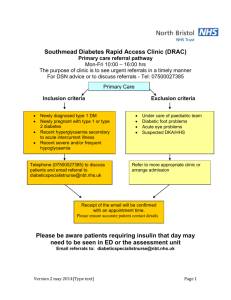
2. Methodology 2.1 The STAR Care Pathway 2.1.1 Development of the STAR Care Pathway The need to address the obstacles to long-term pain management after knee replacement, and to develop a comprehensive care pathway for chronic pain post-TKR, led to the Support and Treatment After Joint Replacement (STAR) trial. This approach involved an initial assessment clinic at 3 months post-operatively to identify patients with pain early on, followed by telephone follow-up appointments. The assessment clinic promotes understanding the underlying reasons for CPSP and referring patients onwards to existing services. These services aim to target those reasons to optimise pain management and reduce adverse outcomes due to pain. Evidently, the design of this care pathway draws on evidence collected from the papers referred to above on the current management of chronic pain after TKR5,6. The development of the intervention was rigorous, involving refinement of the intervention and improving on any issues relating to its implementation before progressing to a randomised controlled trial. Clinicians inputted on the intervention design to ensure the elements of it are appropriate, and clinicians directly involved in its future delivery were consulted to further modify the intervention as appropriate. The intervention was trialled on a small sample of patients with chronic pain after TKR to illuminate any problems in delivery, including how patients respond to it, and offer a chance to rectify these. Examples of these issues included one of the neuropathic pain scoring tools, abbreviated as DN-4, missing patients with clinical symptoms of neuropathic pain. Another clinical neuropathic pain measure, named PainDETECT, was added to the assessment clinic questionnaire and further questionnaires completed by patients during the follow up period. These clinical scoring tools are described in further detail below. Another problem identified was the inconsistency in knee stiffness assessment carried out by the extended scope practitioner (the healthcare professional carrying out the initial assessment clinic. Their role is explained further below) and by the orthopaedic surgeon. This was remedied by supplying the extended scope practitioner (ESP) with a goniometer, a tool which measures range of motion. Testing the intervention delivery and acceptability to patients also aided in the development of training materials for the healthcare professionals that will deliver the intervention in the future. The final stage of development saw health professional stakeholders' views on the implementation of the STAR trial be evaluated to ensure they understood how this intervention would change their work, how they would integrate it into their practice and benefit patients11. 2.1.2 Design of the STAR Care Pathway Study Screening Process: The STAR care pathway study consisted of a multi-centre randomised controlled trial carried out in 8 NHS hospitals in the UK. It aimed to judge whether this care pathway was clinically effective in comparison to usual care for people with chronic pain after knee replacement. Patients who had received a primary TKR for osteoarthritis 2 months prior, at participating sites, were identified and invited to participate. They were sent a screening study pack with a cover letter, patient information leaflet, freepost envelope and a complimentary teabag. The patients were asked to complete and return the screening questionnaire and consent form. The research team scored the Oxford Knee Score (OKS) data from the patients’ responses to identify patients who scored 0-14, indicating pain in their knee post-TKR. The OKS is a clinical scoring tool assessing knee pain. In the screening process, this was adapted into a 7-question score, each question scored from 0-4, yielding a total score of 0-28. 0 indicates severe pain and 28 indicates no pain12. Recruitment Process: Those aged ≥18 years who scored 0-14 on the OKS completed in the screening questionnaire sent to invitees and consented to further contact were eligible for recruitment into the study. Scoring 0-14 was deemed to be relevant due to previous research suggesting that this range represents pain that negatively affects patients' health related quality of life13. Those patients were sent a trial information pack and phoned by a researcher to check if they wished to participate. If so, they carried out the OKS again via telephone to ensure they still met the inclusion criteria. If patients wished to participate, they were required to provide written, informed consent. Participants were further required to complete a detailed baseline questionnaire before being randomly allocates to the STAR pathway (intervention) group or the usual care (control) group12. This screening and recruitment process is discussed by Wylde et al. (2020)14, whereby the detailed questionnaire completed at 13 weeks post-TKR revealed the factors associated with pain and function. More severe pain was associated with poorer general and physical health, more pain worry and lower satisfaction with surgical outcome. More severe functional limitation was associated with higher levels of depression, more pain worry, lower satisfaction with surgical outcome and higher pain acceptance. These outcomes became the targets for patient-specific interventions aiming to improve CPSP and patient outcomes. STAR Trial Procedure 363 patients were recruited. These participants completed a baseline questionnaire at 13 weeks post-operatively, then were randomly allocated to the STAR pathway group or usual care and informed of their allocation. 242 were allocated to the intervention plus usual care group, while 121 were allocated to usual care alone. Usual care entails entailed a 6-week follow up postoperatively, although one site offered an additional appointment at 3 months12. Those in the STAR intervention group also received usual care in addition. The intervention was carried out by ESPs, which are registered allied healthcare professionals with a specialist training in orthopaedics. Furthermore, all ESPs attended a 1-day training session and received a training manual relating to the assessment clinic. The intervention involved a 1-hour assessment clinic appointment with an Extended Scope Practitioner (ESP) where a clinical history was taken, patient-reported outcome measures were reviewed (Brief Pain Inventory (BPI), Hospital Anxiety and Depression Scale (HADS), painDETECT and Douleur Neuropathique 4 (DN4)18), knee examination is carried out, and radiographs and blood tests are reviewed or carried out12. The BPI is a measurement tool for assessing clinical pain as reported by patients: patients rate the severity of their pain via a pain severity scale and how much their pain affects their daily activities and feelings via a pain interference scale. Both scales are scored from 0-10 (best to worst)15. The HADS is a simple clinical measure of anxiety and depression in patients, comprising 7 questions on anxiety and 7 questions on depression and both scales are scored separately from 0-21 (no to severe depression/anxiety). PainDETECT and DN4 are neuropathic screening questionnaires. PainDETECT contains 9 items: 7 on sensory sytmptoms, one on pain course pattern and another on pain radiation17. DN4 is a 10-item questionnaire split into questions on symptoms and physical exam signs18. The outcomes of the assessment clinic were recorded on a standardised proforma and based on this, participants were referred to appropriate existing services for further treatment. This included referral to a surgeon, physiotherapy, GP for treatment of depression or anxiety and/or pain specialists for neuropathic pain or Complex Regional Pain Syndrome. The assessment clinic was held 3-4 months after surgery if possible. Participants then received up to a maximum of six telephone follow-up consultations over 12 months from the ESP to monitor how referrals are progressing and to make other referrals if necessary. These consultations were also recorded on a standardised proforma. Outcome measurements were self-reported by patients when they completed the baseline questionnaire at 3 months after their surgery, then also at 9 months after surgery and 15 months after surgery (12 months after randomisation). The co-primary outcomes were pain severity and interference, assessed using the BPI14. The mean BPI pain severity and frequency scores at 12 months after randomisation will be compared between the usual care and intervention groups12. 2.2 Comparing Outcomes Within the Intervention Group 2.2.1 Reviewing and Coding the STAR Intervention Data In order to examine the impact of treatments (from referrals) on patient reported outcomes, namely BPI scores, the data collected on patients’ referrals from the assessment clinic and subsequent follow-up telephone calls with ESPs will be analysed. The data was made available in a Microsoft Excel spreadsheet presenting which referrals, out of all those available to be made from the assessment clinic, were selected for all participants (for whom data was available and complete) in one worksheet, and in another worksheet the data recorded on participants’ follow-up calls. The worksheet presenting the assessment clinic data was filtered to show only which referrals were made for each participant and exclude all other data recorded from the clinic. Similarly, the worksheet containing the data on follow-up calls was reviewed to remove data identifying participants and healthcare professionals involved in their care to ensure the data is anonymous, and to ensure that, where information was available to do so, dates recorded were consistent. To process the data pertinent to my research project, a new worksheet was created, titled “Project Data”, where the follow-up call data was coded according to participant ID, what referrals they received, a variable reflecting whether the referral was received or not (Yes/No/Unknown/N/A), treatment received for the referral and the outcome of this. The range of number of referrals participants received was 1-9. In addition to this, a variable reflecting the overall outcome subjectively (Improved/Stayed the same/Worse/Unknown) was included. The status of the referral was judged from the follow up call data – where the ESP recorded that a participant received all their referrals, then ‘Yes’ was selected for each referral. Where an ESP recorded that some or all of the referrals were not received then ‘No’ was selected for all/the relevant referrals for that participant. Where data from the follow-up calls was incomplete and the status of referrals for that participant was unclear, then ‘Unknown’ was selected. ‘N/A’ was applied to some of the ‘referrals’ that fell under the category of “Other” where this did not actually represent a referral to further healthcare. For reference, the below flow-diagram illustrates all possible referrals that could be made from the assessment clinic. Figure 1 - Flow diagram demonstrating all referrals made from STAR intervention assessment clinic and the number of participants who received each referral. Similarly, the follow up call free-text data for each participant was read and where details on treatment received and outcome of this for each referral was available, it was recorded. Where this information was not available, this was recorded as “Not recorded”. The overall outcome (Improved/Stayed the Same/Worse/Unknown) was subjectively judged from the comments that ESPs made in the follow up call data. “Improved” was noted when there was clear mention of the participant’s symptoms and function being better than their pre-operative state in the follow-up call comments. “Stayed the Same” was recorded when follow-up call comments suggested that compared to their pre-operative state, a patient’s symptoms largely remained the same or similar. “Worse” was only noted when a patient reported that their symptoms, function and ability had deteriorated in comparison to their pre-operative state. For some participants, the follow-up call data was incomplete or lacked the necessary detail to record whether a patient improved, stayed the same or became worse, so “Unknown” was recorded under “Overall Outcome”. 2.2.2 Descriptive Analysis of Referrals Made in the STAR Intervention Group All referrals made for each participant were listed in a new Excel worksheet alongside whether the referral was received or not using the aforementioned variable for this. The “Sort and Filter” Excel function was used to separately select each individual referral type to count the total number of the individual referrals and the number of “Yes”, “No”, “Unknown” and “N/A” options for whether the referral was received, which builds on the data in Figure 1. From the “Project Data” worksheet, the total number of participants who received all their referrals, and those who did not, was counted. Within the group of participants who received all their referrals, the number of each “Overall Outcome” variable (Improved/Stayed the same/Worse/Unknown) was counted. The same was done for the participants who did not receive all of their referrals, so that the two groups can be compared. 2.2.3 Statistical Analysis of Outcomes for Participants in the Intervention Group To perform statistical analysis of outcomes for participants in the STAR trial who received referrals, and compare outcomes between participants who received all their referrals and those who did not, BPI pain severity and pain interference scores, collected from the 12-month trial questionnaire, were used. BPI scores were available for 216 participants of the 233 who attended the assessment clinic as not all patients who attended the intervention completed a 12-month questionnaire. To determine what statistical test to apply to the BPI scores, a histogram was first derived for BPI pain interference scores and for pain severity scores to determine if the data was normally distributed or not. Based on this, a parametric (T-test) or non-parametric test (Mann-Whitney U test) would be performed on the data. BPI scores were formatted by referral group as depicted in Figure 1 (i.e. surgeon, GP, pain clinic, physiotherapy, follow-up calls to monitor pain and “other” referrals). For each referral type, a table was made with two columns: referral received and referral not received. The BPI scores of the participants who received the individual types of referrals within each referral group, and those who did not (i.e. that referral was selected for them at the intervention assessment clinic but they did not receive it), were listed in their respective columns. For each referral group, a table with BPI pain severity and a table for pain interference scores was produced, on which a Mann-Whitney U test was carried out, yielding a P value which represented whether, for that referral group, there was a statistically significant difference between the BPI scores of those who received that referral and those who did not. Looking more closely at the outcomes within each individual referral type, the above process of formatting BPI scores on which to perform a Mann Whitney U test was repeated for the individual referrals within the referral groups (as in Figure 1) to establish whether any individual referrals yielded a statistically significant difference in BPI scores between participants that received the referral and those who did not. Descriptive statistics were also carried out on the tables of BPI scores as mentioned above.