cryptoxanthin o Non-provitamin A carotenoid Lutein Zeaxanthin Lycopene ** we can’t say beta-carotene has the same potency as retinol Not 100% beta-ca consumed is absorbed & converted into retinol Hence the activity is ard 50% of retinol activity Requirement Affected by the potency of the ceratoid Hence we need to compare the reference= retinol retinol equivalent (RE) o 1 RE = 1ug retinol 6ug beta-carotene 12ug alpha carotene 3.33IU (international unit) RNI: o o o Metabolism Absorption o o Most at duodenum Not so effective as water-sol vit need to go through lymphatic circulation 1st b4 entering systemic circulation o All-trans Retinol is most preferred form for absorption highest absorption rate o Require lipid & bile salt Metabolism of retinol: o o o Retinol can be converted/reconverted into retinal But retinoic acid cannot be reconverted back to other form Transport o RBP (retinol-binding protein) Specific protein that binds with retinol to transport them frm liver to the rest of body Produced in the liver The binding of RBP started frm liver, during the absorption and transport to liver no RBP Once reach target tissue bind to the receptors sie on the cell membrane Receptors for retinol / retinoic acid Retinol is released frm RBP into the cell bound to intracellular binding proteins o o Deficiency In protein malnutrition children reduce protein reduce RBP synthesis Lead to Vitamin A deficiency Higher level of RBP In kidney disease Kidney breakdown & eliminate protein including RBP Lead to vit A toxicity even if vit A intake is above normal Function Vision o The production of rhodopsin in retina imp for adaptation of vision in the dark Rhodopsin regulated by how much light intensity enter our eyers Convert the light into electrical signal o All-trans retinol is transported (the only form) retina cell convert o all-trans retinal isomerized into 11-cis retinal combine with opsin frm rhodopsin Why transport as retinol? Retinol more stable The transport is by RBP only can bind with retinol Retinol is the storage form o Growth o Retinol, retinal, retinoic acid Cell differentiation o Retinol, retinal, retinoic acid Reproduction o Retinol o For the production of sperm Measurement Deficiency plasma retinol bleow 10ug/dl (0.3umol/l) ????? Toxicity Since Vit A may be stored in liver possible to develop toic condiciton when very high consumption (10 times than normal intake) Vit A intoxication is less likely with large intakes of carotene bcs the conversion is limited o But since it is pigmented yellowing of skin due to deposition of carotene in subcutaneous fat Hypervitaminosis A o Increased intracranial pressure Headached Blur vision Vomit Lack of muscular coordination o o Abnormal liver function Pain in weight-beaing bone & joints Inhibit excess vit D effect on renal calcification in general, antagonized the Ca response to Vit D excess vit D reduce retinol bound to erythrocyte membrane teratogenic (Any agent that can disturb the development of an embryo or fetus) cause CNS cranio-facial cardiovascular other defects ** contraindicated in pregnancy 怀孕禁忌 T4- Vitamin D Introduction vitamin D (calciferol) =the term referring to 2 mol o Ergocalciferol (D2) plant source Ergosterol (fat found in plant) + calciferol Most common form= D2 (ergocalciferol) Easier to produce as supplement Easily found in diet o Cholecalciferol (D3) animal source Cholesterol (found in animal) Most effective form of vit D Produced in skin Both types are equivalent in the effect of prevention of rickets Dietary D2, D3 biologically inactive o 2 Activation (hydroxylation) steps: Hydroxylation in liver Add a hydroxyl grp to D2 / D3 calcidiol (25-hydroxyvitamin D) o Not fully activated Hydroxylation in kidney Add another hydroxyl grp to calcitriol (1,25-dihydroxyvitamin D) o Fully activated form Food sources Animal source: (D3) o Fatty fish o Fish Liver oils o Beef liver o Cheese o Egg yolk Plants source (D2) o Mushroom To increase D2 in them treat with UV radiation Fortified food: (with D3, but sometimes with D2) o Milk o Plant milk o Cereal Supplement o Mostly D3 Vit D in food are fairly stable, not prone to losses via cooking, storage or processing nomenclature & structure D vitamins listed are a family of seco steroids that differ only in structures of their side chains o Seco-steroid bcs normally steroid has 4 ring, vit D only has 4, but one of them is broken Pathway of formation of Vit D3 (precursor activated form) o UVB (ultraviolet B) radiation on 7-dehydrocholesterol (found in skin) convert to previtamin D3 unstable preD3 stabilized by rearranging via thermal isomerization stable vit D3 diffuse from skin to blood o o o o o 7-dehydrocholesterol Synthesized In skin’s sebaceous glands secrete onto skin’s surface Activated by UV previtamin D3 UV trigger the opening of B-ring only then this comp is considered as vitamin D related compound to have vitamin activity Previtamin D Only have 2 double bonds To be a real vit D vitamin activity Hydroxyl grp at C-3 + presence of 3 conjugated double bonds Activation (blue) hydroxylation Liver 25 o 2-5X potent than D3 Kidney 1,25 o 5-10X potent than D3 24,25 o Inactive form o May be excreted by kidney into urine Requirement Active vit D is given in IU o 1 IU uses D3 as reference standard 1g cotton seed oil solution of D3 contains 10mg of the vitamin Elder need more vit D o Skin conversion and production of Vit D reduce Sufficient amounts of vitamin D are thought to be obtainable by exposure to sunlight for about 5 to 15 minutes between about 10 a.m. and 3 p.m. Other factors: o Season of the weather o Altitude o Skin complexion Melanin block YVB rays o Disease lead to fat-malabsorption Crohn’s disease Pancreatitis Liver disease RNI: o o o o o metabolism Absorption o o o o o o Absorbed passively with food fat & dependent on presence of bile salts No digestion needed Absorbed with LCFA packed in chylomicrons lymphatic system blood Primarily: Jejunum Ileum Form: Hydroxylated Unhydroxylated Renal disease & excessive amt of sun blocker / lack sunlight exposure Synthesis of D3 impaired Depend more on the dietary vit D3 intestine uptake of active form of Vit D Transport o o o o o Mainly by Chylomicrons (main source from diet) DMP (mainly when vit D is processed in the body) Vit D from chylomicrons is transferred to DMP (vitamin D-binding protein) o All forms of Vit D can be carried by this protein To: Adipose tissue, muscle, other tissue remaining back to liver Obese ppl tend to store more vit D low vit D in obese need higher doses to reach appropriate serum conc than normal weight Metabolism in liver Hydroxylate vit D to 25-OH D calcidiol by Cytochrome P-450 hyroxylase Mostly secreted into blood by DMP Little remain in liver blood is the largest major storage site of calcidiol ½ life = 12 days -3 weeks ** circulating serum calcidiol conc reflect vit D status Storage form: 25 hydroxyl D3 calcidiol In blood, some maybe taken up by other tissue like adipose for storage Accumulate in liver, kidneys, lungs Kidney uptake of calcidiol is stimulated by PTH convert to active form calcitriol released to blood for other tissue use o PTH secreted when serum Ca is low o High serum Ca & P inhibit calcitrol synthesis Calcitriol X accumulates This active form X stored but found in almost all cell & tissue type High calcitriol may stimulate the inactivation Upregulate 24-hydroxylase form 24,25- (OH)2 D from calcidiol excrete in feces Function Their mechanism involve genomic & nongenomic o Calcitriol increase absorption of Ca due to: o Calcitriol after syn in kidney, travel to enterocyte, get into their nucleus, upregulate specific genes encoding for protein involved in Ca uptake & transport synthesis of Calbindin (calcium-binding protein) o Elicit a change in membrane permeability to Ca at the brush border Induce expression of Ca-ATPases & Ca channel transporters in enterocytes Induce uptake of phosphate & Mg by brush border of intestine o Increase protein binding to Ca & phosphate (similar mechanism as for Ca) o The Ca binding protein unintentionally bind with Mg (with lower affinity) Bone mineralization o When PTH & calcitriol present in low conc The deposition of minerals into the bone (Ca) o When high conc promote resorption of Ca & P from bone to restabilize serum Ca Deficiency: o Rickets in children o Characterized: Seizure Growth retard Failure of bone mineralization o Enlarge of bone at wrisk, ankle, knees The cartilage gorw and enlarge without replacement by bone matrix and minerals Reduce calcification of bone skeletal deformities bone pain, muscle weakness Adults osteomalacia Low vit D and calcium conc increase PTH increase bone mineral resorption The bone matrix is preserve, but remineralization is impaired soft bone Bone pain , muscle weakness Vit D help to regulate muscle contractility by regulating Ca uptake and secretion Ricket vs Osteomalacia vs Osteoporosis Osteoporosis o Bone is thin & brittle due to too little mass o But the mineral & composition is normal o Deficient of Ca Osteomalacia o Total mass normal o But lack of mineralization o Deficient of Vit D Measurement Main indicator: o 25-hydroxyvitamin D (calcidiol) in serum o normal value= 27.5 nmol/L o longer circulating ½ life = 15days calcitriol not goof indicator toxicity storage capacity of liver for D precursor is much less than its capacity for A o hard to get toxicity frm natural source o supplement risk symptom: o excess calcification not only of bone, but also in soft tissue kidney, heart, lungs, blood vessel o hypercalcemia, hyperphosphate renal dysfunction o hypercalciuria o urinary Ca stone o anorexia o nausea o vomiting o thirst o polyuria o muscular weakness o joint pain o disorientation o death T4- Vitamin E Introduction 8 naturally occurring forms of Vit E syn by plants (vitamers) Common structure: o Phenolic functional group on chromane ring (head) o Phytyl side chain (tail) 8 vitamers Divide into 2 classes o Tocopherols (4) Have saturated side chain with 16 carbons o Tocotrienols (4) Have unsaturated side chain with 16 carbons Each clasees has 4 vitmaers o Each dif in the number & location of methyl frp on the chromanol rings o They cant be interconverted o Alpha-tocopherol most biological active Food sources Found in many dif food both animal and plant, but more amt in plant Found mostly in frm plant Esp oil of plant o Wheat germ oil o Palm oil (tocotrienol> alpha tocopherol) Animal source o Primarily alpha-tocopherol o Higher-fat meat o Less good source of vit E Susceptible to process o What germ is removed in milling white flour o Oxidized when exposed to air, light, heat Roasting nuts reduce vit E content Alpha-tocopherol highest biological activity nomenclature & structure Most active naturally occurring form= alpha-tocopherol o Alpha-tocotrienol highest activity among the tocotrienol o Alpha-tocopherol highest activity among all 8 forms of vit E Consist of: o Double ring structure o Side chain at C2 (differential tocopherol / tocotrienol) Tocopherol= X double bond (saturated) Tocotrienol = have double bond (unsaturated) o 3 methyl grp (5, 7, 8) <at least 1 methyl grp> dif no. or place of methyl grp differentiate the tocopherol / tocotrienol Tocopherol: o Alpha = 3 o o o Beta= 2 (5, 8) Gamma =2 (7,8) Delta= 1 (8) o ** all forms have 1 OH- at C6 1 CH3- at C8 Isomers/ synthetic Vit E o Commercially available products as acetate / succinate ester ** ester X usually occur in nature o Uncommon to have vit E deficiency than other vit may be due to mal function of Vit E production/absorption (fat- malabsorption) o tocopheryl acid succinate is more effective 0.89 Requirement IU of vit E activity activity of 1 mg of alpha-tocopherol acetate = reference standard o Though a-tocopherol is 36% more active than acetate still use acetate as reference o Bcs: readily available as a standard comparison Hard to determine the requirement o Vit E = antioxidant the requirement may be affected by the antioxidant present in our body Eg: Selenium , vit C o The PUFA level in body Increase PUFA increase the need of vit E RNI? Metabolism Absorption o o o o o Free tocepherols no need digestion Esterified tocotrienol or supplement need digestion Pancreatic esterase and bile-dependent mucosal esterase hydrolyze tocotrienols & syn ester alpha-tocophenol lymphatic system lipoprotein complex Enhance by presence of fat in intestine Esp SF Decrease by PUFA Most at jejunum & ileum Via diffusion across enterocyte membrane Transport o o o o o o Absorbed vit E incorporated into chylomicrons liver B4 entering liver, tocopherl can be transferred among other lipoprotein HDL, LDL LDL posses highest con tog tocopherol Intracellular transport Alpha-tocopherol-binding protein alphaTTP Synthesize in liver Found in hepatic cytosol heart transfer alpha-tocopherol into VLDL distribute to other tissue reaching into ather tissue ATTP are needed to bind ti vit E for intracellular transport into membrane deficient of ATTP vitamin E deficiency Reservoirs: Adipose tissue (over 90%) Increase with increase dosage of vit E Other tissue relatively stable conc Muscle Liver If diet Vit E not enough, use the reservoir until deplete Rate of depletion with dietary inadequacy varies considerably o Affected by other antioxidant Found in all cells Mostly in Adrenal cell Testicular cell Increase intake of b-carotene & Vit c protect a-tocopherol depletion Increase PUFA increase need for antioxidant Function o Antioxidant (main) o Function is shared with affect requirement of Vit E frm diet b-carotene, ascorbic acid regenerate vit E following its oxidation Se-dependent glutathione peroxidase Cu-Mn-Mg dependent superoxide dismutase o ** the one with higher conc may cover/compensate the deficiency effect of the other one o ** beauty product add vit E as antioxidant Maintaining membrane integrity of body cells o Prevent oxidation of unsaturated FA of phospholids of membranes Tissue with cell membranes more susceptible to oxidation Lungs Brain RBC o Expose to high conc of O2 Correct damaging effect of Free radicals on DNA o In steroid hormone syntheses o Spermatogenesis infertility pherol= birth Protect RBC o The enzyme glutathione peroxidase (selenoenzyme) activate by vit E acting as free radical scavenger protect hemoglobin & cell membrane frm oxidation by free radical Prevent oxidation of LDL o Prevent CVD Measurement Use a-tocopherol as indicator (have 8 members) Toxicity Least toxic vitamin High doses acts as antagonist to vit A,D,K Symptom: (>900mg/kg of the diet) o Headache o Nausea o Muscle weakness o Double vision o G disturbance o Increase bleeding Due to anti-platelet effect Deficiency Cause o Premature infant o Fat malabsorption disorder Cystic fibrosis o Genetic ATTP deficiency Consequence o Infertility in men Vit E imp in production of sperm o T4- Vitamin K Introduction 3 classes: (2natural + 1synthetic) o K1 (phylloquinone) Found in plants o K2 (menaquinones) Synthesis by intestinal bacteria o K3 Synthetic form Will be converted into K2 by microbiota Normally, newborn is injected with vit K bcs the intestine is sterile X syn vit K needed for normal blood clot prevent VKDb (bleeding)= hemorrhage disease Source: K1 major source of dietary vit K in human diet Plant: o Green leafy vege? Nomenclature & Structure: Structure give vit K activity: o 2-methyl-1,4- naphthoquinone Structure requirement: o A methyl grp at C2 o Side chain at C3 Can be vary in length Affect vitamin activity o If K1 & K2 have same length of side chain similar activity o There is an optimal length for optimal activity 20 carbon side chain Any length greater / shorter than 20 will have less vit K activity Affect vitamin potency o Potency vs activity: o Drug A is more potent than B o At the same response magnitude, A is needed in less dose than B Drug B is more efficacy than A o o o B has a higher maximum response magnitude than A Activity= efficacy= the max effect to be achieved by a specific concentration Higher potency, need lesser amt to exert the effect The higher the comparative potency, the more potent it is, the lesser amt needed to give the effect. Benzene ring must be unsubstituted Can exist in cis or trans configuration All trans-phylloquinone = naturally occurring form Mixture of cis & trans forms: Synthetic phylloquinone Requirement: Since our microbiota can synthesis vit K , hard to set a requirement and is variable USA suggest: 30-100ug/d o Esp for long-term antibiotic treatment Absorption: Most of the fat-sol vit are absorbed befor reaching large intestine, except for vit K o Bcs production of vit K is at LI, specifically the colon ?? K1 & K2 use transport process K3 passive diffusion Site: o K1 small intestine (from diet, most nutrients absorbed here) o K2 ? o K3 in large intestine bcs need to be ocnvered by microbiota to K2 first Function Blood coagulation o Promote synthesis of GLA in the liver (G-carboxyglutamic acid) GLA essential part for prothrombin (coagulation factor II) and other coagulation factors (VII, IX, X) With no vit K no GLA not factor II, vII, IX, X ????? o Involves 4 phases that must interdigitate if a clot is to be formed Formation of thromboplastin Activation of thromboplastin o Formation of thrombin Formation of fibrin Involve many substances / coagulations factors 4 out of 13, associated with vitamin K Osteocalcin o Carboxylated protein that contain Gla found in bone matrix Since Gla need vit K for synthesis o Synthesis in bone tissue (osteoblast) Highest during rapid growth ??????? Deficiency Rare as body can produce Only due to secondary vit K deficiency delayed / prolonged clotting time o Biliary disease diseases affecting the bile ducts, gallbladder and other structures involved in the production and transportation of bile fat malabsorption affect vit K absorption o Long-term broad spectrum antibiotic therapy Kill microbiota o Anticoagulant therapy using warfarin Prevent blood clot in blood vessel Warfarin is one of the anticoagulants o Interfere the function of vit K = anti-vitamin K o Vit K affected X produce that 4 coagulation factors X blood coagulation Used as rodenticide o Colorless, odorless, tasteless put in food let the rat eat hemorrhage excessive bleeding Symptoms: o Numerous bruises (subcutaneous hemorrhage to injury) Toxicity: Large intake of naturally occurring vit K X toxic Supplements of vit K X be taken with warfarin T4ii- water-soluble vitamin Cannot stored in body, need to consume enough amt daily Exp: o Thiamine o Riboflavin o Niacin o Pantothenic acid o Pyridoxin o Biotin o Folic acid o Cyanocobalamin Though they are classified under vit B dif chemical and structures dif function All 8 vit B always present in the same food Thiamin B1 Structure: o Consist of: Pyrimidine ring Thiazole moiety Contain a sulfur atome o Linked by a methylene bridge (CH2) Food source: Animal: o Phosphorylated form 95% Thiamin diphosphate (TDP) = thiamin pyrophosphate (TPP) 5% thiamin monophosphate (TMP) & thiamin triphosphate (TTP) o Meat (esp pork) Plant: o In free nonphosphorylated form o Legumes, grain (whole, fortidied, enriched) o Yeast o Wheat germ o Soy milk Supplement: o Thiamin hydrochloride o Thiamin mononitrate salt Process susceptibility o Destroyed primarily at methylene bridge by Alkaline Heat o Cooing thiamin-rich food in water promote loss of thiamin Nomenclature & structure A pure vit B1 form is unstable Can present in 3 dif form in body: Thiamine pyrophosphate (TPP) o 80% exist in cells Requirement: o o o Thiamine requirement are related to energy metabolism Factor : o Age o Caloric intake o Carbs intake o Body weight o Presence of infection o Men > women Due to body size and energy needs Metabolism: Absorbed by o Passive diffusion With high thiamin intake, passive diffusion pre-dominate o a specific active transport mechanism Thiamin transporter ThTr1 & ThTr2 ** alcohol inhibit intestinal expression of ThT2 inhibit thiamin absorption o Most rapid in duodenum Phosphorylated form: o Need to hydrolyze the phosphate from TDP, TMP, TTP to free thiamin b4 absorbed into enterocyte o In enterocyte Thiamin may be phosphorylated back o Only TMP / free form can cross the cell membrane Absorption rate: o High o Affected by antithiamin factors destroy thiamin Thiaminase in raw fish Reduced with cooking Polyhydroxyphenols Tannic Caffeic aicd o Thiamin destruction is prevented by reducing agent Vit C Citric acid Transport o In plasma Free form bound to albumin TMP 90% of thiamine in blood is present within RBC as TDP (formed within the cell) Liver: o Most free thiamin is taken up by liver phospholyrated to TDP= TPP (coenzyme form) o 80% OF TOTAL Thiamin in body is TDP= TPP o Thiamin X present in their free form in our body Body X store the vit need daily supply Function: Coenzyme role in energy transformation o As TPP= TDP o Not directly act in the function, but needed for the activity to run o Coenzyme for oxidative decarboxylation of: generate energy (ATP) Carbohydrate metabolism Pyruvate acetyl CoA o Happens b4 the citric acid cycle In kreb cycle o Alpha-ketoglutarate succinyl CoA Fat metabolism BCAA o Coenzyme of BCKDH Alcohol metabolism The same enzyme convert pyruvate acetyl CoA also convert acetaldehyde acetyl CoA Deficiency: Due to malabsorption & poor diet intake o Beri beri = weakness Types: Dry o Predominantly in adult o Due to low thiamin intake + high carb intake o Characterize: Muscle weakness & wasting , esp lower extremities Peripheral neuropathy Affect nerve conduction in limbs paralyze Wet o More extensive cardiovascular system involvement than dry o Edema of heart failure o Digestive disorders Acute/Mixed o Mostly in infant o Characterize: Anorexia Vomiting Lactic acidosis Cant conver pyruvate to acetyle-CoA pyruvate onlyc an be converted into lactic acid Neural & cardiac symptoms Clinical manifestation varies depend upon the severity of deprivation Due to chronic alcoholic o Why? Reduce vitamin intake due to reduce food consumption Increase requirement due to liver damage Main site of thiamin phosphorylation TDP=TPP o Wernicke-Korsakoff syndrome (dry beri beri) Due to their poor diet Characteristic Wernicke’s encephalopathy: o Confusion o Low lvl of consciousness o Poor coordination Korsakoff’s psychosis o Happen when Wenicke is not treated o Brain damage Memory loss o Mechanism: Malnutrition frm poor diet Decrease ability of duodenum absorption of vit B Result in Impaired Krebs’s cycle XATP production brain X enough ATP brain damage Enzyme involved: o PDH o Alpha-KGDH Measurement Red cell Transketolase o Thiamine is the cofactor of this enzyme o Low transketolase activity low thiamin Toxicity Dietary/oral intake B1 rare Most injection of B1 3g/d symptom o Headache o Irritability o Insomnia o Weakness & tachycardia Riboflavin B2 Name: o Ribo = ribose-like side chain o Flavin = yellow color Structure: o Flavin mol Isoalloxazine ring o Sugar alcohol side chain Ribitol side chain Forms: o 2 coenzyme derivatives FMN (flavin mononucleoide) FAD (flavine adenine dinucleotide) Food source Source: o Animal source: (most!) Dairy product !! Milk, meat, eggs o Plant Wheat germ Fortified cereal/ flour o Human production Microbiota can produce small amt of b2 but not enough to meet dietary need Form in food o Free o Protein-bound o In the form of coenzyme FMN, FAD Used immediately & X stored in body o Excess amt are excreted in urine o Bright yellow color urine! Source in diet is unstable o Exposed to UV light Up to 70% will be lost frm milk during 4 hr exposure to sunlight That’s why packaging of milk is not transparent glass anymore o But resist heat, oxidation, acid Nomenclature & Structure C7 & 8 must be substituted with more than just a hydrogen Amine grp at C3 must be unattached A ribityl group at C10 o Most imp that contribute to vit B activity o Solubility o Can be enhanced when solvent pH increase (alkaline) When pH increase, the stability towards UV & heat will decrease/ too acidic deactivated easily The ribityl grp is lost during deactivation no vit activity at all o ** Riboflavin must be protected from light and acid Requirement There is almost no riboflavin reserve daily intake is essential Imp for pregnancy! o B2 deficiency may lead to congenital birth defect Heart defect & limbs deformation Absorption All 3 sides of SI can absorb o Max absorption in jejunum of SI o Significant uptake by duodenum & ileum B2 found in food maybe o Attach to protein Must be freed to be absorbed by: HCL , gastic & intestinal enzyme hydrolysis of protein o Phosphorylated form of coenzyme FAD, FMN Must be dephosphorylated in intestinal lumen free to absorb Pyrophosphatase cleave FMN , FAD Alkaline phosphatase liberate vit frm its coenzyme form By active carrier o Energy & Na dependent o RFT2 Factor: o Bile facilitate absorption Small amt of vitamin circulate via enterohepatic system o Alcohol impair B2 digestion & absorption Enter enterocyte before enter portal blood o Rephosphorylated to reform FMN, FAD bound to albumin and transport in plasma The initial phosphorylation reaction is Zn-dependent o Circulate in blood bound to plasma protein, albumin Function coenzymes that involve oxidation-reduction o o Flavin act as oxidizing agent Ability to accept a pair of hydrogen atom Most are oxidase/ reductase Many of these enzyme involved in mitochondrial respiration ATP synthesis Mitochondrial citric acid cycle They are also called= flavoproteins Eg: Succinate dyhydrogenase its activity = biomarker of riboflavin intake sufficiency Acyl-CoA dehydrogenases fatty acid oxidation Hence riboflavin is essentially needed in regulation of metabolism Contained in flavoproteins o Involved in many oxidation-reduction reactions in many metabolic pathway Serve as intermediate electron carrier with NADH Deficiency =Ariboflavinosis Rarely occur Symptom: o Poor growth o Poor appetite o Skin lesion Outside of the lips = cheilosis Corner of mouth = angular stomatitis Measurement Hard to Urinary excretion Measurement of erythrocyte glutathione reductase activity coefficient (EGRA) o FAD is co-factor for EGR reflect long-term riboflavin status o Activity coefficient: Represent a ratio of enzyme’s activity with FAD to the enzyme’s activity without FAD o When addition of FAD stimulate enzyme activity to generate an AC of 1.3-1.4 low riboflavin status > 1.4 = deficiency o When FAD added, AC <1.3 acceptable Niacin B3 Introduction: Discovered due to pellagra 糙皮病 o characterized by dermatitis, diarrhea, and mental disturbance, and is often linked to overdependence on corn as a staple food. Niacin is a generic term for o Nicotinamide o nicotinic acid o 2 forms in food different physiological properties o Both are very stable in dry form o But amide More soluble than acid Most supplement is amide form in solution readily hydrolyzed to acid form Abt 50% of niacin in body is syn frm AA tryptophan Work in body as coenzyme with more than 400 enzyme dependent on it for various reactions Source: Widely distributed in human food supply o Esp: Best= fish & meat Whole grain cereal Bread Milk Egg Vege that are richly colored Form in food o Animal: o nicotinamide o nicotinamide nucleotide NAD (nicotinamide adenine dinucleotide) NADP (nicotinamide adenine dinucleotide phosphate) Plant: Nicotinic acid We cant get B3 from corn o bcs it is bound covalently to the protein (niacinogens) or complex carbs (niacytin) Reduce availability o But with some process, the B3 is freed from the protein Chemical treatment with bases like lime water Exposure to gastric acid Exp: tortilla Endogenous Synthesis o In liver, from tryptophan o Is an imp contribution to the niacin needs of the body o o Need Fe & PLP (vit B6) Deficiency of these nutrient impair niacin synthesis Nomenclature & structure 2 forms: o Nicotinic acid o Nicotinamide More soluble in water > nicotinic acid Very stable in dry from o But amide form is readily hydrolyzed to acid in solution Mainly appear as coenzyme forms in body o X appear as free form Important structure: o Pyridine ring o Carbon 3 is substituted with side chain Beta-carboxylic acid nicotinic acid Amide nicotinamide o Open sites at pyridine carbons 2-6 Requirement: Hard to give an exact level bcs is affected by protein level as well Low protein diet increases the need for niacin o Tryptophan can be converted into niacin Niacin equivalent= 1mg niacin= 60mg tryptophan RNI o Metabolism NAD & NADP need digestion to nicotinamide before absorbed o Both forms of niacin are absorbed into enterocyte by o Simple diffusion High conc, completely by passive diffusion o Facilitated diffusion ** B1 & B2 are absorbed by active transport Vitamin circulates in blood in its free form o Mostly nicotinamide free form Some bound to plasma protein o Free form may diffuse across cell membrane uptake by tissue But some tissue need carrier for nicotinic acid transport Kidney tubule RBS Need energy brain o If not converted into NAD+ / NADP+ (coenzymes) will be metabolized further and excreted in the urine In tissue: o Amide / acid are used to syn NAD NADP NAD usually found as its oxidized form NAD+ NADP mainly reduced form NADPH Function: NAD, NADP are coenzyme of primarily dehydrogenases o Act as H donor or E- acceptors o o o Nicotinamide is incorporated into these coenzyme Involved in many oxidoreductase reaction Glycolysis FA metabolism Tissue respiration Detoxification Folate coenzyme synthesis Used as drug in clinical as lipid-lowering drug o Nicotinic acid o Niacin inhibit TG synthesis, lowering serum TG o Doses of 1-2g/day are used in the treatment of hyperTG & hyperchol Deficiency: Vitamin deficiency scale great concern o Quite a big concern compared to other vit B Pellagra o Pelle= skin, afra= rough 4 Ds – dermatitis, dementia, diarrhea, death o Dermatitis Skin exposed to sun inflamed progress to pigmentation, cracking, peeling Casal’s collar o o Diarrhea Often accompanied by inflamed tongue Dementia Symptoms range frm mild confusion & disorientation mania Measurement Metabolites NMN (N’-methylnicotinamide) * N’-methyl-2-pyridone-5-carboxamide o Need 24hr urine collection o NMN to creatinine ratio = <1.5mmol/mol deficiency o This metabolite is directly proportional to niacin level in body Concentration of NAD in red cell o NAD= coenzyme form of niacin Fasting plasma tryptophan Toxicity: Chronic administration of 3g/day o Theoretically, niacin is to produce ATP can boost up energy level But if you take more X make your body stronger o It’s hard to get toxicity as it can be excreted in urine Too much vasodilatory side effect Symptom: o Headache o Heartburn o Nausea o Hives o Fatigue o Sore throat o Dry hair o Inability to focus the eyes o skin tautness 紧绷 Pantothenic acid (B5) CoA Introduction: panto = everywhere consist of o 2 component: beta-alanine pantoic acid o joined by: peptide bond o used to form a part of coenzyme A o A = acetylation o source widely distributed in food o but highly processed food X contain the vitamin excellent source: o organ meat !!! o mushrooms o avocado o broccoli o whole grains when it is processed to produce refined grain (white rice, flour) no B5 B5 is found at the outer layer of the whole grain Food process: o Destroyed easily by heating & freezing Nomenclature & structure Only has 1 chemical compound (others got many) Form o Free acid o Supplement Calcium salt Unstable pale yellow oil Or commercially available as white stable, crystalline Ca / Na salt When dry, salt is stable to air & light but is hygroscopic 吸湿的 Readily destroyed by o Heat Hydrolytic cleavage of the mol produce Beta- alanine 2,4-dihydroxy-3,3-dimethyl butyrate o alkaline/acid pH Requirement gut bacteria can produce B5 but not enough to meet daily need o hence info is X available to derive recommended intake Metabolism Form in food: o Bound as component of CoA CoA need to be hydrolyzed free B5 o Free Passive diffusion When high amt Facilitated diffusion When Low amt intake SMVT (sodium-dependent multivitamin transporter) o SHARE with biotin, lipoic acid Transport o Diffuse into blood travel in 2 forms travel to liver and other cell Free Within RBC (most) o Tissue high in B5 (used for CoA) Liver Adrenal gland Kidney Brain heart Large doses of B5 / after its release from CoA rapidly excreted in the urine Function o Part of coenzyme A (CoA) o Imp in citric acid cycle = kreb cycle o Essential for reaction involve carbs/ lipid metabolism o B5 is the backbone of CoA, but not serve at CoA active site Still imp la cuz no B5, no CoA no need memorize o Toxicity Not been described in human as single entity Large dose GI symptom Deficiency: If it occurs, accompanied by other deficiency disorder as well Increase need o Alcoholism o DM o IBS Symptom o Burning feet syndrome Numbness of the toes & sensation of burning in feet Pyridoxine B6 3 naturally occurring forms: (inter-convertable) 1. Pyridoxine (alcohol) PN Plant source 2. Pyridoxal (aldehyde) PL 3. Pyridoxamine (amine) PM Last 2 Animal source more potent precursors for coenzymes pyridoxal phosphate (PLP) & pyridoxamine phosphate (PMP) o To have the activity, need to be phosphate Each has 5’-phosphat derivative Food source: Plant 1. Form: pyridoxine PN 2. Stablest form 3. Its; phosphorylated form PNP found exclusively in all plant food 4. Some in conjugated form pyridoxine-glucoside animal 1. PD, PM, their phosphorylated derivatives 2. Not so prevalent than plants Food process: 1. Fairy stable with cooking 2. Destroyed by: Prolonged heating (sterilizing & canning) Milling & refining of grain Nomenclature & Structure B6 Is the generic descriptor for all methyl-3,5- dihydroxymethyl pryridine derivatives Imp structure for B6 activity 1. Phosphorylated at 5-hydroxymethyl grp Hence, need to be added with phosphate to have the coenzyme activity 2. C4 substituent must be convertible to aldehyde form Pyridoxal = aldehyde form dy Need 1 more step to activate o Add 1 phosphate at C5 Pyridoxine & pyridoxamine= not aldehyde form but can be interconverted Need 2 steps: o Change C4 aldehyde o Add 1 phosphate at C5 Pyridoxine HCl 1. Synthetic form of B6 2. Stable to light & heat in acid solution But unstable in neutral & alkaline solution Pyridoxal 1. Aldehyde form is much less stable 2. Instability to heat major concern in food process 3. Moreover, most food rich in B6 is neutral slightly alkaline Make them even more unstable 4. Esp concern: infant formula Infant formula needs to undergo autoclave to kill food borne pathogens Requirement B6 is imp in AA metabolism requirement are linked to protein intake Metabolism Phosphorylated must be dephosphorylated 1. Done by Zn-dependent alkaline phosphatase & intestinal phosphatase at brush border 2. PN, PL, PM Pyridoxin glycoside hydrolyze to be freed Absorption 1. Preferably free form 2. Phosphorylated form If ingestion of high amt of phosphorylated from Uptake by passive diffusion X active transport special (jejunum, ileum) 1. B1,B2, B5 active transport In enterocyte 1. Some may be phosphorylated to PNP, PMP, PLP Carried by RBC to all cells tightly bound to protein (hemoglobin & albumin) Significant amt of vit B6 may be found in liver, brain, spleen, kidney, heart but not stored In liver: Unphos phos PNP, PMP PLP (main vitamer) 1. By FMN-dependent oxidase Need riboflavin In blood: PLP is the main form of the vitamin found in systemin blood 1. Mostly bound to albumin Since only unphos vitamers may be taken up by tissue, PLP typically hydrolyzed prior to cellular uptake Function PLP coenzyme In reaction whose substrates contain nitrogen amino acid 1. transamination Produce keto acid & synthesis of NEAA 2. Decarboxylation (removal of COO-) Yield bioactive amines Neurotransmitter (NE, E, serotonin, dopamine, GABA) Histamine 3. Porphyrin synthesis Coenzyme in the 1st step in synthesis of heme Hemaglobin 4. Niacin synthesis From tryptophan PLP-dependent reaction 5. Cysteine synthesis Cystathionine synthase & lyase ate PLP-dependent enzyme PLP for transulfhydration Homocysteine cysteine Glycogen degradation PLP is needed for glycogen phosphorylase to catabolize glycogen glucose-1-PO4 Hence most PLP in muscle is bound to glycogen phosphorylase Deficiency Target: 1. Infant with severe heat treatment infant milk Form PLP=lysine little vitamin activity Sign: Seborrheic rash on face, neck, shoulder, butt Esp: seizure, convulsion 2. Elderly Poor intake of vit B6 Accelerate hydrolysis of PLP & oxidation of PL 3. Alcoholics Impair conversion of PN, PM PLP Acetaldehyde enhance coenzyme degradation Other sign 1. Weakness, fatigue 2. Cheilosis, glossitis 3. Sideroblastic (Microcytic, hypochromic) anemia Due to impaired heme synthesis 4. Impair niacin synthesis from tryptophan 5. Inhibit metabolism of homocysteine Hyperhomocysteinemia Toxicity: Loss of sensation in feet Peripheral neuropathy Daily dose: 1. Not exceeding 10 mg/d measurement Plasma conc of pyridoxal phosphate PLP 1. Normal : above 30nmol/L Total vitamin B6 Biotin B7 skin Found out due to egg white injury 1. Eating raw wgg white causes hair loss, dermatitis 2. Found out biotin can cure this 8 isomers 1. Only D-biotin is biologically active Source 1. Diet 2. Gut microbiota syn in colon Food source: Found in every living cell in minute amt 2 forms: 1. bound amino acid lysine biocytin Protein bound Glycoprotein bound o Avidin in raw egg white Heat labile can be destroyed with cooking no adverse effect on biotin absorption o Irreversibly bound to biotin prevent absorption Need to hydrolyze frm the form to be freed to absorb 2. Amide Free form Natural form Rich source 1. Organ meat 2. Egg yolk 3. Brewer’s yeast 4. Royal jelly Other 1. Soy flour/ soybean 2. Ocen fish 3. Whole grain 4. Human milk Nomenclature & structure: Name: cis-hexahydro-2-oxo-1H-thieno (3,4-d)imidazole-4-pentanoic acid Imp structure: 1. 2 ring: Ureido ring Thiophene ring 2. Side chain Valeric acid Requirement Difficult to determine 1. Can be form by gut 3-7mg is consider adequate Metabolism Can exist in food in 2 form 1. protein bound need to be digested proteolysis by pepsin & intestinal proteases free biotin, biotinyl peptide, biocytin biocytin hydrolyzed by biotinidase lysine + biotin genetic disorder of biotinidase deficiency biotin deficiency Not all will be hydrolyzed less than 50% of plant origin (low conversion rate) animal origin more readily available > plant 2. Free Absorbed readily Absorption 1. Form: Free Some biocytin, peptide-bound 2. Mechanism: facilitated diffusion when high dose (pharmacologic foses as needed with some genetic disorder) carrier mediated SMVT o Shared with pantothenic acid & lipoic acid In blood 1. travel to liver bound to liver plasma membrane receptor (SMVT) 2. form: unbound , free (~80%) bound to plasma protein storage: 1. stored in small quantities in muscle, liver, brain Function Coenzyme of several carboxylic enzyme biotin is covalently bound to some types of carboxylases Involved in nutrients metabolism 1. Gluoconeogenesis 2. Fatty acid synthesis 3. Amino acid catabolism 4. Protein synthesis: keratin Found mainly in mitochondria and cytoplasm 1. 2. Serves as mobile carboxyl carrier When it is attached to enzymes that catalyze carboxyl grp transfer Bound covalently to histone (DNA-binding proteins) Bound to histone tail regulate gene expression 1. Biotinylation of histone tail histone uncoil expressed Maintain DNA structure Hair, skin, nail Biotin improve body’s keratin infrastructure Deficiency Extremely rare in normal population 1. Can be syn by intestinal bac Cause 1. Long-term eating raw egg reversible 2. Defective biotinidase enzyme 3. Alcoholism Impair biotin absorption Symptom: 1. Dermatitis 2. Skin rash 3. Hair loss, alopecia 4. Developmental delay 5. Seizure 6. Conjunctivitis 7. Visual & auditory loss Complication 1. Reproductive failure 2. Impair growth & development of fetus Measurement: Available in whole blood or urine Normal range: 1. Whole blood: 0.22-0.75 ug/ml Toxicity No report Cause diarrhea due to large doses Other: Certain supplement high in biotin is stated: 1. Can promote the health of hair, nails, skin 2. Cause biotin can improve body’s keratin infrastructure Beyond this, no further evidence liao hence not conclusion 3. But it can maintain the health of hair,nail,skin, not really improving B9 Folic Acid Discovery: 1. Folate + vit B12 cure megaloblastic anemia Folic acid 1. Tho it is synthetic form , not it is more available for absorption and stable 2. 85% absorption rate Folate 1. Natural form 2. Commonly found in many food 3. Folate folium= leaf Food source Both plant and animal origin Exp: 1. Meat liver 2. Frutis 3. Vege Esp asparagus 4. Dru beans 5. Peas 6. Nuts 7. Whole grain cereal Food process: 1. Heat destroy folate Raw > cooked 2. Oxidation, UV Nomeclature & Structure: Important Structure for vitamin activity: 1. Pteroic acid a. Pterin ring b. PABA (para-aminobenzoic acid) 2. Glutamate Derivative of folic acid o Has dif subgrp at N5 & N10 o Requirement Human X produce own folate hence essential & highly needed o Required in daily diet o Though is available in many foods, but the absorption rate is 50% only Unless folic acid fortified la Women contemplating pregnancy (trying/ aldy pregnant) o Need increase intake 2X for folate o Metabolism absorption o Folate natural in food 50% bioavailability Polyglutamate form Up to 9 glutamic acid residues attached to PABA Mostly= 5-methyl tetrahydrofolate (5-MTHF) need to be digested to monoglutamate b4 absorbed By carboxypeptidase o Zinc dependent o Affected by alcohol Both Zn & alcohol impair polyglutamate absorption o Folic acid Monoglutamate 100% absorption o Absorbed form: Monoglutamate form 5-methyl THF o Carrier mediated 2 types of specific Folate binding protein Low affinity o At brush border membrane of absorptive cell High affinity o PCFT (proton-coupled folate transporter) o Mostly at duodenum & upper jejunum brush border cells o Absorption is reduced in alkaline, improved in acidic cond. within enterocyte: o Folic acid & folate reduced to dihydrofolate (DHF) reduced to THF (tetrahydrofolate) o circulation o as monoglutamate form (free form) Folate 5-methyl THF 10-formyl THF o Bound in RBC RBC X take up folate from the circulation, but the amt of folate Is bound to RBC during erythropoiesis RBC folate conc represent longer term folate status than plasma (2-3month) Uptake by tissue: o Carrier mediated RFC reduced folate carrier PCFT proton-coupled folate transporter In liver: o Glutamate is added polyglutamate form of THF storage form excretion o not used excrete in urine as pteroylglutamic acid 5-methyl-pteroylglutamic acid, 10-formyltetrahydrofolate, acetamidobenzoylglutamate. o Very little in feces Function: Coenzyme in one-carbon transfer (methyl group) o Activation needed for activity Need to be activated to bcm Tetrahydrofolate acid THF used as coenzyme o DNA & RNA synthesis: Imp in purine & pyrimidine & glycine syntheses o Other Methionine Genetic disorder: MTHFR o Coenzyme form of folate are interconverable o Except 5-methyl THF cannot be directly converted back to 5, 10-methylene THF MTHFR enzyme are needed to convert 5,10-methylene THF to 5-methyl THF Lack of MTHFFR reduce 5-methyl THF --. Reduce remethylation of homocysteine to form methionine But we can get 5-methyl THF naturally from diet, but not folic acid Interaction with other nutrients Vitamin B12 o Without vit B12, methyl group from 5-methyl THF cannot be removed trapped = methyl-folate trapped o Even enough folate intake X not in the form to be used for DNA synthesis Including: 10-formyl THF purine 5,10- methylene THF thymidylate Deficiency Megaloblastic macrocytic anemia o RBC is Lesser Larger Immature Shorter lifespan o Due to disrupt DNA synthesis & cell dividion Folate needed for purine & thymidylate synthesis dermatitis, impaired growth o Common in chronic alcoholics Alcohol prevent folate absorption Imp for development of embryo o Deficiency in pregnant women prior affect early stage of embryonic development lead to spina bifida & other neural tube defect A gap in the spine Not fully enclosed Measurement Recent intake is assessed by serum folate o Measure blood sample o Normal level: 2-11 ug/L Cellular status by red cell folate o Normal level 150-700 ug/L Toxicity Hardly as can be excreted by urine Cyanocobalamin B12 Discover due to it can cure pernicious anemia Complex mol that contain cobalt Commercial form o Cyanocobalamin Can be converted into natural form Source Found primarily from animal origin products Plant o fortified food la o contaminated with microbes from manure Unstable to o UV light o Acid o Metal (Fe, Cu) Stable to: o Light o Heat o Oxidation o Nomenclature & Structure Imp structure: o Cobalt-centered corrin ring Consist of 4 reduced pyrrole rings In the ring center Cobalt o At 3+ state o Can form up to 6 bonds Tightly bound to 4 pyrrole N atoms can bond a nucleotide & a small ligand below & above the ring respectively o Requirement Daily requirements is very small o Normal turnover rate = 2.5ug/day Hence recommendation for adult is close to turnover rate or 2 ug/day o Body gut microbiota can synthesis but not enough for need Strict Vegetarian & vegan take note of B12 intake since X take in animal products Pregnancy: o Increase need for B12 for growth & development of infant Need for DNA & RNA synthesis Metabolism (4 binding protein) Vit B12 in food is bound to protein o B12 is in complex form of protein In stomach o Pepsin + Acid dissociate B12 frm protein o B12 bind to another protein heptocorrin (called R protein, produced in salivary gland) To protect B12 frm acidic pH in stomach & bacterial use In duodenum o R protein degraded by pancreatic enzyme + alkaline environment free B12 In acidic environment vit B12 is prefereably bind to R protein > IF o B12 bind to another protein , intrinsic factor (produced in parenetic cell of stomach but escape digestion) IF is imp for absorption by intestinal cell No IF no absorption In ileum o IF + B12 complex bind to IF receptor = cubilin take up by intestinal cell Active transport Defect of cubilin B12 malabsorption In enterocyte: o Vit B12 released from IF complex o Transported to portal blood bind to mainly transcobalamin 2 (produced by ileum mucosal cell) Or other TC1, TC3 Large intestine o Small absorption happen here o Mostly are those produced by gut microbiota o Passive transport Trqnsport in blood o Transcobalamin II Genetic disorder SNP Reduce TC ability to bind with Vit B12 for distribution Consequence: o Low serum vit B12 o High serum homocysteine risk factor of heart disease o Haptocorrin-like protein Storage: ** unlike other water sol vit, can be stored in body for long time (even years) o Stored form: Adenosyl cobalamin o Site Liver Kidney Heart Spleen Brain Malabsorption o Destruction of gastric parietal cell IF pernicious anemia o Inability to release food-bound cobalamin to bind to IF food-cobalamin malabsorption Normally in older ppl o Acidic intestine pH unable release B12 from R-protein Function 2 enzymatic reaction in 2 dif form o methylcobalamin methionine synthesis o adenosylcobalamin convert L-methylmalonyl- CoA to succinyl-CoA in mitochondira 1. Imp for myelination of nerve a. Nerve exon is covered by myelin sheath speed up impulse transportation 2. Recycling of folate coenzyme a. Reconvert folate into active form 3. Synthesis of methionine from homocysteine a. One of the way to measure B12 lvl measure lvl of homocysteine i. If B12 less high homocysteine 1. Accumulate homocysteine due to no B12 convert homo back to methionine 4. Coenzyme of various enzyme a. Deficiency Has body storage takes months to develop Megaloblastic anemia 巨幼红细胞性贫血 o o o Pernicious anemia 恶性贫血 o o o Larger size of RBC , lesser amt Affect DNA synthesis affect RBC synthesis (RBC rapid turnover) Cause: Lack of dietary B12 intake or folate Hence it is reversible / irreversible depending on the cause A type of megaloblastic anemia which body X absorb vitamin B12 due to lack of IF In stomach secretion Caused by: Lack of IF Vit B12 is not absorbed Can be reversible with intravenous B12 Treatment Intramuscular injection of vit B12 or high oral dose induce passive diffusion Peripheral neuropathy o Due to insufficient SAM for methylation reaction of myelin o o o Nerve damage with numbness Numbness will spread as the cond getting more serious Cant hold things Cant walk/ stand need wheel chair as X walk anymore Tingling in the hands & legs Irreversible disorder Once nerve cell damage, it X be undone anymore o Vulnerable population: o Strict vegetarian Since B12 only found naturally in animal product Should include B12- fortified food or B12 supplement In the free form But still need the other 3 proteins for absorption ** if its pregnant more careful! o Lack of IF Pernicious anemia Normally due to autoimmune disease attaching GIT cells affect IF secretion Even high dose of B12 supplement X solve o Inadequate stomach acid Due to insufficient released of bicarbonate to SI (achlorhydria) X release B12 frm food 10-30% of adult over the age of 50 have difficulty absorbing vit B12 Recommend to eat B12 supplement that is aldy in free form, no need acid to free them o Intestinal surgeries / digestive disorder that cause malabsorption Eg: bariatric surgery Some may affect stomach where IF made or Ileum where B12 is absorbed o Impaired intestinal fucntion Esp ileum eG: celiac disease crohn’s disease decrease absorptive surface o competition ppl with parasitic infection tapework parasite uses vitamin causes: prolonged use of H2 blockers & proton pump inhibitors o use to tread GERD o due to bacterial overgrowth due to alkaline intestinal environment due to medication diminish acid production Measurement Blood B12 o Not the best way to determine deficiency Not as confirmative test o Affect by diet greatly o Normal B12 level in blood nay not means normal cell lvl/ activity May not be taken up by cells due to some defect Better marker: o Blood level of methylmalonic acid A protein breakdown product o Blood level of homocysteine o Their value may increase with B12 deficiency Toxicity No specific toxic effect o Large dose may casue GI symptom like diarrhea No adverse effects have been associated with excess B12 intake from food & supplement in healthy individual Vitamin C ascorbic acid o exist in 2 isomer L & D But only L- ascorbic acid is biologically active in human Naturally in some food Unlike most animal, human X syn vit C due to lack of enzyme = L-gulonolactone oxidase o From glucose/ galactose Source: Destroyed: o Heat o Light o Oxidation Alkaline solution but stable in acidic solution Cooking and storage may reduce vit C o Fe & Cu Ingest large amt of Fe & CU with Vit C may oxidative destruct vit C in GI tract Supplement: o Free ascorbic aicd o Calcium ascorbate o Sodiul ascorbate o Ascorbyl palmitate o Requirement: Widely vary di dif countries due to dif definition o Eg: Based on the conc of Vit c in WBC Based on Vit C lvl in the body that X show any symptom due to Vit C deficiency Smoking increase vit C requirement o Increase vit C turnover o Estimated value: 80mg/d Pregnant & lactating women o +20, +20mg respectively o Why? When we prepping infant formula, tend to use high temp destroy the vit C Hence one of the good sources of vit C for infant is breastmilk Cow milk also very low in vit C so not so recommended lo For development of infant To produce collagen needed in muscle tendon… Stressed / traumatized persons o Increase vit C requirement Serve as antioxidant to neutralized harmful ROS Nomenclature & Structure: Ascorbic vs dehydroascorbic o Natural form found in diet L- ascorbic acid 2,3-didehydro-lthreo- hexano-1,4-lactone. Dehydroascorbic acid oxidized form o But the distribution is dif Ascorbic 80% (more prevalent) Dehydroascorbic 20% o Interchangeable: Ascorbic lose 2 hydrogens dehydroascorbic ** they are readily donate/ receive hydrogen Dehydroascorbic acid can be reduced to ascorbic acid with Hydrogens provided by GSH (reduced form of glutathione) Both are biological active Imp structure for vitamin activity 2,3- enediol (green) 2 -OH adjacent to a double bond Dehydroascorbic don’t have hence ascorbic higer activity than dehydroas 6 carbon lactone Exist in d- & L- form o Only L has biological activity o o o Stable in dry form but once dissolved in water, it is easily oxidized pH: o Stable in solution in acidic environment (pH below 4) Hence fruits contain vit C is normally acidic o In high pH degraded easily Esp heated, exposed to air, in contact with Fe, Cu salts Metabolism: Does not require digestion Ascorbic acid o (but not dehydroascorbic acid) can be absorbed throughout SI o Via Active transport system = SVCT Sodium vitamin C cotransporter Found in intestine one is mainly type 1 Other than transporting AA into cell, also transport 2 Na into the cell o Hence SVCT can only function in the presence of Na in extracellular space o No sodium, no influx of Vit C Indirectly active transport o To ensure Na conc is high in extracellular space for use use sodiumpotassium pump that use 1ATP to transport 3Na out , 2K in o Hence we can find many Na/K pump in ileum for the absorption of vit C o But SVCT itself X use ATP, but its Na/K needs o o Enterocyte vit C conc higher than capillary Passive diffusion out enterocyte to blood Dehydroascorbic o Absorbed by GLUT o Once absorbed, rapidly reduced back to ascorbic with the help of GSH Absorption rate: o 70-90% o Decrease with increase intake of vit C `** if the conc of vit C too high in supplement slow down absorption excrete in urine SVCT X take up vit C continuously got a limit Transport in circulation o Free form o No need carrier Storage: o Not store in the body o But higher in some organ than in plasma (5-100times) They need vit C for their function o Brain o Vit C serve as cofactor for enzyme to convert dopamine noepinephrine Why? Due to more SVCT 1/ 2 Due to ascorbic acid recycling o Asc can be dehydrolyzed/ oxidation into DHA (dehydroascorbic acid) DHA can be transported into cell with GLUT1/ 3 (glucose-transporter) passive diffusion due to conc gradient! Their main function is to transport glucose into cell as passive diffusion o Hence almost all the cell got GLUT for energy o GLUT 1 all tissue Higher in RBC, blood-brain barrier o GLUT 3 mainly CNS, brain In the cell: DHA reduced back to Asc by adding 2 hydrogen atoms DHA conc decrease, Asc conc increase o Due to conc gradient, DHA outside cell passively diffused into the cell again o This is how the cell regulate the Asc recycling Metabolites: excrete in urine Ascorbate-2-sulfate Oxalic acid Ascorbate Dehydroascorbate 2,3-diektogulonic acids Function: Basis of their biological function o Oxidation & reduction of ascorbic acid o Further oxidation (irreversible) diketogulonic aicd = biologically inactive No 6-carbon lactone No enediol o Powerful reducing agent (antioxidant) Help protect other antioxidant o Reconvert vit E o Synthesis of collagen o Imp to stop bleeding Need collagen to close up the wound Hence vit C deficiency scurvy as part of prolyl hydroxylases & lysyl hydroxylases Vit C function as a reductant to reduce the Fe from ferric to ferrous in these enzymes o Vit C role in hydroxylation reaction related to Fe cofactor The hydroxylation of dopamine to neurotransmitter noradrenaline Production of carnitine o TRANSPORT fat into mitochondria for beta-oxidation ATP production o Vit C also act as reductant of Fe from Fe3+ ferrous of an hydroxylase Enhancement of Fe absorption o Take fruit juice tgt with meals o Non-heme iron Metabolism of drugs o Imp coenzyme in cytochrome P450 oxidase Activation of peptide hormones This function is due to its coenzyme role in certain enzyme responsible in the function above o Except antioxidant la it’s the function of vit C itself o Cold vs vit c Vit c enhance IS by o Promoting chemotaxis o Proliferation of some immune cells like macrophages & lymphocytes o Increase activity of NK cell o Destroy histamine Ingest high doses of vit C X prevent common cold or reduce symptom Regular vit C use appear to modestly reduce duration of symptom by 3-13% in adult Deficiency Poor wound healing o scurvy = Bleeding gums, skin hemorrhage Affect energy production o Carnitine affect Fe-deficiency anemia o Due to decreased absorption of non-heme iron o Esp vegetarian la o Petechiae= red skin discoloration due to ruptured small blood vessels Vulnerable population for Vit C inadequacy: o Vit C inadequacy: Can also occur with Intake that fall below RDA but are abv the amt required to prevent overt deficiency (ard 10mg/day) o Smokers/ second hand smoker Lower plasma & WBC vit C levels than nonsmoker o Infants Infant formula treated with high temp Cow milk less vit C Hence feed them with breastmilk Lactating mother need increase vit C to transfer to milk Measurement Plasma o <11mol/L ->17mmol/L WBC o Adequate > 2.8pmol/106 cells o Better reflect body stores Toxicity Vit C X prevent infection o But it will make your body stronger and faster recovery Obtaining the RDA or slightly higher may be protective against certain disease states Toxicity very rare o Bcs the absorption of vit C is dose dependent High lvl (10g/day) kidney oxalate stone o One of the metabolite of vit C is oxalate May be eliminated in urine But high lvl of oxalate react with calcium to form calcium oxalate stone Mild cases o Just crystal Severe o Many crystal form stone Whitening effect of vit C? May inhibit the oxidation of melanin But intravenous is better than dietary vit c la o Cant absorb that much of vit C T5- mineral Macro mineral vs trace mineral Criteria for essentiality of minerals & trace elements: 1. 2. 3. 4. 5. Present in healthy tissues Concentration must be relatively constant Deficiency induces specific biochemical changes Supplementation corrects the abnormalities Deficiency changes are accompanied by equivalent abnormalities Macrominerals: (greater than 100mg per day) 1. 2. 3. 4. 5. 6. Calcium Phosphorus Magnesium Sodium Potassium Chlorine Trace Minerals: (1mg-100 mg per day) 1. 2. 3. 4. 5. Iron Zinc Copper Selenium Iodine Ultramineral (less than 1 mg per day) Calcium 5th most abundant element int eh body o 1.4g/kg 99% deposited as HA (hydroxyapatite) Ca5(PO4)3OH in bone & teeth For rigidity 1% Intra & extra-cellular fluid o Ionic form Ca2+ o Bone: 150mg Ca/g bone o Soft tissue: Liver, muscle, brain Less than 35 ug Ca/g tissue Ca plasma level Controlled by 3 hormones: o Parathyroid hormone PTH o 1,25 dihydroxycholecalciferol (calcitriol) o Calcitonin Other factor affecting Ca mobilization & deposition o Age o Diet o Hormonal status o Physiological state Bone Ca homeostasis o If mobilization exceed deposition bone weak osteoporosis break easily o Relate to bone strength Ca mobilization mostly happens in bones & plasma, seldomly in teeth! Food source: Poor source: o Spinach, rhubarb, oxalic acid Better absorption in animal source than plant o Ca in milk and dairy food more readily absorbed than in plants Due to anti-nutrients Phytate o In cereals Oxalates and tannins o Leafy green vegetables Ca is absorbed better in the free form o These anti-nutrients may bind to the Ca reduce the bioavailability Ca in milk may also bind to other protein = lactalbumin But this X affect the absorption But if consume with plant food with those anti-nutrients affect Ca absorption Cereal + milk Enhancer of Ca absorption o Vitamin C Vit C reduce Ca to the reduced form that is more bioavailable o Phosphorus Normally food with high Ca is high in P no need purposely find food high in P to pair with Ca Supplement: o Calcium citrate Good for those with limiting gastric acid production (older ppl) Can be ingested without food o Calcium carbonate o Take note: Generally absorbed better with food Absorption higher consumed in less than 500mg o Requirement More focus on elderly ppl on Ca requirement o They need more Ca o reasons: Elderly tend to have lower physical activity Low Ca retention in the body o PA influences Ca turnover through increase Ca retention Elderly has lower expression of TRPV6 & calbindin Post-menopause women lower estrogen Reduce Ca absorption from the diet o Oestrogen can increase calcium absorption directly and indirectly by stimulating 1-α hydroxylaseactivity in the kidney. Hence elderly more risk to osteoporosis as bone is the main site for Ca in homeostasis o Other Lactation: Need more Ca mammary gland needs high Ca to produce breast milk nutrients for baby Growth Need more Ca for bone development Metabolism: Ca naturally in food & supplement insoluble salt o Can be solubilized free Ca2+ from Ca salt o But solubilization X ensure better absorption Free Ca may bind to other dietary constituent, limiting bioavailability But Ca bind with milk lactose improves Ca solubility absorption increase This effect more pronounce in infant > adult Not all consumed Ca is absorbed o Unlike Na, potassium, chloride o Reason: Presence of anti-nutrients Food source Mixture of food consumed Physiological status of individual Absorption main site: o Small intestine duodenum to ileum o Only small amt 10% in colon 2 mechanisms for Ca absorption: a. Paracellular transport (diffusion) i. Through the tight junction between mucosal cells ii. Passive Diffusion no need energy 1. From high conc to low conc iii. b. Transcellular transport i. Active transport need atp ii. = vit D-dependent transport 1. Calcitriol iii. When Ca intake low – moderate iv. Steps: 1. Ca diffuse across the brush border down its thermodynamic gradient into the cell as free unbound Ca++ a. Required the transport protein= TRPV6 (transient Receptor Potential Vanilloid subfamily member 6) no need atp at this point i. Vit D-dependent 2. Bind to intracellular protein= calbindin (also known as D9k) a. Transport Ca across cytosol b. Vit D-dependent c. Carry Ca to the other protein released Ca into plasma 3. Vitamin-D-dependent Ca-ATPases pump a. Release Ca into plasmaa b. This need atp c. This is a co-transport i. Ca release + Mg take into the cell 1. 2+ in, 2+ out 2. To maintain the ion balance 3. Ca form in transport in blood o Most 50% of the blood Ca is free form= ionized Ca2+ 100mg/L (2.5mmol/L) May have small decline in older age (10%) due to age-related decline in total calcium-binidng capacity of serum protein o The other 45% Protein-bound calcium Prealbumin, albumin o Small 5% Ca complexed Ca Bind to phosphorus, sulfate, citrate o It’s imp if we wanna measure plasma Ca as the value is reflecting the free Ca, not including those bound to protein/ complex Homeostasis of Ca: o Extracellular Ca conc regulation Regulated by Active vitamin D / calcitriol o renal tubule increase reabsorption o intestine increase absorption o mechanism increase expression of TPRV6 & calbindin Calcitonin o Totally opposite effect of PTH & calcitriol o Also syn by thyroid gland (parafollicular cells) o Help prevent Ca toxicity + make sure bone have enough Ca Inhibit osteoclast-mediated bone resorption Inhibit activation of Vit D Inhibit renal Ca conservation Parathyroid hormone o Low level of Ca in blood will stimulate the release of PTH on the thyroid gland o Pth ACTS ON Kidney Increase calcitriol synthesis act on renal tubule Increase Ca reabsorption reduce Ca loss Bone Stimulate the release of Ca frm bone to blood Inhibit collagen synthesis by osteoblast stimulate their proliferation & differentiatin into osteoclast (bone-breaking cell) Osteoclast release protease & acid resorb/degrade bone release Ca to blood Nutrients interaction inhibition of absorption Divalent Cation (Zn, Mg) Compete for intestinal absorption esp an excess of one in GI tract Unabsorbed dietary fatty acids Form insoluble Ca soup Cannot be absorbed excrete in feces Drugs Proton pump inhibitor o Used to treat GERD o insufficient product of Gastric acid Function 1. Bone mineralization o 99% of total body Ca is found in bones & teeth o Ca is part of mineral comlplex deposited on an organic matrix comprised primarily of type I collagen o Hardness is enhanced by presence of fluoride 2. Cell signaling o Though less than 1% of total body Ca serves in cell signaling system but the flux of Ca from one compartment to another is vital in metabolic regulation For communication between cells + between organelles inside the cells o The flux is facilitated by intracellular Ca-binding protein = calmodulin 3. Cell death o In normal state cell only allow fixed amt of Ca come into the cell o If the cell is injured Ca balance is disrupted active energy-driven export of Ca will be interrupt Ca continue flow into the mitochondria –> raise ionic conc of mitochondrial matrix mitochondrial dysfunction o Ca influx into the cytosol + nucleus cell die o Very imp if it happens in heart cell Heart muscle cell die heart failure! 4. Muscle contraction o In muscle cell, special endoplasmic reticulum= sarcoplasmic reticulum= calcium storage site imp for muscle contraction o Deficiency In early adulthood o stunted growth o Failure to achieve peak bone mass A risk factor for osteoporosis in later life Children o Poor Ca absorption due to vit D deficiency rickets Causes o Kidney failure o Reproduction system disorder Hormonal imbalance affect Ca absorption and retention Toxicity Accumulation in blood & tissues due to dietary excess is unknown o Bcs Ca level is controlled tightly by homeostatic control of hormone Excessive Antacid tablets & Ca supplement o Excessive intake of Ca & alkali MAS milk alkali syndrome MAS is reported at Ca carbonate intake >= 4g/d or more o Reversible once stop these tablets o Symptoms: Nausea, vomiting, dry mouth, confusion, lethargy May cause kidney damage o Calcium may bind to oxalate Form crystal Measurement Normal plasma range for Ca= 2.15-2.55mmol/L Usually X affected by dietary insufficiency o Bcs plasma Ca level is tightly controlled o Hence not good to reflect the Ca status in bone Bone mineral concentration can be measured by o Neutron activation analysis o DEXA dual X-ray absorptiometry Phosphorus: 80-85% is found with Ca in hydroxyapatite (HA) in the bone Other form in body o Phosphate PO4o Rarely free phosphorus o present in every cells Ca & P are essential minerals that usually considered tgt bcs the formation of bone & uptake of Ca for this purpose is closely tied to an optimal ratio of Ca:P of 1:2 – 2:1 Food source: Food source high in P is also high in Ca Present in o all natural food o In many addictive o Soft drink phosphoric acid Absorption is atd 60% of intake o Reduced by non-starch polysaccharides Metabolism Form: o Organic bounded phosphorus Nned to be digested release inorganic Phosphate By phospholipase Can be upregulated by calcitriol But X free all bound form o Eg: X phytic acid-bound P 2 absorption mechanism: o Readily absorbed in the free form 1. Paracellular absorption 2. Transcellular transport Active saturable sodium-dependent mechanism Sodium-phosphate Co-transporter o 2NA + 1phosphate transport into the cell tgt at the same time o Need ATP o Aluminum, magnesium (as hydroxides), and calcium (as carbonate or acetate) are common components of antacids and for years were given in pharmacological doses to bind dietary phosphate in people with hyperphosphatemia (high blood phosphorus concentrations) caused by kidney disease. Reabsorption o At kidney 85% proximal convoluted tubule 10% loop of Henle 3% distal convoluted tubule 2% collecting duct Renal phosphate conservation main mechanism for P homeostasis Enhance o • Vitamin D/ calcitriol Stimulate phosphate intestinal absorption o • Glucocorticoids o • Growth hormone Inhibit o • Oestrogen o • Thyroid hormones o • Parathyroid hormones Stimulate excretion of P In urine > (override) Stimulate resorption of P from bone Net effect: reduce plasma P o • Elevated plasma Ca levels Function: Skeletal rigidity tgt with Ca hydroxyapatite Energy metaboslim o Form ATP phosphate bonds in ADP Constituent of phospholipid and membrane Constituent of nucleic acid Deficiency: Hardly happen as dietary deficiency as it found in every type of food unless have some disease Fanconi Syndrome o Kidney disorder Wont be able to control the release of these substances (phosphate) into urine Hence urine may have high ……… Lead to phosphate deficiency o To correct this phosphate deficiency phosphate supplement to prevent skeletal bone disorder (need both Ca and P for bone health HA) Consequence: o Bone pain & poor skeletal growth & mineralization o Lack of HA for deposition in the bone matrix Other factor o Phytate form insoluble salt with Ca, Mg, Fe rendering these minerals unavailable for absorption Toxicity: Generally high intake are balanced by high excretion in urine o But may be disrupted in renal patients Excess P can cause o Diarrhea o Hardening of organs & soft tissue Measurement: Serum total phosphate levels are measured. The normal adult range is 0.7–1.5 mmol/l. Magnesium: Both vegetables and meats are good sources of Mg o milk and milk products are relatively poor sources of this mineral. Mg stabilizes mammalian membranes and in plants. o ionically bound in the centre of the chlorophyll molecule. Mg is a cofactor in almost all phosphorylation reactions involving ATP. universality of its presence in the food supply low deficiency states if consuming a variety of foods. Food source: Spices, nuts and cereals are rich sources of Mg. Green leafy vegetables such as spinach are also rich in Mg. Beverages rich in Mg are coffee, tea and cocoa. Requirement: Ca is for contraction Mg for relaxation o Work antagonistic o Due to muscle relaxation imp during pregnancy Prevent the uterus to contract too early o Lactation lady: Need more Mg good source of nutrients for body for growth and teeth? Metabolism: Absorption: o Same as Ca & P Mediated by both passive diffusion & active transport Paracellular & transcellular o But Mg for paracellular transport need protein = claudins o Transcellular need protein = TRPM 6 & 7 o Absorption rate vary from 30-70% o o o Fatty acid Form soap with Mg Phosphorus Form a complex Mg3 (PO4)2 X absorbed Both inhibit each other Calcium Mg is needed for Ca absorption Transport in plasma o 55% - free ionic form Mg2+ o 33%- protein bound o 13% complexed with citrate, phosphate, sulfate Homeostasis o Renal excretion Hormone affect Mg metabolism o PTH Increase intestinal Mg absorption Reduce renal excretion Enhance bone Mg resorption Function: Bone integrity Bone mineralization o Tgt with other mineral + phosphate HPX o Bone has 50-60% of Mg Exchangeable Mg pool to maintain serum Mg Energy metabolism Cofactor for enzyme requiring ATP Mg bind to ATP provide stability o Replication of DNA o Synthesis of protein & RNA Phosphate transferring system Muscle relaxation Magnesium also may mimic or displace calcium from calcium-binding sites, decrease the flux of calcium across the cell membrane, further inhibit the release of calcium from the sarcoplasmic reticulum in response to increased influx from extracellular sites, and activate the Ca2+-ATPase pump to decrease intracellular Ca2+ concentrations. Magnesium may compete with calcium for nonspecific binding sites on troponin C and myosin to alter muscle contraction. Additionally, in smooth muscle, magnesium, if bound to sites that are normally occupied by calcium, can inhibit contraction. Membrane stability Ca & Mg bind to phospholipid maintain membrane stability nerve cell function Deficiency: Due to: o High renal loss o Malabsorption Use of drug Diuretics manage hypertension Symptom o Cardiac arrhythmias & cardiac arrest Due to Mg has ability to relax o Calcitriol not so active in promoting intestinal Ca uptake w/o Mg Mg is needed to be exchanged for the Ca to pump out of enterocyte Measurement Serum Mg Normal : 0.7-1.0 mmol/L Toxicity Occur in renal or adrenal disease T5ii- Trace Minerals List: o Fe o Zn o Cu o Se o Iodine Needed in smaller amt , in ug (macro need in milligram) can further classified into ultra-trace mineral o excluding Fe, Zn, Cu o still got a lot la, not only Se, iodine Iron essential mineral o o need to make hemoglobin, RBC carry oxygen needed in myoglobin in muscles store oxygen in muscle Fe in muscle is dif structure with hemoglobin Form: (2 ionic stage) o Ferric 3+ Has to be reduced to be absorbed & function By stomach low pH of gastric juice Needed when combine with protein / for storage o Ferrous 2+ The only active form that can bind to O2 Food source: Only can absorbed Fe in free form o X bind to protein 2 types: o Heme Animal myoglobin give meat red color In ferrous state binding with O2 Heat/ exposed to O2 ferrous is oxidized to Ferric red to brownish not fresh liao o Hence manufacture may treat meat with nitrite / CO bind to the Fe, to retain it’s ionic state to retain the meat reddish color o Non-heme Plant X in free form Inorganic Fe bound to various protein Major dietary Fe Though we take a lot Fe from plant, the % of absorbed Fe is very low compared with heme Fe than we can absorbed Hence for vegetarian, in order to make sure has enough Fe, or increase the absorption take with fruit juice for vit C enhancer of absorption o Non heme more factors affecting the absorption o The absorption of non-heme Fe in the presence of meat, fish, seafood To investigate whether is protein in the meat that enhance or the type of meat. Result: o Egg absorption enhancer efficiency is << than protein in meat protein Hence, not all protein can enhance the absorption o In the animal meat, there is a factor that encourage the absorption of Fe, but not identify yet Requirement: In 3rd world country high risk of Fe deficiency due to poor diet o less meat intake o rich in whole grain, cereal, legume but only nonheme Fe o less fruit intake for vit C menstruating women & growing children high risk pregnant need more Fe for fetus growth o make more rbc o tissue growth metabolism: absorption: o mainly in duodenum o free state of Fe is toxic hence need close controlled on transport & storage by many protein transferrin o transport Fe in plasma transport to the sites needed Fe like BM o temporary holding Fe in intestine mucosal cell not the real storage of Fe just a standby if not needed, excreted into the feces there is also ferritin in enterocyte main storage of ferritin wont discard Fe stored in ferritin to the feces will be stored till they are utilized Ferritin / hemosiderin o Long term Storage in a lot of cell body X store free Fe unused Fe o site: liver, spleen, bone marrow o Transport mechanism: Dif mechanism for dif Fe hence not competitive! 1. Heme Fe Must be hydrolyzed from the globin portion of hemoglobin & myoglobin b4 absorption o Done by proteases in stomach & SI Protein: HCP-1 o Carry heme Fe into enterocyte o Found mainly in proximal SI In enterocyte: o Heme (heme-oxygenase) release ferrous from the heme 1. Non-heme Fe Typically bound to componenet of food o Must be hydrolyzed in the GIT b4 absorbed 1. HCL, proteases released nonheme Fe, mostly as Fe3+ from the food component 2. The acidic environment reduce to Fe2+ (more soluble to be absorbed ) ** but not all o If the Fe3+ is not reduced, passed to SI which is more alkaline 1. May complex to produce Fe(OH)3 precipitate less absorbed o o 2. Reduction to Fe2+ by cytochrome B reductase 1 (on the enterocyte brush border) Dcytb is vitamin C dependent o It also has the ability to reduce Cu2+ Cu+ Protein: DMT-1 o Take up the non heme Fe in ferrous form Not in non heme Fe a!!!! Can also absorbed other divalent Zn, Mn, Cu, nickel, lead Why less absorption than heme? o Bcs there is no protein that is specifically take up non-heme frm the gut o But non-heme iron has to be hydrolyze from the binding protein in the diet and be reduced to ferrous in order to be absorbed This process involved duodenum cytochrome B This needs vit C Enterocyte use: Free Fe is toxic mostly bounded Fe within the cell Can be either Stored in ferritin temporary o In ferric form + apoferritin ferritin o Increase synthesis in high Fe intake Transport to blood by ferroprotein o oXidation to Fe3+ first by 1. hephaestine (Cu-containig protein) 2. ceruplasmin (Cu-containg preotein) ** Cu deficiency reduce their conc Fe accumulation in intestine & liver o Transport by transferrin in ferric state 1. When Fe bind to other protein ferric state To liver , BM, muscle, other cells Have transferrin receptor bind and release Fe into Liver In the form of Hemosiderin o Lesser storage capacity Ferritin o Major storage Regulation o Liver produce hepcidin when Fe high Function Hemoglobin o Transport of O2 o Cell respiration Myoglobin o O2 storage in muscle Component of enzyme o Cytochrome Essential for E- transport system in mitochondria Transfer of electron due to the change in oxidation state of Fe o Received e- reduced to ferrous o Donate e- oxidized ot ferric Cytochrome P45? in liver imp for drug metabolism Chrome= color due to heme Deficiency: 3 stages: 1. Depletion of Fe storage a. Measured by serum ferritin i. Ferritin is the main Fe storage 1. Though hemosiderin also store la, but not the main ii. Fe stores are depleted and serum ferritin levels will fall below 12 μg/l. Other measures of Fe status will be normal. 2. Fe deficient erythropoiesis a. Measured by i. Decreased in transferrin saturation level ii. Increase erythrocyte protoporphyrin 1. The one that bind with heme to form hemoglobin 2. If heme X form due to lacking of Fe many protoporhyrin b. Fe stores are depleted and supply does not meet needs for haemoglobin production. Serum ferritin levels will be low, serum Fe concentration is low, and transferrin saturation is 3. Actual iron-deficiency anemia a. Measure by: i. Depressed hemoglobin 1. Haemoglobin levels <11.5mg/l in women and <13mg/l in men. 2. Red cells are microcytic and hypochromic 3. Mean corpuscular volume MCV < 77fl & mean cell hemoglobin (MCH) < 27pg. b. Clinical symptom: i. Pallor ii. Weakness iii. Changes in nail 1. Spoon shape when Fe def is very severe Vulnerable population o infants and young children (6 months to about 4 years) because of the low iron content of milk and other preferred foods, rapid growth rate, and insufficient body reserves of iron to meet needs beyond about 6 months o adolescents in their early growth spurt because of rapid growth and the needs of expanding red blood cell mass o females during childbearing years because of menstrual iron losses o pregnant women because of their expanding blood volume, the demands of the fetus and placenta, and blood losses that are incurred in childbirth Toxicity: Cause: o Due to overdose of supplement o Genetic disease: hemochromatosis High lvl of Fe being absorbed Fe deposit in liver & heart cirrhosis, congestive heart failure death Why has higher risk of cancer? ROS generation: Fe is toxic high lvl of Fe generate ROS damage cell mutation if mutated cell not removed proliferate and form tumordevelop hepatocellular carcinoma & colon cancer Cancer cell also need Fe to survive o Symptom: o Bloody diarrhea Affect other micronutrients absorption Sodium: Major extracellular electrolyte o Circulate as fully dissociated ion due to its +1 charge fully water sol Body content o Male: 52-60 mFq/kg o Female: 48-55 mEq/kg Only small amt of Na is involved in Na turnover in body o (2/3 – 3/4) Mostly are fixed in the bone mineral apatite Can be released when hyponatremia Food source: Food addictive o MSG o NaCl Weight ratio: 40% Na, 60% Cl 3g of NaCl 1.2g Na, 2.8g Cl (accd to molecular weight ratio) 1 tsp salt 2300mg sodium Nearly all food has Na impossible to have sodium deficiency o Except pure refined food like pure fat Requirement To avoid taking too much not to avoid deficiency RNI based on normal individual has a moderately active lifestyle & lives in temperate environment o Dif PA & environment & medical condition affect Na requirement High PA/ hot temp increase Na due to increase sweat loss Na through skin Air-con less Na Level of serum Na is regulated well in small range not highly variable o Hypernatremia > 150 mEq/L o Hyponatremia < 135 mEq/L Causes of hyper/ hyponatremia o o Hyponatremia mostly due to disease/ other complication, rarely due to dietary factor, except excess water intake Regulation of serum Na Bcs the range of serum Na is small, need well regulation system Include regulation of (not only just Na, but other elements as well) o Na o K o Cl o Water balance These ions (fully ionized solutes) may affect the osmotic pressure of the system Mechanism: o Hormonal Renin indirect involve in regulation of Na o But imp for activation of Angiotensin II conserved sodium Hypothalamus: Osmoreceptors in anterolateral hypothalamus sense the changes in Na conc activate osmoreceptor release several hormones o Na is the most potent ions to stimulate osmoreceptors Increase Na o ADH by posterior pituitary 1. increase renal water resorption dilute the Na conc in body 2. X enhance Na excretion, but retain water to dilute Na conc Decrease Na + high K o Aldosterone by adrenal cortex 1. Increase renal reabsorption of Na ion o Atrial natriuretic hormone 1. Inhibit ADH o o o Renin 1. Convert Angiotensin I II Angiotensin II 1. Increase Na resorption in kidney 2. Convert to Angiotensin III Stimulate aldosterone release renal resorption of Na Physical/chemical Disease due to dysfunction of Na regulation Diabetes Insipidus o Absence of ADH o Body X conserve water frequent dilute urination & extremely thirsty o Very high Na in body o Treated with oral ADH o Causes: Dysfunction of posterior pituitary (tumor…) Hypertension o High Na conc high osmotic pressure Function 1. Regulation of osmotic pressure/ blood pressure 2. Nerve conduction To let nerve function properly, there should be a potential difference between inside,, outside of the nerve transfer signal o To maintain this imbalance charge, Na-K pump is very imp! Bring in 2+ potassium in, bring out 3+ sodium 2 potassium ion in, 3 Na ion out. 1 charge dif To ensure 2 different: Electro chemical gradient o Imbalance chemical conc o Imbalance electric charge 3. Muscle contraction/relaxation Na/K pump o is responsible to bring in Ca into the cell o Bring in Ca, bring out Na out of muscle cell muscle contract Na/Ca pump o Also imp to ensure muscle has enough Ca Ca pump o But not involving Na not discussed 4. Active transport Mainly Sodium-potassium pump o Still got other pump need Na la Toxicity Hypertension & Heart disease associated Symptom: o Strong emetic o Excessive oral loads potentially fatal o Intravenous severe & rapid effect Measurement: Plasma Normal range: 135-150 mmol/L Potassium Major intracellular electrolyte o Na is extracellular o Due to the Na/K pump bring in 2 K+, bring out 3+ Na Hence little K in extracellular fluid (3.5-5 mEq/L) Healthy male range 42-48 mEq K+/kg All body K is exchangeable o Only small amt that is bound irretrievably in bone mineral X involved in the turnover Food source: Milk, milk product, orange juice, avocado, fish, banana o Myth: banana can prevent muscle cramp due to high level of K Bcs the cause of muscle cramp can be due to many reason, X just be prevented by taking high K though K do have this effect It’s just good to be pre-workout to supply simple carb as the immediate fuel K passes freely from GI enterocyte into body o Most excrete in urine o Only small amt in feces Diarrhea o Short term o No need 特地 consume more K to replenish K Long term Need to make sure replacement of K for the loss That’s why ask drink 100 plus when diarrhea Requirement: Hardly hyponatremia due to dietary factor as almost all food contain K Increase requirement to give therapeutic effect on hypertension o High K relax blood vessel lower bp o DASH diet reduce NA, increase K reduce hypertension, risk f heart attack fruits & vege K/Na ratio higher Function same as Na working tgt in Na/K pump electrophysiology of nerve & muscles Deficiency: cause medical condition o long term diarrhea loss of body electrolyte hypokalemia o impact: o most affected muscle activity (contraction) heart bradycardia (low heart beat irregularly) cardiac arrest intestine lost in motility o reduce absorption of nutrients brain mental depression & confusion toxicity: acute intake of supplements exceeding 17.6g / 450mmol symptom: o paraesthesia ard the mouth o tachycardia (fast heart beat) cardiac arrest o muscle weakness measurement: unreliable o the plasma conc is replaced by the intracellular K when it is deficient normal plasma conc = 3.5-5 mmol/L causes of hypokalemia & hyperkalemia Chlorine Involved in o Osmotic pressure o Acid-base balance Normal Cl level o in plasma: 100-106 mEq/L Range very small!!! 变化很小罢了 o Sweat Usually very little but can be As much as 40 mEq/L o intracellular fluid veru little ~ 4mEq/L o intestinal juice 69-127mEq/L HCl gastric juice o In urine Main excretion pathway o In fece Very little Bcs in the GI will be reabsorbed and recirculates into the body like Na & K Increase excrement in Secretory diarrhea o Your intestine X properly absorb / secrete electrolyte Passively distributed throughout the body o Although it is relatively reactive ion chemically o Cl- move to replace anions lost to cells via other processes Food source Table salt o Tgt with Na o If excess Na, also excess Cl Yet usual plasma Na+ : Cl- ratio = 3:2 This imbalance due to: Passive natur of Cl transfer between water compartments & to the active system that serves to retain Na+ Requirement No specific DRV Function: 1. 2. 3. 4. Cl is the anion to the cations Na & K Helps keep the amt of fluid inside & outside the cell in balance Helps maintain proper blood volume, bp, pH of body fluids Imp for the function of stomach & RBC o Stomach: Formation of HCl for gastric juice For absorption of vit B12 Kill microbes o RBC RBC X carry CO2!!!! It just facilitate the process of transportation bcs 大多数的时间,CO2 在血 液里面 in the form of HCO3- Chloride shift CO2 diffuse into RBC CO2 + H2O – (carbonic anhydrase) H2CO3 –(dissociated) H+ + HCO3 HCO3- will leave RBC making the RBC to be lack of 1 negative charge o To balance the charge, Cl- need to come in At lungs, the Cl- move out, HCO3- move in convert back to H2CO3 CO2 diffuse out into lungs Measurement: Normal plasma conc: o 97-107 mmol/L Abnormal lvl is not diet related o Due to metabolic reasons related to Na+ & K+ homeostasis I. Deficiency hardly can happen due to abundant in food II. Tight regulation of body Normally if we wanna measure the electrolyte status, we wont just measure one of the electrolytes, but a lot tgt Cl, K, Na, HCO3- Causes of hypochloremia o o o o o o Increased extracellular water volume due to trauma and/or cachexia Vomiting with large loss of gastric HCL Overuse of diuretics Overuse of adrenal steroids with retention of Na+ Chronic respiratory acidosis (high CO2, low pH) Chronic renal disease, renal failure Cause of hyperchloremia o o o o Dehydration Diabetes insipidus Brain stem injury Ureterointestinal anastomoses due to reabsorption of Cl– Copper An adult has 80mg of Cu in body o 40% in muscle o 15% in liver o 10% in brain o 6% in blood Main function of Cu cofactor of enzyme o Incorporated in many metallo-enzyme Interact with Fe o Cu & Fe both are needed for hemoglobin synthesis Anemia can due to Cu deficiency Food source Not rare nearly found in all food Rich in o Legumes & nuts Esp cashew o Raisin o Whole grains o Beef liver o Shellfish & shrimps Poor in o Dairy products Absorption of Cu o vary in dif form: 2 types: Cuprous o Cu+ o Better absorption Cupric o Cu2+ Hence high lvl of Cu in food X mean it is a good source Need to be high in Cu + to be better source o The presence of other mineral affect absorption Zn, vit C, Fe may reduce the Cu absorption Requirement: Increase requirement for pregnancy o Need Cu for RBC formation Heart Bone Nervous system Blood vessel Average intake is higher in men than in women Relationship with Zn High intake of Zn reduces Cu absorption High Cu reduce Zn absorption Why? o Due to metallothionine (MT) Both Zn & Cu can bind to MT But For Cu: o Not helping in absorption into the cell o o o The MT affinity is higher to Cu bind strongly to form a stable MT-Cu stored/ trapped in enterocyte 1. Increase fecal excretion of Cu Higher MT higher Cu complex higher excretion o For Zn: o MT help absorb into enterocyte o High Zn increase MT expression Hence high Zn high MT more Cu excrete High Cu less free MT to bind Zn more Zn excrete (A) Normal absorption of zinc (Zn) and copper (Cu) is depicted. Metallothionein (MT) binds both zinc and copper in the enterocyte but with a higher affinity for copper. (B) In the setting of zinc supplementation, there is an overexpression of metallothionein, which preferentially binds copper for excretion into the stool. Metabolism: Absorption: o Mst Cu in food is Cu2+ & bound to organic component like AA Need to be freed from AA By HCl, pepsin, protease o Site: SI limited extent to stomach o form: Cu2+ Need to be reduced by STEAP reductase Cu+ Cu+ Take up by 2 carrier o Ctr 1 1. The expression is regulated by Cu intake high Cu, decrease CTR1 o DMT1 1. Less extent 2. Compete with other divalent o In cell: once absorbed bind to MT (blue) and copper chaperones (pink) transport out to blood via ATP7 (A/B) (yellow) This CC (COX17, ATOX1) has 2 roles o Reduce free Cu+ toxicity to the cell 1. Prevent Cu+ bind to cells for bad interaction o Transportation 1. COX17-Cu Brought to mitochondria 2. ATOX1-Cu Brought to organelle Facilitate Cu transport to blood If too much Cu CTR1 reduce ATP7 increase Factor: Enhancer Amino acid Glutathione Organic acid Inhibitor Alkaline o H2 receptor blocker o Proton pump blocker Phytic acid Zn o Zn stimulate metallothionein syn in intestinal cells o Intestinal cell Cu use o Stored Bind to metallothionein o Used functionally o Transport through cytosol to blood Via active transport ATPase ATP7A o Mutation leads to Menke’s disease Transportation in blood o Transporter: In portal blood Albumin Transcuprein In other blood Ceruloplasmin (most active Cu transporter) o It is also the transporter of Fe o Made from liver o Deliver to: Liver 1st Cu + apoceruloplasmin Ceruloplasmin (transport protein & enzyme activity) o Transport Cu to the rest of body 1. `Bind up to 6 Cu+ o Enzyme activity: 1. As a Ferroxidase Release Fe from liver storage to transferrin in plasma transport Fe to plasma o Convert ferrous ferric o Ferric + apotransferrin transferrin transport to reticulocyte for hemoglobin synthesis 2. SOD (superoxide dismutase) Antioxidant Cu & Zn depdendent enzyme Convert superoxide radical O2 & H2O2 o H2O2 also toxic to cell o Need another enzyme to neutralize it Selenium Excretion: o Main site: Feces Not absorbed in intestine feces Unused Cu from liver bile intestine feces o Urine o Skin o Hair Function Regulation of gene expression o MT metallothionein transcription o Regulated by both Cu & Zn MT can only be syn in the presence of both induce gene expression Can also expressed by mercury & cadmium non-essential to reduce toxicity Zn more influence Imp component of mitochondrial respiratory enzyme o cytochrome C oxidase imp in energy production fucntion in the terminal oxidative step in mitochrondrial elextron transport o Is also Cofactor of dif enzymes o o Interaction with other nutrients: Fe o Imp for normal Fe metabolism Ferroxidase activity of hephaestin in enterocyte (Cu-dependent protein) Ceruloplasmin Responsible for the oxidation of Fe to Fe3+ only then can be bound to transport protein transferrin for delivery to tissue Cu deficiency Fe-trapped secondary -Fe deficiency anemia Deficiency (premature infant/ genetic disorder) All enzyme activity affected Prominent clinical features: o Related to blood Anemia (Fe-resistance) Poor wound healing o Related to collagen & elastin production Affected site: Blood vessels & heart Bones & muscles to the bone o Related to antioxidant (SOD) Not so imp body has many other can compensate Rare cases due to food intake o Maybe due to too high Zn intake Other factor: o Can happen during pregnancy premature fetus Consequence: Premature infant Why? Mother Cu not enough to give to fetus During late stage of pregnancy Cu can be accumulated in fetus liver large store for usage when he’s born Symptom: Failure to thirve Fe resistant anemia Twisted kinky hair Skeletal changes (failure for syn of connective tissue due to collagen & elastin affected) o Fractures o Osteoporosis o Weakness o Joint pian o Abnormal blood vessels o 2 Genetic disorders: abnormal Cu lvl in body Menkes syndrome (ATP7A) Cu decrease Faulty Cu absorption o Enterocyte absorb Cu but X release into circulation o Less severe o Treatable: 1. Intravenous Cu Faulty transport to brain o Premature death due to Cu deficiency in brain o More serious hardly treatable Wilson’s disease (ATP7B) Cu accumulation Impaired incorporation of Cu into ceruloplasmin o But this protein is responsible for Cu to be transport out of liver o Also accumulate in other part of body : eye, brain o Toxic lead to death Decreased biliary excretion of Cu Feature: o Kayser-Fleischer ring in the eyeblack Treatment: o Limit absorption of Cu with Cu-binder 1. Bind to Cu in body to reduce free Cu toxicity Toxicity: Too much Cu can induce body mechanism to reduce absorption but still got chance to toxic Cause: o Deliberate ingestion of Cu salt o Drinking contaminated water Symptom: o Actue toxicity nausea, vomit, diarrhea fatal o Chronic Cu poisoning liver cirrhosis Due to contaminated by Cu water pipe Cooking utensils More vulnerable to Infant Young children Selenium Similar chemistry to sulfur Trace amt needed for cellular function very toxic in even small doses o but have a better excretory pathways than Fe & Cu urine Can be seen as an ingredient in o Multivitamins o Dietary supplements o Infant formula A component of antioxidant enzyme (GPx) o Neutralize H2O2 produced by SOD (Cu antioxidant ) Food source the selenium content of plant foods and products is extremely variable. o Depend on the soil Se conc Whole grain Seafood Organ meat o Tissue esp skeletal muscle can store more Se meat source Risk of deficiency; o Vegan Form: o Organic Selenomethionine Selenocysteine o Inorganic Selenide Selenite Slelenate Requirement Increase for o pregnancy: Se def miscarriage & CNS defect of fetus o Lactation Breast milk is a source of Se for baby o Male > female: Se def infertility sperm quality sperm number o Metabolism Absorption very efficient blood o Most ingested is absorbed o Site: SI o Most of Se in body found in blood 2 fades: o Used in selenoprotein enzyme o Stored in kidney/ liver as SeMet o Excreted from body Urine (primary route) Feces (predominant if due to low intestinal absorption) Sweat Different form of Se: (similar absorption rate) o Organic selenium Se compete with sulfur in some AA to form Sec, SeMet 2 types: Selenomethionine o Mainly found in plant protein Selenocysteine o Mainly in animal protein Enter enterocyte via amino acid transport system B0AT1 o Na+ dependent neutral amino acid transporter rBAT o neutral & basic amino acid transport protein o Inorganic Se: (selenium salt) Types: Selenate Selenite o Less absorption rates Absorbed by active sodium-dependent transport solute carrier 26 (SLC26) Hence, no need to convert inorganic organic o That’s why Se absorption very efficient Transport in blood o Selenoamino acid travel free to liver and other tissue o Selenite Reduced by glutathione & glutathione reductase selenide Transport form Binds to VLDL or LDL Bind to albumin To liver o Major organ metabolizes Se o 2 forms reached liver: Se-albumin SeMet bound to albumin o o o 2 fades: 1. Incorporated in some protein such as albumin 2. Convert to Sec via transsulfuration pathway Intact form: Sec Selenate & Selenite HSe Converted Sec + dietary Sec—(SCLY selenocysteine bete-lyase) HSe Selenite – (TRXR / glutathione-glutaredoxin pathway) HSeSe-Phosphate (final form) HSe- --(SPS2) Se-P Useful to form Sec tRNA for selenoprotein production Transport Se through blood to other tissue by LDL / VLDL Factor affecting Se absorption: o Methionine & Cysteine similar structure to Sec & SeMet o ADE vitamin increase Se absorption Found in: o RBC o Liver o Spleen o Muscle o o o Nails Hair Tooth enamel Function 1. Se is essential element for Selenoprotein o o Syn of selenoprotein: Sulfur-containing AA + Se Secysteine Selenophosphate help donate the Selenium to form Secysteine Catalyzed by selenophosphate synthetase o Cofactor= Vit B6 Se bond with Sulfur in the cysteine /methionine using their SH grp from there incorporated into selenoprotein glutathione peroxidase (GPx) Most well known selenoprotein Catalyze the reduction of … 2 peroxides water & oxidized glutathione (GSSG) o H2O2 o Organic peroxides (fatty acid peroxides) With glutathione (GSH) presence o Furnish the reducing equivalents in the reaction o GSH 把 H2O2 的 oxygen 拿走 ** this reduction can be performed by other antioxidant as well: o Such as: 1. Catalase 2. Peroxidase o If we lack of one, wont have too severe consequence for short term o If long term antioxidant system too saturated not enough antioxidant to neutralize ROS damage body cells Essential enzyme to maintain the redox state of membrane & cell content Esp RBC o No mitochondria (a imp organelle to maintain optimal redox state) o Imp to regulate redox state for gas exchange by hemoglobin o During exchange, peroxide may formed need GPx to suppress its formation o The activity of GPx sensitive indicator of Se status Less active in deficiency ppl 4 isozymes GPx1 & GPx4 most common in most tissue o GPx1 1. Rbc 2. Kidney 3. Liver o GPX4 1. Testes protec thte testes function GPX2 o GI tract GPX3 o Kidney o Lung o Heart o Breast o placenta 36% OF TOTAL body Se associated with GPx (Se is always linked to GPx ) Other selenoprotein other than GPX 2. Thyroid Hormone synthesis: Iodothyronine 5’- Deiodinases removal of iodine from T4 T3 (active form) o Se deficiency Increase T4 Decrease T3 3. Keep the stability of membrane o o Membranes are made of UFA easily oxidized Need antioxidant system to reduce it GPX and other antioxidant like Vit E , SOD, catalase… Though there is overlapping function of GPX and Vit E, but they both are needed to run the job Deficiency: Develop in o premature infants o person with long time Se-free enteral/parenteral solutions symptom: o decline GPX activity in a variety of cell types o fragile RBC membrane not stable o enlarged heart o cardiomyopathy o growth retardation o cataract formation o abnormal placenta retention o deficient spermatogenesis GPX4 in testes o Skeletal muscle degeneration Impaired thyroid hormone activity o Selenoprotein iodothyronine deiodinase convert T4 T3 (most active thyroid hormone) Keshan disease o Degenerative changes in the heart muscle o Due to mutation of virus in the absent of Se o Happen in china Measurement: Activity of GPX Blood selenium not informative Toxicity Intake in excess of 400ug/d = UL Acute poisoning o 1st: GI effects Nausea Vomiting Diarrhea o Hypersalivation o Garlic-smelling breath o hair loss, restlessness, tachycardia, fatigue Chronic poisoning = selenosis o o o Nail, hair changes brittleness & loss Skin lesion Neurological effects Numbness Pain Paralysis Interfere other trace mineral homeostasis: o Reduce Zn absorption o Reduce Fe tissue store o Increase Cu in heart, liver, kidney o *** there is a complex relationship between all minerals Any increment or decrease of any mineral will affect one another Iodine The heaviest element commonly needed by living organism Imp for endocrine system (thyroid hormone) Food source Natural sources of I o Marine organism o Plant grown on I-rich soil Iodized salt o This is due to Iodine deficiency frequent happen in certain area due to geographical factor hardly access to marine food Absorption is reduced in food with goitrogen (phytochemical)甲状腺激素 o o o Brassica vege (cabbage, broccoli, swede, brussels sprouts) Maize Goitrogen interfere Fe absorption ** vegan susceptible to iodine deficiency Inactivated by cooking Requirement Increase in pregnant females (10-20%) o Thyroid hormone increases during pregnant Increase in lactation o Iodine source for infant Metabolism Form: o Iodine convert to iodide ion (I-) absorbed In blood o Circulate in blood to all the tissue in free IDistribution o 80% in thyroid gland For T4 (thyroxine) synthesis o Salivary gland o Gastric mucosa o o Choroid plexus Lactating mammary gland Synthesis of thyroxine o When body need thyroid hormone increase TSH (thyroid-stimulating hormone) stimulate tyrosine-rich thyroglobulin (a protein made by follicular cells of thyroid gland) main structure of thyroid hormone make available for iodination Thyroglobulin is made of Tyrosine (NE amino acid made form melanin) iodine o In the meanwhile, I- is pumped actively into the thyroid follicular lumen o Iodination: Thyroglobulin + iodine -- (iodide peroxidase) monoiodothyronine diiodothyronine triiodothyronine (T3) thyroxine(T4) o o o Thyroid gland produced ratio of thyroid hormone: o 90% T4 (T2 *2) o 10% T3 (T2 + T1) T4 transport Released from follicles to blood transport by “thyroid-binding protein” to all cells of body At target cell: Deiodination of T4 T4 – (deiodinase <Se-containing enzyme>) T3 (most active thyroid hormone) + iodine The consequence of The released iodine conserved and sent back to thyroid gland unused lost in urine or feces o Function: Thyroid hormone o Maintain metabolic rate by Control energy production O2 consumption in cells o Normal growth & development Normal protein metabolism in brain & CNS o For fetus & neonate o Needs Iodine o ** that’s why pregnant & lactating mom needs more Iodine Deficiency Goiter o o o Can happen in both hypo & hyperthyroidism 不可以断定大颈包是 hypo/ hyper Enlarged thyroid gland Due to hypertrophic, hyperplasic change in gland’s follicular epithelium Lack of thyroid hormone pituitary gland produce mre TSH to increase production increase stimulation of the epithelial cells but still cant increase syn thyroxine vicious cycle excess stimulation hypertrophy Cell enlarged due to lack of iodine to complete thyroxine synthetic process Hypothyroidism o Due to Iodine deficiency Or selenium deficiency even in iodine efficient Cannot produce the active thyroid hormone T3 o Characteristic: (low metabolism) Weight gain Lethargy Poor cold tolerance Bradycardia Myxoedema 粘液性水肿 Dif age dif consequence: o Pregnant iodine-deficiency developing embryo/ fetus Suffer neurological deficit Lose their pregnancies Fetus fail to develop and dies in utero o Children / infant Consume iodine deficient diet Fail to grow normally Low development of intellectual Common case: o Eat little iodine + diet rich in Brassica vege Toxicity Hyperthyroidism Toxic modular goiter o Due to excess secretion of T3 & T4 o But the symptom is very dif to hypo-goiter Like bulging eyes Weight loss To test for hyper/hypo: o Look for TSH! Very sensitive indicator Hypo Increased o Our body not enough TH Hyper Absent/ decreased o As our body has more than enough of TH T6- Alcohol The one that can be consumed = ethanol (2 c C2H5OH) o Ethanol= ethyl alcohol o Mostly produced by fermentation of glucose in plant Vegetarian friendly Labeling law: o Needed to indicate % alcohol by volume (abv) in all alcoholic drink 10% abv= 7.9g alcohol/100mL Nutritional value: 7kcal (29kJ)/ g May contain other nutrient since is obtained from plant o But small amt only X depend on alcohol to get these nutrient Propyl alcohol K Riboflavin Niacin Recommendation Intake: Dif type of alcoholic drink if intake size o As we need to look at the ethanol conc Men: 3-4 unit/d Women: 2-3unit/d 2d/week should be alcohol free Pregnant: not more than 2-4 unit/week o Excessive alcohol consumption during pregnancy fecal alcohol syndromes Cause facial deformities & growth prob Short nose Thin upper lip o Indistinct philtrum 人中 (easiest to identify) Flat midface Short palpebral fissure Alcohol causes higher blood alcohol concentrations in your developing baby than in your body because a fetus metabolizes alcohol slower than an adult does. Alcohol interferes with the delivery of oxygen and optimal nutrition to your developing baby. If too much fecal die o Metabolism: Absorbed in stomach & jejunum distribute throughout body water including blood distribute mainly to brain & liver Ethanol is readily absorbed through the entire gastrointestinal tract. It is transported unaltered in the bloodstream and then oxidatively degraded in tissues, primarily the liver, first to acetaldehyde and then to acetate. In tissues other than the liver, as well as in the liver itself, the acetate subsequently is converted to acetylCoA and oxidized via the TCA cycle. At least three enzyme systems are capable of ethanol oxidation: o alcohol dehydrogenase (ADH) o the microsomal ethanol oxidizing system (MEOS; also known as the cytochrome P-450 system) o catalase, in the presence of hydrogen peroxide Of these, the catalase-H2O2 system is the least active, probably accounting for <2% of in vivo ethanol oxidation. Alcohol dehydrogenase (ADH) acetaldehyde o Then broken down again Aldehyde dehydrogenase (ALDH) acetate o These 2 enzyme is mainly found in liver o o o o o o Average 5-10g is metabolized per hour Some excreted in breath monitor alcohol intoxication Ethanol acetaldehyde toxin that get you drunk In liver, further detoxify by ALDH acetic acid excrete in urine So that you may not be drunk anymore Require NAD+ Depletes NAD+ force shit to microsomal system that X need NAD+ = MEOS Also expressed in GIT But significantly different in gender Female lesser ADH in GIT o Young premenopausal femal develop higher blood alcohol than male with equal consumption lower tolerance of alcohol and greater risk of toxic effect in liver Affect other metabolism NAD+ are needed for other reaction the increase ratio of NADH:NAD+ impair TCA cyc;e Gluconeogenesis Fatty acid oxidation o Microsomal ethanol-oxidizing system (MEOS) o Inducible by ethanol to increase efficiency of hepatocyte to metabolize alcohol o A system of alcohol metabolism induced by alcoholics CYP2E1 enzyme help ADH to metabolize ethanol to acetaldehyde The amt of ethanol is too much need another enzyme to help ADH Mostly in liver o Effect on other metabolism It can also accelerate the metabolism of other sub etabolized by microsomal system increase their tolerance as well Fatty acid Aromatic hydrocarbons Steroids Barbiturate drugs Catalase: (not included in MEOS) o Help ADH to convert to acetaldehyde o Mostly found in brain To reduce the hangover symptom Other factors: o Food in stomach can slow alcohol absorption o Smaller ppl have smaller liver metabolize alcohol slower Women has smaller liver than men intoxicate faster o The build up of acetaldehyde leads to headache, nausea & vomit Fatty liver: Impair fatty acid oxidation due to reduce NAD+ o Build up of acetyl-CoA in liver Encourage liver synthesis FA with time lead to TAG accumulation in liver Toxicity Acetaldehyde toxicity Able to attach covalently to proteins protein adduct o If adduct an enzyme impair the enzyme activity Impede formation of microtubules in liver cell o Cuase development of perivenular fibrosis initiate cirrhosis High NADH:NAD+ ratio Metabolic shift to hydrogenation o Account for fatty liver Trhough anabolic activity producing fatty acicds o Lactic acidemia High blood lactate level Increase reduction of pyruvate to lactic acid Slow down hydrogenase reaction of TCA cycle o Accumulation of citrate which positively regulate acetyl-CoA carboxylase Enzyme convert acetyl-CoA malonyl CoA by attaching a carboxyl grp A key regulatory enzyme for synthesis of FA from acetyl0CoA Hence, direct metabolism away from TCA cycle oxidation fatty acid synthesis The effect of NADH on glycerophosphate dehydrogenanse reaction (GPDH) o Favor reduction of DHAP to glycerol-3-phoshpate if NADH conc is high Provide glycerol component in the synthesis of TAG impair gluconeogenesis o Affect glutamate dehydrogenase GluDH reaction o Imp in conversion of Amino acid to their carbon skeleton by transamination & release amino group o o A shift of glutamate and deplete alpha-ketoglutarate which is a major acceptor of amino grp in the transamination of amino acid Several stages : depend on how much alcohol in our blood o Common effect: o Heart beat fast o Facial Flushing: Vasodilation o Anesthetic: CNS depressant o Diuresis: Alcohol act on pituitary gland may lead to dehydration The reactive metabolite led to toxicity: acetaldehyde: o Acute toxicity: Target: CNS suppression Can be seen very fast Sedative & hypnotic effect, cognitive impairment, motor incoordincation, hallucinogenic, euphoriant effect, learning, memory deficit o Chronic toxicity: Target: Liver damage Accumulation of fat o Complex mechanism Oxidative stress, inflammation, necrosis in liver, liver failure, cancer o Teratogenicity: Birth defect o Thiamine deficiency 2 reason o Ethanol reduces thiamine intake & absorption o Increase needed for ethanol metabolism Thiamine needed for GSH production antioxidant needed for ethanol metabolism Consequence: o Wernicke’s encephalopathy o Korsakoff’s psychosis Genetic polymorphisms in alcohol metabolism: East Asian & American Indian o Higher efficiency of ADH Can breakdown ethanol to acetaldehyde faster East Asian: ALDH 2*2 o Less efficient than ALDH2 ALDH2 is the enzyme normally break down acetaldehyde Hence lead to Asian flush syndrome/Asian glow Bcs produce AA very fast that make us drunk AA unable to detoxify efficiently by ALDH2*2 to acetic acid Hence get drunk easily Benefit: Light – moderate consumption of alcohol reduce risk of CHD in men & post-menopausal women mechanism o increase HDL prevent obstruction of blood vessel in heart o polyphenolic comp in wine resveratrol reduce plasma LDL Paracetamol & alcohol chronic alcoholics are at increased risk of paracetamol hepatotoxicity not only following overdose but also its therapeutic use o in chronic alcoholics, CYP2E1 increase o paracetamol will produce toxic damaging liver the paracetamol toxicity is more severe in CYP2E1 increased ppl risk of hepatotoxicity o induction of CYP2E1 by ethanol increases formation of toxic metabolite of paracetamol