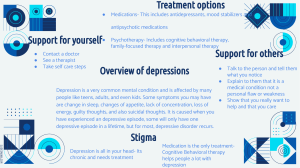
Psychopharmacology Chapter 5—Medication Nonadherence Activation—acute onset anxiety Chapter 6—Preliminary Diagnostic Considerations Agonist—drug or chemical that acts on receptor to mimic the effects of a naturally occurring substance or of another chemical Antagonist—substance or drug capable of blocking the activity of an agonist without exerting any effect itself. Differential diagnosis—the process of considering diagnostic possibilities based on comparison of signs and symptoms of two of more disorders or diseases. Egodystonic—symptoms subjectively experienced by the patient as being aversive, undesirable or alien. Egosyntonic—signs or symptoms judged to be pathological by others but not experienced as distressing by the patient. Etiology—the study of the causes of disorders and diseases Pathophysiology—the underlying physiological dysfunction or disease that contributes to the manifest symptoms of the disease Target symptoms—in this book the distinctive symptoms that are the focus of medication treatment Toxicity—serious medication related adverse effects associated with actual or potential damage to tissue, organs, or the entire body system, the toxicity may be directly related to critically elevate blood levels of a drug and may be acute or chronic. Chapter 7—Depressive Disorders Two ways to have a depressive disorder Reactive—reaction to the situations around you and events Endogenous—just appears out of no where Three groups of depressive disorders 1. Reactive dysphoria—relatively low-grade mood changes, sadness, disappointment, despair—that occur in response to minor losses and disappointments. Considered to be normal and appropriate and do not interfere with functioning 2. Grief—uncomplicated bereavement, more prolonged and intensely painful experience. Considered to be normal and appropriate response to major losses such as a death of a loved one or divorce. Lasts usually from 6-12 months or sometimes even years. Occurs in waves, social and occupational functioning can be derailed temporarily 3. Clinical depression—characterized by their intensity, duration, impact on functioning, and a host of symptoms. self-esteem almost always erodes, and true depression is a clearly pathological condition. Results in tremendous personal suffering, can last for months to years and severely affect normal daily functioning. About 25-30% of patients who experience grief develop clinical depression When grief becomes clinical depression Marked erosion of self-esteem Agitation Early morning awakening Serious weight loss Psychotic symptoms Suicidal ideation or attempts Anhedonia (loss of the ability to experience any pleasure) Marked impairment Types of Clinical Depression 1. Major unipolar depression—reactive, biological, reactive-biological, atypical 2. Bipolar disorder—manic and depressive episodes 3. “minor” depressions—dysthymia, chronic residuals of partially recovered major depressions Medical disorders that can cause depression Addison’s disease AIDS Anemia Asthma Chronic fatigue syndrome Chronic infection/inflammation Chronic pain Congestive heart failure Cushing’s disease Diabetes Hypothyroidism Infectious hepatitis Influenza Lyme disease Malignancies (cancer) Malnutrition Multiple sclerosis Parkinson’s disease6 Premenstrual dysphoria Porphyria Restless leg syndrome Rheumatoid arthritis Sleep apnea Syphilis Systemic lupus erythematosus Traumatic brain injury Ulcerative colitis Uremia Biological depression 4 factors 1. Medical illness that leads to systemic changes and ultimately to brain dysfunction. It should be noted that recently it has been found that thyroid dysfunction is a common disorder underlying 5 to 10 percent of serious depressions. Because of this high frequency, a thyroid panel is strongly recommended in all cases of serious depression. 2. Female sex-hormone fluctuation, especially noted postpartum, during menopause, and premenstrually 3. Medications and recreation drugs 4. Endogenous biological depressions. These disorders appear to emerge spontaneously in certain at-risk individuals in the absence of stressful events. The prevailing theory is that such disorders likely reflect a genetically transmitted biological vulnerability that leads to repeated dysfunction of selected neurons in the limbic system and resulting recurring depressive episodes CBT (cognitive behavioral therapy)—the gold stage of depression treatment The depressive triad, negative view of themselves, world, view of the future. Chapter 16 -antidepressants Antidepressants—large important group of medications used to treat depression MAOIS—monoamine oxidase—an enzyme used to break down catecholamines (dopamine, norepinephrine, and serotonin)—has a long list of foods you must avoid while taking this medication—the wine and cheese effect because certain wines and cheeses have these amines that are harmful Six major groups of antidepressants 1. 2. 3. 4. Cyclic antidepressants Selective serotonin reuptake inhibitors (SSRIs) Serotonin and norepinephrine reuptake inhibitors (SNRIs) Norepinephrine reuptake inhibitors (NRIs) 5. Monoamine oxidase inhibitors (MAOIs) 6. Atypicals Types of Cyclic Antidepressants Amitriptyline Clomipramine Desipramine Doxepin Imipramine Nortriptyline Trazodone Brand name Elavil Anafranil Norpramin Silenor Tofranil Pamelor, Aventyl Oleptro Side effects of tricyclic antidepressants—“dirty drug” anticholinergic—dry mouth, dry skin, blurred vision, constipation, paralytic ileus, cessation of movement of the intestines, inability to urinate, ruptured bladder adrenergic—sweating, sexual dysfunction, orthostatic hypertension antihistaminic—sedation and weight gain miscellaneous—lowered seizure threshold, cardiac arrhythmia, hepatitis, agranulocytosis, rashes, sweating, anxiety, elevated heart rate. Dirty drug—effects more receptors that just the intended one—hence the side effects SSRIs--have the same effects as tricyclics but have less side effects and are safer in dosage --the drugs have different half-lives which determine how long they take to work and how long they stay in your system, they have sexual dysfunction side effects fluoxetine—Prozac citalopram—Celexa escitalopram—Lexapro fluvoxamine—Luvox paroxetine—Paxil sertraline—Zoloft SSRIs Side effects—tend to be related to increased serotonin activity nausea gastrointestinal upset sweating anxiety insomnia headache restlessness sexual dysfunction dry mouth sedation blurred vision After several months it can begin to cause loss of energy, passivity, apathy, decreased pleasure, decreased libido Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs)—dual action antidepressants Venlafaxine—Effexor Desvenlafaxine—Pristiq Duloxetine—Cymbalta Levomilnacipran—Fetzima Mirtazapine—Remeron MAOIs—used mainly when other antidepressants have failed in the treatment of major depression and panic disorder. Not used commonly due to the severity of the side effects including hypertension, cerebral hemorrhage, or even death Phenelzine—Nardil Tranylcypromine—Parnate Three phases of treatment of major depression Acute treatment—begins with the first dose and extends until the patient is asymptomatic Continuation treatment—continue treatment for a minimum of six months to avoid a relapse Maintenance treatment—continued lifetime treatment o First episode—at the end of the continuation phase, gradually reduce the dose and assuming no return of depressive symptoms discontinue. Educate the patient to be alert to nay signs of recurrence and should this occur, as soon as possible reinstate treatment o Second episode—with risk factors: recommend lifelong medication treatment to prevent recurrence. Without risk factors: gradually discontinue medications o Third or subsequent episodes: recommended lifelong medication treatment Three side effects that can lead to patient discontinuation 1. Activation—acute onset side effect seen within the first few hours after starting an antidepressant or when doses are increased. It presents with nervousness and anxiety 2. Switching—when a person being treated with an antidepressant is provoked into a manic state. One significant difference between activation and switching is that generally switching does not occur until after several weeks of antidepressant treatment a. Inorgasmia—difficulty achieving an orgasm despite adequate arousal 3. Weight gain Treatment resistant depression—refers to a depression that has failed to respond adequate trials of two or more antidepressant ECT (electroconvulsive therapy)—shock therapy for severe depression and mood disorders, or depression with psychotic features such as delusions Chapter 8—Bipolar Disorder Hypomania—the stage between manic and neutral Mania—the highest stage of “feeling good” Bipolar 1—must meet the criteria for atleast one manic state Bipolar 2—at least one hypomanic episode and at least one major depressive episode but has NEVER reaches a full manic episode Stages of Acute Mania 1. Stage 1 (corresponds with hypomania) a. Increased psychomotor activity b. Emotional lability c. Euphoria or grandiosity d. Coherent but tangential thinking 2. Stage 2 (frank mania) a. Increased psychomotor activity b. Heightened emotional lability c. Hostility, anger, impulsivity d. Assaultive or explosive behavior e. Flight of ideas, cognitive disorganization f. Possible grandiose or paranoid delusions 3. Stage 3 (exhibited by some patients) a. Frenzied psychomotor activity b. Incoherent thought processes c. Ideas of reference, disorientation, delirium d. Florid psychosis (indistinguishable from other psychotic disorders, although usually mood congruent) Medical conditions associated with mania Central nervous system trauma, for example, post-stroke Metabolic disorders such as hyperthyroidism Infections diseases such as encephalitis Seizure disorders Central nervous system tumor Drugs that can induce mania Stimulants (amphetamines) Antidepressants (especially tricyclic antidepressants) SAM-e Antihypertensives Corticosteroids (prednisone) in higher doses Anticholinergics (benztropine, trihexyphenidyl) Thyroid hormones (levothyroxine) Bipolar I Disorder—one or more manic episodes, there may be preceding or subsequent episodes of hypomania or depression. Bipolar II Disorder—one or more depressive episodes and at least one episode of hypomania Rapid cycling—at least four episodes of mania, hypomania, or major depression in the previous twelve months Cyclothymia disorder—numerous periods of alternating depressive symptoms with hypomanic symptoms of at least two years duration that do not meet criteria for either major depression or hypomania Criteria History of numerous periods of alternating depressive and hypomanic symptoms Symptoms do not meet criteria for a hypomanic, manic, or depressive mode Not due to organic factors, substance abuse, medical condition, or other psychiatric disorder Chapter 17—Bipolar Medication Side effects of Lithium Gastrointestinal o Nausea o Vomiting o Diarrhea Nervous system and neuromuscular o Headache o Lethargy o Muscle weakness Endocrine o Clinical hypothyroidism o Goiter Renal o Interference or alteration in normal kidney functioning can potentially lead to a buildup of lithium Hematological o a benign reversible increase in white blood cell count occurs frequently with lithium treatment Cardiovascular o Serious cardiac symptoms are rare but sometimes minor changes on an EKG are present Dermatological o Rash o Acne-like lesions Weight gain o Very common side effect, up to twenty pounds weight gain in 20% of patients Teratogenicity o Carries risk during pregnancy Monitoring Blood Levels o Necessary to maintain a safe and therapeutic dosage Three anticonvulsants Carbamazepine—second line agent for mania as well as mixed episodes o Side effects—sedation, dizziness, drowsiness, blurred vision, incoordination, nausea, vomiting, diarrhea, abdominal pain, itching rash, hives Divalproex—First line agents for mania, recommended for mixed episodes and rapid cycling o Side effects—fatigue, dizziness, nausea, vomiting, indigestion Lamotrigine—used for acute maintenance therapy, first line treatment for bipolar depression, second line treatment for rapid cycling o Side effects—dizziness, headache ataxia, drowsiness, tremor nausea, vomiting, Steven Johnson’s syndrome can occur in rare conditions Chapter 12—PTSD Symptoms of PTSD Persistent reexperiencing of the trauma o Distressing intrusive recollections of the event (images, affects, conditions) o Recurring nightmares regarding the trauma o “flashbacks” or déjà vu (sensations as if the traumatic episode were happening in the present) Increased arousal o Sleep disturbances o Startle response o Irritability o Hypervigilance Transient psychotic symptoms o Derealization o Illusions o Hallucinations (visual or auditory) Avoidance o Avoiding discussion of the traumatic events o Avoiding activities or people and places that could provoke recollections of the trauma o General social withdrawal Numbing o Blunted affective responses o Feelings of emptiness o Feelings of estrangement or detachment o Clouding of consciousness Associated features o Major depression o Panic attacks o Substance abuse (often seen as an attempt to “self-medicate” to reduce anxiety or intrusive experiences) Six models in which biology can potentially be altered by psychological stress 1. Attachment and the repetition compulsion—due to early severe child abuse or neglect may leave not only emotional scars, but also neurobiology may be altered, can lead to increased need for attachment 2. Attachment and impaired affect modulation—traumatic experience early in life which may lead to inadequate attachment and bonding, especially true in neglected children 3. Hyperarousal—behavioral reactions—initially hypervigilance or arousal and ultimately profound state of withdrawal 4. Intrusive symptoms—flashbacks 5. Acute toxic levels of glutamate and cortisol—after a severe trauma marked increases in the neurotransmitter glutamate, and the stress hormone cortisol may reach toxic levels and damage parts of the brain associated with affect regulation 6. Kindling—repeated episodes of trauma change brain functioning