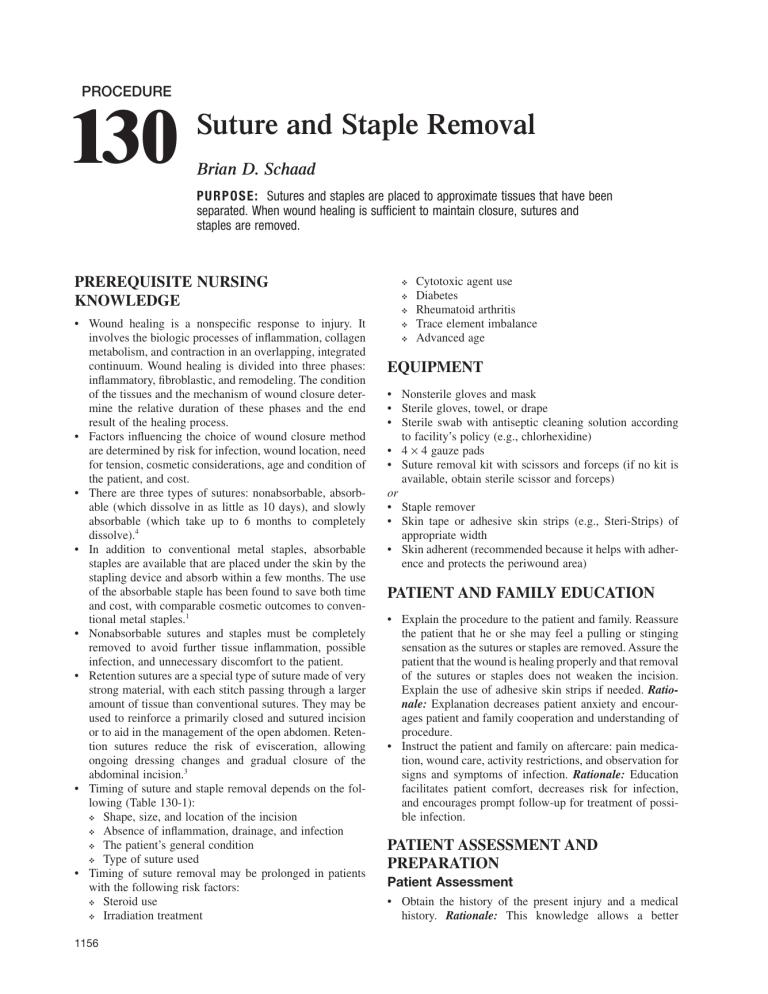
PROCEDURE 130 Suture and Staple Removal Brian D. Schaad PURPO SE: Sutures and staples are placed to approximate tissues that have been separated. When wound healing is sufficient to maintain closure, sutures and staples are removed. PREREQUISITE NURSING KNOWLEDGE ❖ • Wound healing is a nonspecific response to injury. It involves the biologic processes of inflammation, collagen metabolism, and contraction in an overlapping, integrated continuum. Wound healing is divided into three phases: inflammatory, fibroblastic, and remodeling. The condition of the tissues and the mechanism of wound closure determine the relative duration of these phases and the end result of the healing process. • Factors influencing the choice of wound closure method are determined by risk for infection, wound location, need for tension, cosmetic considerations, age and condition of the patient, and cost. • There are three types of sutures: nonabsorbable, absorbable (which dissolve in as little as 10 days), and slowly absorbable (which take up to 6 months to completely dissolve).4 • In addition to conventional metal staples, absorbable staples are available that are placed under the skin by the stapling device and absorb within a few months. The use of the absorbable staple has been found to save both time and cost, with comparable cosmetic outcomes to conventional metal staples.1 • Nonabsorbable sutures and staples must be completely removed to avoid further tissue inflammation, possible infection, and unnecessary discomfort to the patient. • Retention sutures are a special type of suture made of very strong material, with each stitch passing through a larger amount of tissue than conventional sutures. They may be used to reinforce a primarily closed and sutured incision or to aid in the management of the open abdomen. Retention sutures reduce the risk of evisceration, allowing ongoing dressing changes and gradual closure of the abdominal incision.3 • Timing of suture and staple removal depends on the following (Table 130-1): ❖ Shape, size, and location of the incision ❖ Absence of inflammation, drainage, and infection ❖ The patient’s general condition ❖ Type of suture used • Timing of suture removal may be prolonged in patients with the following risk factors: ❖ Steroid use ❖ Irradiation treatment ❖ 1156 ❖ ❖ ❖ Cytotoxic agent use Diabetes Rheumatoid arthritis Trace element imbalance Advanced age EQUIPMENT • Nonsterile gloves and mask • Sterile gloves, towel, or drape • Sterile swab with antiseptic cleaning solution according to facility’s policy (e.g., chlorhexidine) • 4 × 4 gauze pads • Suture removal kit with scissors and forceps (if no kit is available, obtain sterile scissor and forceps) or • Staple remover • Skin tape or adhesive skin strips (e.g., Steri-Strips) of appropriate width • Skin adherent (recommended because it helps with adherence and protects the periwound area) PATIENT AND FAMILY EDUCATION • Explain the procedure to the patient and family. Reassure the patient that he or she may feel a pulling or stinging sensation as the sutures or staples are removed. Assure the patient that the wound is healing properly and that removal of the sutures or staples does not weaken the incision. Explain the use of adhesive skin strips if needed. Rationale: Explanation decreases patient anxiety and encourages patient and family cooperation and understanding of procedure. • Instruct the patient and family on aftercare: pain medication, wound care, activity restrictions, and observation for signs and symptoms of infection. Rationale: Education facilitates patient comfort, decreases risk for infection, and encourages prompt follow-up for treatment of possible infection. PATIENT ASSESSMENT AND PREPARATION Patient Assessment • Obtain the history of the present injury and a medical history. Rationale: This knowledge allows a better 130 Suture and Staple Removal TABLE 130-1 Timing of Suture Removal Location of Sutures Extremities, scalp, and trunk Face Palms, soles, back, and skin over mobile joints Retention sutures Days Before Removal 7–14 3–5 10–14 14–21 understanding of the nature of the injury and any factors complicating suture or staple removal. • Assess patient allergies, especially to adhesive tape and povidone-iodine, chlorhexidine, or other topical solutions or medications. Rationale: Further tissue damage can be prevented. • After determining when sutures or staples were placed, observe the wound for signs of gaping, drainage, inflammation, infection, or embedded sutures. Rationale: Findings may delay suture or staple removal. Procedure 1157 Patient Preparation • Ensure that the patient and family understand preprocedural teachings. Answer questions as they arise, and reinforce information as needed. Rationale: Understanding of previously taught information is evaluated and reinforced. • Verify that the patient is the correct patient using two identifiers. Rationale: Before performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention. • Administer pain medication as prescribed. Rationale: Pain medication promotes patient comfort and reduces activity during suture or staple removal to provide a stable field. • Provide privacy and position the patient for comfort without undue tension on the suture line or staples. Rationale: Provides patient comfort and promotes cooperation during procedure. • Adjust the light to shine directly on the suture line or staples. Rationale: Light is used to facilitate visibility. for Suture Removal Steps 1. Check order to confirm exact timing and other relevant information. 2. HH 3. PE 4. Apply sterile drapes or towels over or under the area as needed. 5. Gently tug on the sutures to test the wound line before removal, to be sure the wound does not separate. If any doubt exists to the integrity of the suture line, apply a skin adherent and adhesive skin strips between sutures before removing them. Remove alternate sutures initially, until integrity of the incision is ensured; then remove the remaining sutures.5 (Level E*) 6. Clean the suture line with antiseptic skin cleanser. The wound is considered clean, so when cleaning it, wipe from clean to dirty, moving from the inner aspect to the outer margins of the wound. Rationale Special Considerations Ensures appropriate treatment. Prescribing physician, advanced practice nurse, or other healthcare professional may want to leave some sutures in place for an additional day or two to support the suture line. Provides protective barrier. Ensures that the wound is healed sufficiently before removal of all sutures. If the patient has both retention and regular sutures in place, retention sutures may remain in place for 14–21 days. Decreases the number of microorganisms and reduces the risk for infection. Be particularly careful to clean the suture line before removing mattress sutures, especially if the visible, contaminated part of the stitch is too small to cut twice for sterile removal. Carefully remove encrusted drainage to allow visualization of all sutures to be removed. *Level E: Multiple case reports, theory-based evidence from expert opinions, or peer-reviewed professional organizational standards without clinical studies to support recommendations. Procedure continues on following page 1158 Unit VII Procedure Integumentary System for Suture Removal—Continued Steps Rationale Special Considerations 7. Use sterile techniques to remove running sutures (Fig. 130-1)2: A. Use sterile forceps to grasp the knot and gently raise it off of the skin. B. Use the rounded tip of the sterile suture scissors to cut the suture at the skin edge on one side of the visible part of the suture. C. Remove the suture by lifting the visible end of the skin to avoid drawing the contaminated portion through subcutaneous tissue. 8. To remove mattress sutures (Fig. 130-2)6: A. Remove the small visible portion of the suture opposite the knot by cutting it at each visible end and lifting the small piece away from the skin. B. Remove the rest of the suture by pulling it out in the direction of the knot. C. If the visible portion is too small to cut twice, cut once and pull the entire suture out in the opposite direction. 9. If the wound dehisces, apply butterfly adhesive strips or paper tape to support and approximate the edges and call the physician or physician extender. 10. Wipe the incision line gently with gauze soaked in antiseptic skin cleanser or prepackaged swab.2 (Level E*) 11. Apply adhesive skin strips or paper tape and a light, sterile gauze dressing, if desired. Leave strips in place for 3–5 days or as ordered. 12. Dispose of gloves and equipment in appropriate receptacles. 13. HH Visible part of suture is exposed to skin bacteria and is considered contaminated. For running sutures, each individual section needs to be cut to prevent the contaminated suture material from being pulled through the subcutaneous tissue. Prevents pulling it through and contaminating subcutaneous tissue.6 Adhesive strips may be used to reapproximate the wound edges until complete wound closure occurs. Removes serous or bloody drainage from the suture line. Wound dehiscence is the premature opening of a wound along a suture line.6 Holds incision edges together, decreases transmission of microorganisms, and decreases irritation from clothing. *Level E: Multiple case reports, theory-based evidence from expert opinions, or peer-reviewed professional organizational standards without clinical studies to support recommendations. Figure 130-1 Removal of plain interrupted sutures with sterile forceps and scissors. Figure 130-2 Removal of interrupted mattress sutures with sterile forceps and scissors. 130 Procedure Suture and Staple Removal 1159 for Staple Removal Steps 1. Check order to confirm exact timing and other relevant information. 2. HH 3. PE 4. Apply sterile drapes or towels over or under the area as needed. 5. Gently test the wound line before removal of the staple to be sure the wound does not separate. If any doubt exists, apply a skin adherent and adhesive skin strips between staples before removing them. Remove alternate staples initially, until integrity of the incision is ensured, then remove the remaining staples.5 (Level E*) 6. Clean the staple line with antiseptic skin cleanser. The wound is considered clean, so when cleaning it, wipe from clean to dirty, moving from the inner aspect to the outer margins of the wound. 7. Use sterile techniques to remove staples (Fig. 130-3). A. Gently place the tip of the staple remover under the staple at its center. B. If the incision line is under tension, gently squeeze the opposite sides together with your free hand as each staple is removed. C. Compress the staple remover until the staple bends in the center and the edges lift out of the skin. D. Discard the staple and proceed to the next staple. 8. If the wound dehisces, apply butterfly adhesive strips or paper tape to support and approximate the edges and call the prescribing physician, advanced practice nurse, or other healthcare professional. Rationale Special Considerations Ensures appropriate treatment. Prescribing physician, advanced practice nurse, or other healthcare professional may want to leave some staples in place for an additional day or two to support the staple line. Provides protective barrier. Ensures that wound is healed sufficiently before removal of all staples. Decreases the number of microorganisms and reduces the risk for infection. Carefully remove encrusted drainage to allow visualization of all staples to be removed. Provides approximation of wound edges until the physician, advanced practice nurse, or other healthcare professional reassesses the wound. Monitor wound dehiscence for sign of infection. **Level E: Multiple case reports, theory-based evidence from expert opinions, or peer-reviewed professional organizational standards without clinical studies to support recommendations. Procedure continues on following page Figure 130-3 Staple removal. 1160 Unit VII Procedure Integumentary System for Staple Removal—Continued Steps Rationale Special Considerations 9. Wipe the incision line gently with the gauze soaked in antiseptic skin cleanser or prepackaged swab. 10. Apply adhesive skin strips or paper tape and a light, sterile gauze dressing, if desired. Leave strips in place for 3–5 days or as ordered. 11. Dispose of gloves and equipment in appropriate receptacle. 12. HH Removes serous or bloody drainage from the staple line. Holds incision edges together, decreases transmission of microorganisms, and decreases irritation from clothing. Expected Outcomes Unexpected Outcomes • Wound remains infection free • Function is preserved • Appearance is restored • • • • Wound infection and possible sepsis Loss of function Abnormal appearance Wound dehiscence Patient Monitoring and Care Steps Rationale Reportable Conditions 1. Retest range of motion and sensory perception after suture or staple removal. 2. Observe for wound discharge or other abnormal changes. Ensures no further damage was imposed. 3. Provide detailed patient and family education, including wound care, medications, signs and symptoms of infection, when the patient can get the incision wet, and follow-up instructions. 4. Follow institutional standards for assessing pain. Administer analgesia as prescribed. Facilitates patient and family cooperation. Allows for early treatment and prevents systemic infection. Identifies need for pain interventions. These conditions should be reported if they persist despite nursing interventions. • Altered range of motion • Change in sensation, paresthesia, tingling • Wound that is red, swollen, tender, or warm • Wound that begins to drain or fester • Red streaks around the wound • Tender lumps in the groin or under the arm • Chills or fever • Redness that surrounds the incision and does not gradually disappear or shows only a thin line after a few weeks2 • Continued pain despite pain interventions Documentation Documentation should include the following: • Patient and family education and aftercare instructions • Date and time sutures were placed, and date and time sutures were removed • Care of the wound after suture removal • Location and appearance of wound • Range of motion and sensory perception • Pain assessment, interventions, and effectiveness 130 Suture and Staple Removal References and Additional Readings For a complete list of references and additional readings for this procedure, scan this QR code with any freely available smartphone code reader app, or visit http://booksite.elsevier.com/9780323376624. 1161