CRANIOMAXILLOFACIAL TRAUMA
Is the Mandible Injury Severity Score a
Valid Measure of Mandibular Injury
Severity?
Rodney N. Nishimoto, DMD, MD,*
Thomas B. Dodson, DMD, MPH,y and Melanie S. Lang, DDS, MDz
Purpose:
Developing a valid method for assessing mandibular injury severity could permit standardized
comparisons of treatment-specific outcomes between and among various mandibular fracture studies. The
study purpose was to assess the validity of the Mandible Injury Severity Score (MISS) developed by Shetty
et al (J Oral Maxillofac Surg 65:663, 2007) by measuring the association between the MISS and postoperative complications, operative time, and length of hospital stay (LOS) after operative treatment of isolated
mandibular fractures.
Materials and Methods:
The authors designed and implemented a retrospective cohort study and
enrolled a sample derived from patients treated for isolated mandibular fractures at Harborview Medical
Center (Seattle, WA) by the oral and maxillofacial surgery service from June 2012 through December
2016. The primary predictor variable was the MISS. The primary outcome variable was postoperative
complication (yes or no). Secondary outcome variables were operative time and LOS. Descriptive, bivariate, and multiple logistic regression statistics were computed to measure the association between the
MISS and postoperative complications. The level of statistical significance was set at a P value less than
or equal to .05.
Results: The study sample was composed of 415 patients with a mean age of 32.7 14.3 years and 80%
were men. The average MISS was 13.4 3.5 (range, 6 to 25). The postoperative complication rate was
21%. The average MISS was significantly higher in patients with postoperative complications than in
patients without complications (16.3 3.3 vs 12.6 3.1; P < .001). In the adjusted model, postoperative
complications were significantly associated with an increasing MISS (odds ratio [OR] = 1.4; 95% confidence interval [CI], 1.3-1.6; P < .001) and open treatment (OR = 7.6; 95% CI, 1.6-35.6; P = .01). The
MISS was positively correlated with operative time (r = 0.529; P < .001) and LOS (r = 0.114; P = .02).
Conclusion:
The results of this study suggest that the MISS may be a valid measurement of mandibular
injury severity as evidenced by the positive correlation between the MISS and postoperative complications, duration of operation, and LOS.
Ó 2018 American Association of Oral and Maxillofacial Surgeons
J Oral Maxillofac Surg 77:1023-1030, 2019
Management of isolated mandibular fractures remains
controversial, with highly variable outcome data and
complication rates.1-4 Because of the frequency of
mandibular fractures, considerable research has been
devoted to identifying ideal treatment protocols.2
Although these studies have been useful in improving
Received from the Department of Oral and Maxillofacial Surgery,
University of Washington School of Dentistry, Seattle, WA.
Address correspondence and reprint requests to Dr Lang: Department of Oral and Maxillofacial Surgery, University of Washington
*Resident.
School of Dentistry, 1959 NE Pacific Street, Health Sciences Center
yProfessor and Chairman.
B-241, Box 357134, Seattle, WA 98195-7134; e-mail: drmelslang@
zClinical Assistant Professor.
gmail.com
Conflict of Interest Disclosures: None of the authors have any
Received October 9 2018
relevant financial relationship(s) with a commercial interest.
Accepted November 30 2018
An abstract for this article was presented at the 2018 Annual Meeting
Ó 2018 American Association of Oral and Maxillofacial Surgeons
of the American Association of Oral and Maxillofacial Surgeons in
Chicago, IL (J Oral Maxillofac Surg 76[suppl]:e10, 2018).
0278-2391/18/31295-3
https://doi.org/10.1016/j.joms.2018.11.027
1023
1024
the efficacy of mandibular fracture treatment, their
utility in directing treatment decisions has been
limited by the failure to measure and control for fracture severity as a confounding variable.5,6
Oral and maxillofacial surgeons assess the severity
of mandibular fractures by assessing anatomic
fracture-specific characteristics, such as number of
constituent fractures, degree of displacement, presence versus absence of teeth, occlusion, and soft tissue involvement.2,7,8 The degree to which individual
surgeons weigh each characteristic in their summary
assessment of fracture severity differs and could
explain why the management and outcomes of
similar fractures can vary.2,8
The Mandible Injury Severity Score (MISS) developed by Shetty et al1 converts numerous disparate
anatomic and clinical characteristics of mandibular
fractures into a single numeric value. If the MISS is a
valid measurement of mandibular injury severity,
then it could be used to predict outcomes, allocate resources, and produce a standard measure of fracture
severity to compare different treatment alternatives.
To date, no external study has validated the MISS in
adult patients with isolated mandibular fractures.1,6,9
The purpose of this study was to answer the
following clinical question: in patients with isolated
mandibular fractures, is the MISS associated with postoperative complications, operative time, and length of
hospital stay (LOS)? The authors hypothesized that an
increasing MISS is positively correlated with the frequency of postoperative complications, operative
time, and LOS. The specific aims of the study were
to 1) compute the MISS and 2) measure the association between the MISS and postoperative complications, duration of operation, and LOS. A positive
correlation between the MISS and frequency of postoperative complications, duration of operation, and
LOS would suggest that the MISS may have validity in
quantifying mandibular fracture severity.
Materials and Methods
STUDY DESIGN AND SAMPLE DESCRIPTION
The authors designed and implemented a retrospective cohort study. Because of the retrospective
nature of this study, it was granted an exemption in
writing by the institutional review board of the University of Washington (Seattle, WA; number 51070). The
study sample was derived from the population of
patients treated for isolated mandibular fractures at
Harborview Medical Center (HMC; Seattle, WA) by
the oral and maxillofacial surgery (OMS) service from
June 1, 2012 through December 31, 2016. Patients
were identified from HMC billing records using the
following American Medical Association Current
Procedural Terminology classification codes: 21450
VALIDITY OF MANDIBLE INJURY SEVERITY SCORE
(closed treatment of mandibular fracture; without
manipulation), 21451 (closed treatment of mandibular
fracture; with manipulation), 21452 (percutaneous
treatment of mandibular fracture; with external fixation), 21453 (closed treatment of mandibular fracture;
with interdental fixation), 21454 (closed treatment of
mandibular fracture; with external fixation), 21461
(open treatment of mandibular fracture; without interdental fixation), 21462 (open treatment of mandibular
fracture; with interdental fixation), 21465 (open treatment of mandibular condylar fracture), and 21470
(open treatment of complicated mandibular fracture
by multiple surgical approaches, including internal fixation, interdental fixation, and wire if all approaches
were intraoral).
Patients were excluded from the study if 1) they
were younger than 18 years; 2) had a follow-up duration shorter than 4 weeks; 3) had incomplete or
unavailable medical records; 4) had pre-existing
mandibular pathology; 5) had other maxillofacial fractures; or 6) had a mandibular fracture secondary to
gunshot trauma.
STUDY VARIABLES
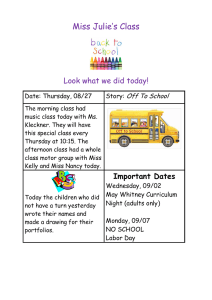
The primary predictor variable was the MISS. To
calculate the MISS, the authors used the following
fracture-specific variables: 1) fracture type (incomplete, simple, comminuted, bone defect); 2) location
of fracture (coronoid, symphysis, parasymphysis, alveolar, body, subcondylar, angle, ramus); 3) nature of occlusion (normal, malocclusion, edentulous); 4) extent
of damage to the soft tissue envelope (closed, open intraorally, open extraorally, intra- and extraoral, soft tissue defect); 5) presence of infection; 6) extent of
interfragmentary displacement (mild [<2 mm], moderate [2 to 4 mm], severe [>4 mm]); and 7) number of
fractures. The MISS was computed for each patient using the method described by Shetty et al1 (Fig 1). For
patients with multiple fractures, the MISS was calculated for the most severe individual fracture and a
value of 4 was added for each additional fracture to
compute the summary score.1 Estimates of interfragmentary displacement were obtained from panoramic
radiographs or computed tomograms. Fractures
without visible step-offs on panoramic imaging were
graded to have displacement smaller than 2 mm. Any
fracture extending through a tooth-bearing segment
was considered open. Fractures extending over 2
contiguous anatomic regions (eg, parasymphysis and
body) were assigned a location corresponding to the
basal region predominately involved by the fracture.1
The primary outcome variable was postoperative
complication (yes or no). Complications included surgical site infection (superficial soft tissue or deep
osseous infections associated with mandibular
1025
NISHIMOTO, DODSON, AND LANG
FIGURE 1. Mandible Injury Severity Score.1,6 For patients with more than 1 mandibular fracture, the Mandible Injury Severity Score is
calculated for the most severe individual fracture and a value of 4 is added for each additional fracture to compute the summary score.
Fractures extending over 2 contiguous anatomic regions are assigned a location corresponding to the basal region predominately involved
by the fracture. Reprinted with permission from Shetty V, Atchison K, Der-Matirosian C, et al: The Mandible Injury Severity Score: Development
and validity. J Oral Maxillofac Surg 65:663, 2007; and Gordon PE, Lawler ME, Kaban LB, Dodson TB: Mandibular fracture severity and patient
health status are associated with postoperative inflammatory complications. J Oral Maxillofac Surg 69:2191, 2011. F, forehead; L1, left symphysis; L2, left parasymphysis; L3, left body; L4, left alveolar; L5, left angle; L6, left ramus; L7, left coronoid; L8, left subcondylar; LD, left dentition; LM, left maxilla; LN, left nose; LO, left orbit; LZ, left zygoma; R1, right symphysis; R2, right parasymphysis; R3, right body; R4, right
alveolar; R5, right angle; R6, right ramus; R7, right coronoid; R8, right subcondylar; RD, right dentition; RM, right maxilla; RN, right nose;
RO, right orbit; RZ, right zygoma.
Nishimoto, Dodson, and Lang. Validity of Mandible Injury Severity Score. J Oral Maxillofac Surg 2019.
fracture sites, hardware, or surgical incision), wound
dehiscence requiring more intervention than local
wound care and antibiotics (hardware removal or
surgical debridement or incision and drainage), hardware failure (loosening or fracture of plates or screws),
malunion or nonunion, osteomyelitis (clinical or radiographic), and malocclusion. Postoperative complications were subcategorized as major or minor. Major
complications were those requiring a hospital admission or a second procedure to be carried out under
general anesthesia in the operating room. Minor
complications were those that could be managed in
the clinic on an outpatient basis.
Secondary outcome variables were operative time
(minutes) and LOS (days). Operative time was
computed from anesthesia or nursing records documenting procedural start and end times. LOS was
computed from hospital admission and discharge records; patients discharged on the same day of surgery
were assigned a LOS of 0 days.
Other study variables were grouped into the
following categories: demographic (age, gender), risk
factor (American Society of Anesthesiologists classification I to V, presence of immune-related disease
[diabetes, human immunodeficiency virus, cancer,
transplantation], presence of substance abuse
[alcohol, tobacco, illicit drugs], fracture etiology [assault, other]), and perioperative (time from injury to
repair [days], incision type [none, intraoral, extraoral,
intra- and extraoral], fixation type [closed treatment
with intermaxillary fixation {IMF}, open treatment
with open reduction and internal fixation with or
without postoperative IMF], intraoperative antibiotics
[administered #1 hour before surgical incision], and
perioperative antibiotics [>24 hours preoperatively
and >24 hours postoperatively if administered]).
DATA COLLECTION, MANAGEMENT, AND
ANALYSES
The authors used a custom data-collection form in
the University of Washington–sponsored Research
Electronic Data Capture (REDCap) database.10 Data
were collected and the MISS was computed by a single
investigator (R.N.N.) using operative, inpatient, and
clinic notes and panoramic and computed tomographic imaging from each patient’s electronic health
record. Descriptive statistics were computed for each
study variable. Bivariate and multiple logistic regression statistics were computed to measure the association between study variables and postoperative
complications using SPSS Statistics 23.0 (IBM Corp,
1026
VALIDITY OF MANDIBLE INJURY SEVERITY SCORE
Table 1. SUMMARY OF STUDY VARIABLES
Table 2. SUMMARY OF STUDY VARIABLES VERSUS
MISS
Study Variables
Study Variables
Demographic variables
Total sample size
Age (yr)
Men
Risk factor variables
ASA class
I
II
III
Immune-related disease (yes)
Substance abuse (yes)
Fracture variables
Etiology
Assault
Other (MVC, fall, sports,
work)
Number of fractures
MISS
Perioperative variables
Time to treatment (days)
Operative time (minutes)
Length of stay (days)
Incision type
None
Intraoral
Extraoral
Intra- and extraoral
Treatment
Closed (IMF)
Open (ORIF or
ORIF + IMF)
Intraoperative antibiotics
Perioperative antibiotics
None
Pre- postoperative
Postoperative complication
Yes
415
32.7 14.3
335 (81)
185 (45)
198 (48)
32 (8)
21 (5)
285 (69)
271 (65)
144 (35)
1.8 0.6
13.4 3.5
10.9 11.1
136.8 65.2
0.4 2.1
92 (22)
299 (72)
14 (3)
12 (3)
92 (22)
323 (78)
415 (100)
184 (44)
231 (56)
88 (21)
Note: Data are presented as mean standard deviation or
number (percentage).
Abbreviations: ASA, American Society of Anesthesiologists
physical status classification; IMF, intermaxillary fixation;
MVC, motor vehicle crash; MISS, Mandible Injury Severity
Score; ORIF, open reduction and internal fixation.
Nishimoto, Dodson, and Lang. Validity of Mandible Injury Severity
Score. J Oral Maxillofac Surg 2019.
Armonk, NY). The level of statistical significance for all
analyses was set at a P value less than or equal to .05.
To measure intra-examiner variability in MISS
scoring, 25 patients were randomly selected and rescored. The intraclass correlation coefficient (ICC)
was computed to assess intra-examiner reliability
(2-way mixed-effects model, single measures, absolute
agreement, ICC [3,1]). Intra-examiner agreement for
Demographic variables
Sample size
Age
Men
Women
Risk factor variables
ASA class
I
II-IV
Immune-related disease
(yes)
Substance abuse (yes)
Fracture variables
Etiology
Assault
Other (MVC, fall, sports,
work)
Number of fractures
Perioperative variables
Time to treatment (days)
Operative time (minutes)
Length of stay (days)
Incision type
None
Intraoral
Extraoral
Intra- and extraoral
Treatment
Closed (IMF)
Open (ORIF or
ORIF + IMF)
Perioperative antibiotics
None
Pre- postoperative
MISS
P Value
415
not applicable
0.017*
.730
13.6 3.4
12.6 3.5
.026y
13.2 3.6
13.6 3.3
15.1 3.7
.240
.026y
13.7 3.5
.015y
13.8 3.3
12.7 3.6
.003y
0.681*
<.001y
0.122*
0.529*
0.114*
.013y
<.001y
.020y
10.5 3.2
14.1 2.9
15.1 4.1
17.6 3.9
<.001y
10.5 3.1
14.3 3.1
<.001y
12.5 3.6
14.1 3.1
<.001y
Note: Data are presented as mean standard deviation.
Abbreviations: ASA, American Society of Anesthesiologists
physical status classification; IMF, intermaxillary fixation;
MVC, motor vehicle crash; MISS, Mandible Injury Severity
Score; ORIF, open reduction and internal fixation.
* By Pearson correlation.
y Statistically significant.
Nishimoto, Dodson, and Lang. Validity of Mandible Injury Severity
Score. J Oral Maxillofac Surg 2019.
MISS scoring was excellent (ICC = 0.93: 95% confidence interval [CI], 0.78-0.97; P < .001).11
Results
During the study interval from June 1, 2012 through
December 31, 2016, 415 patients met the inclusion
criteria. Table 1 presents the descriptive statistics.
The sample’s mean age was 32.7 14.3 years
1027
NISHIMOTO, DODSON, AND LANG
Table 3. BIVARIATE ANALYSES OF ALL STUDY VARIABLES VERSUS POSTOPERATIVE COMPLICATION (YES OR NO)
Study Variables
Demographic variables
Sample size
Age (yr)
Men
Risk factor variables
ASA class
I
II-IV
Immune-related disease (yes)
Substance abuse (yes)
Fracture variables
Etiology
Assault
Other (MVC, fall, sports,
work)
Number of fractures
Perioperative variables
Time to treatment (days)
Operative time (minutes)
Length of stay (days)
Incision type
None
Intraoral
Extraoral
Intra- and extraoral
Treatment
Closed (IMF only)
Open (ORIF or
ORIF + IMF)
Perioperative antibiotics
None
Pre- postoperative
Complication—Yes
Complication—No
P Value
88 (21)
32.7 13.3
76 (86)
327 (79)
32.7 14.6
259 (79)
not applicable
.998
.131
36 (41)
52 (59)
4 (5)
70 (85)
149 (46)
178 (54)
17 (5)
215 (66)
.472
.804
.014*
66 (75)
22 (25)
205 (63)
122 (37)
.031*
2.0 .6
1.8 .6
.027*
9.8 8.4
175.9 63.0
0.5 1.0
11.2 11.8
126.3 61.8
0.4 2.3
.307
<.001*
.713
2 (2)
76 (86)
5 (6)
5 (6)
89 (27)
222 (68)
9 (3)
7 (2)
<.001*
2 (2)
86 (98)
90 (28)
237 (72)
<.001*
26 (30)
62 (71)
158 (48)
169 (52)
.002*
Note: Data are presented as mean standard deviation or number (percentage).
Abbreviations: ASA, American Society of Anesthesiologists physical status classification; IMF, intermaxillary fixation; MVC,
motor vehicle crash; MISS, Mandible Injury Severity Score; ORIF, open reduction and internal fixation.
* Statistically significant.
Nishimoto, Dodson, and Lang. Validity of Mandible Injury Severity Score. J Oral Maxillofac Surg 2019.
(mean standard deviation) and 80% of patients were
men. Assault accounted for 65% of fractures and substance abuse was present in 69% of patients. The
average number of fractures per patient was
1.8 0.6. The average MISS was 13.4 3.5 (range,
6 to 25). The average time to treatment was
10.9 11.1 days and average LOS was
0.4 2.1 days. Open treatment was performed in
78% of patients. All patients received intraoperative
antibiotics in accord with hospital policy. Perioperative antibiotics were given to 56% of patients. Postoperative complications occurred in 21% of patients, of
which 57% were major (hospital admission or second
procedure to be carried out under general anesthesia
in the operating room) and 43% were minor (managed
in the clinic on an outpatient basis).
Table 2 presents bivariate associations between
the study variables and the MISS. Gender,
immune-related disease, substance abuse, fracture
etiology, number of fractures, time to treatment,
operative time, LOS, incision type, fixation type,
and perioperative antibiotics were statistically associated with the MISS.
Table 3 presents a summary of bivariate associations
between the study variables and postoperative
complications (yes or no). Substance abuse, number
of fractures, operative time, incision type, fixation
type, and perioperative antibiotics were statistically
associated with postoperative complications. Open
treatment was significantly associated with an
increased risk for postoperative complications
compared with closed treatment (27 vs 2%; P < .001).
1028
VALIDITY OF MANDIBLE INJURY SEVERITY SCORE
Table 4. MISS VERSUS POSTOPERATIVE
COMPLICATION (YES OR NO)
Table 5. SUMMARY OF MULTIPLE LOGISTIC REGRESSION ANALYSIS
Postoperative Complication
MISS
Yes
No
P Value
16.3 3.3
12.6 3.1
<.001*
Note: Data are presented as mean standard deviation.
Abbreviation: MISS, Mandible Injury Severity Score.
* Statistically significant.
Nishimoto, Dodson, and Lang. Validity of Mandible Injury Severity
Score. J Oral Maxillofac Surg 2019.
Table 4 presents the association between postoperative complications (yes or no) and the MISS. The
average MISS was significantly higher in patients
with postoperative complications than in patients
without
complications
(16.3
3.3
vs
12.6 3.1; P < .001).
Table 5 presents the multiple logistic regression
analysis. Multivariate analysis included the following
variables (reference group within parentheses): MISS
(increasing), age, gender (men), substance abuse
(yes), fracture etiology (assault), fixation type
(open), and perioperative antibiotics (yes). The MISS
(odds ratio [OR] = 1.4; 95% CI, 1.3-1.6; P < .001) and
open treatment (OR = 7.6; 95% CI, 1.6-35.6; P = .01)
were significantly associated with increased risk for
postoperative complications.
Table 6 presents the association between the secondary outcome variables (operative time and LOS)
and the MISS. Operative time (r = 0.529; P < .001)
and LOS (r = 0.114; P = .02) were significantly associated with an increasing MISS.
Discussion
The purpose of this study was to assess the validity
of the MISS by measuring the association between the
MISS and fracture management outcomes (ie, postoperative complications, operative time, and LOS) of
operative treatment of isolated mandibular fractures.
If the MISS were a valid measurement of fracture
severity, the authors hypothesized that the MISS would
be positively correlated with complications, operative
time, and LOS. The specific aims of the study were to
1) compute the MISS and 2) measure the association
between the MISS and postoperative complications,
duration of operation, and LOS.
The study results confirmed the hypothesis that an
increasing MISS is meaningfully associated with an
increased risk for postoperative complications. After
adjusting for age, gender, substance abuse, etiology,
treatment, and perioperative antibiotics, the MISS
was statistically significantly associated with postoper-
Study Variables (Reference)
OR (95% CI)
P Value
MISS
Age
Gender (men)
Substance abuse (yes)
Etiology (assault)
Treatment (open)
Pre- postoperative antibiotics
(yes)
1.4 (1.3-1.6)
1.0 (1.0-1.0)
0.9 (0.4-2.1)
0.7 (0.4-1.4)
0.8 (0.4-1.6)
7.6 (1.6-35.6)
0.6 (0.3-1.1)
<.001*
.890
.893
.359
.520
.010*
.077
Abbreviations: CI, confidence interval; MISS, Mandible
Injury Severity Score; OR, odds ratio.
* Statistically significant.
Nishimoto, Dodson, and Lang. Validity of Mandible Injury Severity
Score. J Oral Maxillofac Surg 2019.
ative complications (OR = 1.4; 95% CI, 1.3-1.6;
P < .001) and open treatment (OR = 7.6; 95% CI, 1.635.6; P = .01). The MISS also was significantly associated with increased operative time (r = 0.529;
P < .001) and LOS (r = 0.114; P = .02). The results of
this study suggest that the MISS may be a valid measurement of mandibular injury severity as evidenced
by the positive correlation between the MISS and postoperative complications, duration of operation,
and LOS.
The MISS was developed by Shetty et al1 as a system
for converting multiple anatomic and clinical characteristics of isolated mandibular fractures that
contribute to their severity into a single numeric
score. Individual components of the MISS are summarized by the acronym FLOSID (fracture type [F], location of fracture [L], nature of occlusion [O], extent
of damage to the soft tissue envelope [S], presence
of infection [I], and extent of interfragmentary
displacement [D]), with the elements of each component assigned a numeric weight depending on their
perceived contribution to fracture severity.1 In the
original study, the MISS was found to have a statistical
association with surrogate markers of injury severity,
Table 6. OPERATIVE TIME AND LENGTH OF STAY
VERSUS MISS
Study Variables
Operative time (minutes)
Length of stay (days)
MISS
P Value
0.529*
0.114*
<.001y
.02y
Abbreviation: MISS, Mandible Injury Severity Score.
* By Pearson correlation.
y Statistically significant.
Nishimoto, Dodson, and Lang. Validity of Mandible Injury Severity
Score. J Oral Maxillofac Surg 2019.
1029
NISHIMOTO, DODSON, AND LANG
such as sensory nerve deficit, need for hospitalization
after surgery, and pain at 1-month follow-up; however,
the study did not show a meaningful association between the MISS and clinical indicators of postoperative wound healing complications (infection,
nonunion, malunion, malocclusion).1 Gordon et al6
conducted a case-and-control study in adults ($18 yr
old) with isolated mandibular fractures and found
that an increasing MISS and pre-existing medical problems were associated with an increased risk for postoperative inflammatory complications (recurrent
swelling, fever, increased pain, or trismus; wound
dehiscence with purulent drainage; exposed or infected hardware; abscess formation; radiographic evidence of osteomyelitis; and presence of a fistula)
after operative treatment. Christensen et al12 conducted a retrospective study to identify risk factors for major complications (hospital readmission; return to the
operating room for a second procedure; or prolonged,
unexpected postoperative stay >24 hours) developing
after the operative treatment of isolated mandibular
fractures in adult patients and did not find a relevant
association between the MISS and major postoperative
complications. The study did not include complications treated in the outpatient setting and excluded
fractures managed by closed treatment with IMF, making the study’s association between the MISS and complications difficult to interpret.12 Swanson et al9
studied the application of the MISS in a cohort of pediatric (<18 yr old) patients treated for mandibular fractures and found that complications (unerupted teeth,
facial asymmetry, hyperplasia, restricted movement,
malocclusion, temporomandibular joint dysfunction,
exposure of hardware, dystonia, gingival recession,
and periodontal bone loss) were meaningfully associated with an increasing MISS. To date, the MISS has
been used in several studies to control for fracture
severity in treatment-specific outcomes research,
develop a model for identifying patients suitable for
outpatient management of mandibular fractures, and
correlate fracture severity with alcohol use and interpersonal violence.13-16
Currently, most studies attempt to classify fracture
severity by using multiple variables (eg, open or
closed, tooth in the line of fracture, number of fractures, displacement). As such, one routinely needs
several variables to describe fracture severity. The power of a study is based on the sample size, the size of
the difference between groups, and the number of variables in the statistical model. More variables mean less
power for a given sample size. The major advantage of
using a single variable (MISS) to score mandibular fracture severity is that it improves the efficiency of a
study. In other words, one could detect a smaller difference between treatment groups for a given sample or
one could enroll a smaller sample for a given prespeci-
fied difference between study groups. Alternatively,
one could categorize the fracture severity score (eg,
simple, intermediate, or complex). However, definitions of these 3 severity categories can vary among
studies. In addition, categorical variables, when
compared with a continuous variable (MISS), are less
efficient (eg, more patients are needed to detect relevant differences when using a categorical variable
compared with a continuous variable). In addition, if
one collects the outcome as a continuous variable,
then it can be converted to a categorical variable. A categorical variable cannot be converted to a continuous
variable. In essence, severity scoring systems aim to
convert multivariate data into a single meaningful index of severity that can increase statistical power in
data analyses.17
The strengths of this study include a large generalizable sample with demographics and complication rate
comparable to previous studies, inclusion of all fracture types (condylar and non-condylar fractures), and
treatments (open and closed), and multivariate statistical analysis and calculation of the ICC.6,12,18,19
Weaknesses of the study include the retrospective
design, limitation of the study sample to patients
treated by the OMS service at HMC, and treatment
performed by multiple OMS attending and resident
surgeons with different levels of experience from
2012 to 2016.
Incorporation of a validated severity scoring system
into the management and study of isolated mandibular
fractures is long overdue. The ability to objectively
quantify the nature and extent of injury into a single
score will allow surgeons to communicate the
complexity of injury, predict outcomes, guide treatments, and stratify patients in clinical research.1 The
results of this study suggest that the MISS is a valid measurement of mandibular fracture severity that is positively correlated with increased
risk for
postoperative complications and can be used in
evidence-based decision making and patient-oriented
clinical research.
References
1. Shetty V, Atchison K, Der-Matirosian C, et al: The Mandible
Injury Severity Score: Development and validity. J Oral Maxillofac Surg 65:663, 2007
2. Ellis E: An algorithm for the treatment of noncondylar mandibular fractures. J Oral Maxillofac Surg 72:939, 2014
3. Nasser M, Pandis M, Fleming PS, et al: Interventions for the management of mandibular fractures. Cochrane Database Syst Rev 7:
CD006087, 2013
4. Joos U, Meyer U, Tkotz T, et al: Use of a mandibular fracture
score to predict the development of complications. J Oral Maxillofac Surg 57:2, 1999
5. Dodson TB: Discussion: Complication rates associated with
different treatments of mandibular fractures. J Oral Maxillofac
Surg 58:280, 2000
6. Gordon PE, Lawler ME, Kaban LB, Dodson TB: Mandibular fracture severity and patient health status are associated with
1030
7.
8.
9.
10.
11.
12.
postoperative inflammatory complications. J Oral Maxillofac
Surg 69:2191, 2011
Shetty V, Atchison K, Der-Martirosian C, et al: Determinants of
surgical decisions about mandible fractures. J Oral Maxillofac
Surg 61:808, 2003
Shetty V, Atchison K, Belin TR, et al: Clinician variability in characterizing mandible fractures. J Oral Maxillofac Surg 59:254,
2001
Swanson EW, Susarla SM, Ghasemzadeh A, et al: Application of
the Mandible Injury Severity Score to pediatric mandibular fractures. J Oral Maxillofac Surg 73:1341, 2015
Harris PA, Taylor R, Thielke R, et al: Research Electronic Data
Capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics
support. J Biomed Inform 42:377, 2009
Cicchetti DV: Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 6:284, 1994
Christensen BJ, Mercante DE, Neary JP: Risk factors for severe
complications of operative mandibular fractures. J Oral Maxillofac Surg 75:787.e1, 2017
VALIDITY OF MANDIBLE INJURY SEVERITY SCORE
13. Shetty V, Atchison K, Leathers R: Do the benefits of rigid internal
fixation of mandible fractures justify the added costs? Results
from a randomized controlled trial. J Oral Maxillofac Surg 66:
2203, 2008
14. Ward NH, Wainwright DJ: Outcomes research: Mandibular fractures in the diabetic population. J Craniomaxillofac Surg 44:763,
2016
15. Haq J, Olding J, Chegini S, et al: Development of a financially
viable model for the management of mandibular fractures as
day cases in a level 1 major trauma centre. Br J Oral Maxillofac
Surg 55:618, 2017
16. O’Meara C, Withersppon R, Hapangama N, et al: Mandible fracture severity may be increased by alcohol and interpersonal
violence. Aust Dent Assoc 56:166, 2011
17. Indrayan A: Medical Biostatistics (ed 3). Boca Raton, FL, CRC
Press, 2013, pp 312–313
18. Dillon JK, Christensen B, McDonald T, et al: The financial burden
of mandibular trauma. J Oral Maxillofac Surg 70:2124, 2012
19. Gutta R, Tracy K, Johnson C: Outcomes of mandible fracture
treatment at an academic tertiary hospital: A 5-year analysis. J
Oral Maxillofac Surg 72:550, 2014