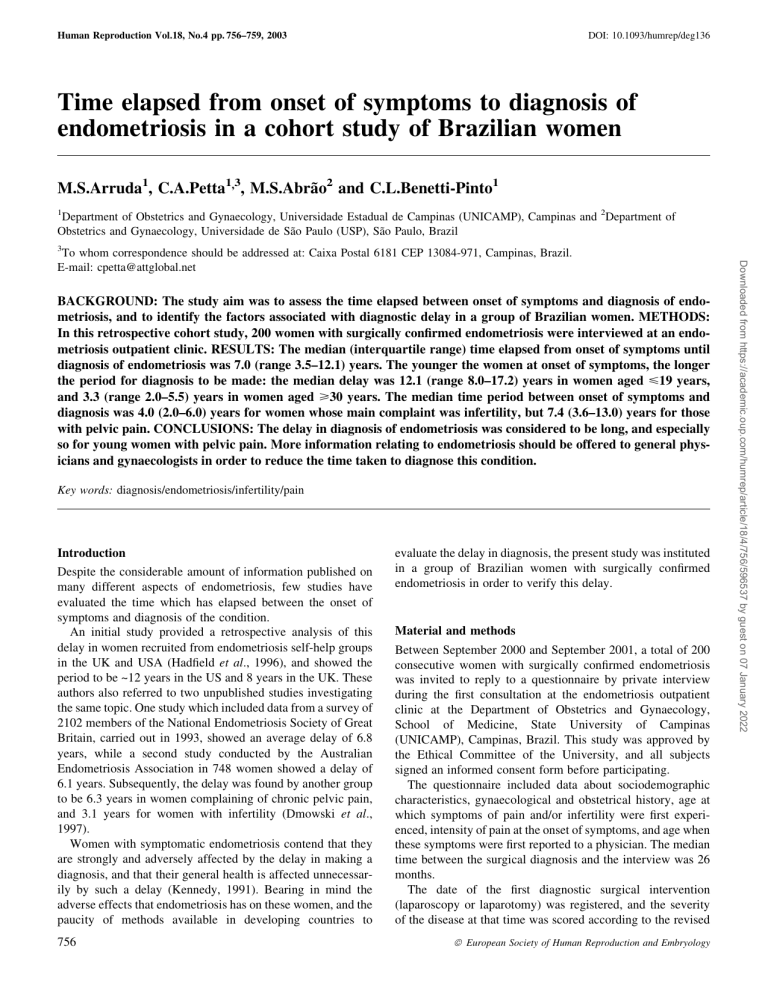
Human Reproduction Vol.18, No.4 pp. 756±759, 2003 DOI: 10.1093/humrep/deg136 Time elapsed from onset of symptoms to diagnosis of endometriosis in a cohort study of Brazilian women M.S.Arruda1, C.A.Petta1,3, M.S.AbraÄo2 and C.L.Benetti-Pinto1 1 Department of Obstetrics and Gynaecology, Universidade Estadual de Campinas (UNICAMP), Campinas and 2Department of Obstetrics and Gynaecology, Universidade de SaÄo Paulo (USP), SaÄo Paulo, Brazil 3 BACKGROUND: The study aim was to assess the time elapsed between onset of symptoms and diagnosis of endometriosis, and to identify the factors associated with diagnostic delay in a group of Brazilian women. METHODS: In this retrospective cohort study, 200 women with surgically con®rmed endometriosis were interviewed at an endometriosis outpatient clinic. RESULTS: The median (interquartile range) time elapsed from onset of symptoms until diagnosis of endometriosis was 7.0 (range 3.5±12.1) years. The younger the women at onset of symptoms, the longer the period for diagnosis to be made: the median delay was 12.1 (range 8.0±17.2) years in women aged <19 years, and 3.3 (range 2.0±5.5) years in women aged >30 years. The median time period between onset of symptoms and diagnosis was 4.0 (2.0±6.0) years for women whose main complaint was infertility, but 7.4 (3.6±13.0) years for those with pelvic pain. CONCLUSIONS: The delay in diagnosis of endometriosis was considered to be long, and especially so for young women with pelvic pain. More information relating to endometriosis should be offered to general physicians and gynaecologists in order to reduce the time taken to diagnose this condition. Key words: diagnosis/endometriosis/infertility/pain Introduction Despite the considerable amount of information published on many different aspects of endometriosis, few studies have evaluated the time which has elapsed between the onset of symptoms and diagnosis of the condition. An initial study provided a retrospective analysis of this delay in women recruited from endometriosis self-help groups in the UK and USA (Had®eld et al., 1996), and showed the period to be ~12 years in the US and 8 years in the UK. These authors also referred to two unpublished studies investigating the same topic. One study which included data from a survey of 2102 members of the National Endometriosis Society of Great Britain, carried out in 1993, showed an average delay of 6.8 years, while a second study conducted by the Australian Endometriosis Association in 748 women showed a delay of 6.1 years. Subsequently, the delay was found by another group to be 6.3 years in women complaining of chronic pelvic pain, and 3.1 years for women with infertility (Dmowski et al., 1997). Women with symptomatic endometriosis contend that they are strongly and adversely affected by the delay in making a diagnosis, and that their general health is affected unnecessarily by such a delay (Kennedy, 1991). Bearing in mind the adverse effects that endometriosis has on these women, and the paucity of methods available in developing countries to 756 evaluate the delay in diagnosis, the present study was instituted in a group of Brazilian women with surgically con®rmed endometriosis in order to verify this delay. Material and methods Between September 2000 and September 2001, a total of 200 consecutive women with surgically con®rmed endometriosis was invited to reply to a questionnaire by private interview during the ®rst consultation at the endometriosis outpatient clinic at the Department of Obstetrics and Gynaecology, School of Medicine, State University of Campinas (UNICAMP), Campinas, Brazil. This study was approved by the Ethical Committee of the University, and all subjects signed an informed consent form before participating. The questionnaire included data about sociodemographic characteristics, gynaecological and obstetrical history, age at which symptoms of pain and/or infertility were ®rst experienced, intensity of pain at the onset of symptoms, and age when these symptoms were ®rst reported to a physician. The median time between the surgical diagnosis and the interview was 26 months. The date of the ®rst diagnostic surgical intervention (laparoscopy or laparotomy) was registered, and the severity of the disease at that time was scored according to the revised ã European Society of Human Reproduction and Embryology Downloaded from https://academic.oup.com/humrep/article/18/4/756/596537 by guest on 07 January 2022 To whom correspondence should be addressed at: Caixa Postal 6181 CEP 13084-971, Campinas, Brazil. E-mail: cpetta@attglobal.net Diagnostic delay in women with endometriosis Statistical analysis The median and the interquartile range were used to describe the sample. Because of the asymmetric distribution of the variables (time from onset of symptoms to the ®rst appointment; time from the ®rst appointment to a diagnosis; and total time from onset of symptoms to a diagnosis of endometriosis) and the presence of atypical values (outliers), the nonparametric Wilcoxon test was used to evaluate the association between dependent and independent variables. The level of signi®cance was set at P < 0.05. Although the infertility group was small (n = 20) compared with the chronic pelvic pain group (n = 180), after performing a power analysis (a = 5%; b = 80%), the sample size was considered appropriate (P = 0.01) for use of the non-parametric test (Noether, 1987). Results At the time of the interview, 100 (50%) women were aged between 30 and 39 years, 41 (20.5%) were aged >40 years, and only ®ve (2.5%) were aged <20 years. Half of the women were nulligravida, 73% were white, and 62% had more than 8 years of formal school education. Dysmenorrhoea was the main complaint for 134 women (67%), chronic pelvic pain for 35 (12.5%), and dyspareunia for 11 (5.5%). Twenty patients (10%) reported infertility as the main complaint. A total of 177 women (88.5%) experienced more than one symptom, and 126 women (70%) who suffered from pelvic pain classi®ed their symptoms as severe. The overall median time from the onset of symptoms to a diagnosis of endometriosis was 7.0 years, with an interquartile range of 3.5 to 12.1 years. The median age at the time of onset of symptoms was 20.5 years for those women whose main complaint was pelvic pain, Table I. Median (interquartile range) age at onset of symptoms, at reporting symptoms to a doctor, and at diagnosis in women presenting for pelvic pain and infertility Age at onset of symptoms (years) Age at reporting symptoms (years) Age at diagnosis (years) Median delay from onset of symptoms to diagnosis (years) aWilcoxon Pelvic pain (n = 180) Infertility (n = 20) 20.5 (14.0±27.5) 23.0 (17.0±30.0) 33.0 (29.0±39.0) 7.4a 23.5 (20.0±25.5) 25.5 (22.5±28.0) 30.0 (29.0±32.0) 4.0a test, P < 0.01. Table II. Median time (years) elapsed from the ®rst symptoms to seeing a doctor and to the surgical diagnosis according to age at onset of symptoms Age at onset of Time from ®rst Time from seeing a Total time elapsed symptoms (years) symptoms to doctor to surgical from ®rst symptoms seeing a doctor diagnosis to diagnosis <19 20±29 >30 Pa aWilcoxon 2.0 0.5 0.2 < 0.01 9.0 4.0 3.0 < 0.01 12.1 4.5 3.3 < 0.01 test. Table III. Median (interquartile range) time (years) elapsed from ®rst symptoms to seeing a doctor and to the diagnosis, according to the main symptom Main complaint n From ®rst symptoms to seeing a doctor From seeing a doctor to diagnosis From ®rst symptoms to diagnosis Chronic pelvic pain Dysmenorrhoea Dyspareunia Infertility Total 35 134 11 20 200 0.3 0.6 1.0 1.7 0.9 4.0 6.5 4.0 2.0 5.0 4.2 8.4 5.0 4.0 7.0 (0.2±1.0) (0.3±3.0) (0.2±3.0) (1.0±2.0) (0.2±2.0) (2.0±6.0) (3.0±11.0) (1.0±11.0) (0.7±3.5) (2.0±9.5) (2.2±6.3) (5.0±14.0) (2.2±15.2) (2.1±6.0) (3.5±12.1) and 23.5 years for those with infertility complaints. The median age at diagnosis was 33.0 years for the group with pelvic pain, and 30.0 years for those who were infertile (Table I). The median time elapsed between onset of symptoms and diagnosis was shorter for women complaining of infertility [4.0 (range 2.0±6.0) years] than in those with pelvic pain [7.4 (range 3.6±13.0) years] (P < 0.01). In terms of seeking help, the infertility group took a median of 1.7 (1.0±2.0) years, which was signi®cantly longer than women with pelvic pain, who took 0.5 (range 0.2±2.0) years. Younger women took a signi®cantly longer time to report their symptoms to a doctor, and also had to wait for longer until a de®nitive diagnosis was made (Table II). The time interval from the ®rst symptoms to a diagnosis was not signi®cantly different in the four stages of the disease, namely 7.0, 6.8, 7.4 and 6.7 years for stages I, II, III and IV respectively. The delay from onset of symptoms to a ®rst consultation, from the ®rst consultation to a diagnosis of endometriosis, and the total time from onset of symptoms to diagnosis according to the main complaint are detailed in Table III. No relationship 757 Downloaded from https://academic.oup.com/humrep/article/18/4/756/596537 by guest on 07 January 2022 American Society for Reproductive Medicine classi®cation (American Society for Reproductive Medicine, 1997). These data were obtained from the women's medical records or surgical reports and/or video tapes of surgery sent by the referring physician. Women with more than one symptom were asked to point out the main reason why they decided to seek help. Whenever pain was the main complaint, whether chronic pelvic pain (pain unrelated to menses and lasting for at least 6 months), dysmenorrhoea or dyspareunia, women were asked to classify their pain (at the time of the initial report) as either: (i) mild, if there was mild interference with normal activities and usually no medication was required; (ii) moderate, if there was noticeable interference with normal daily activities and analgesics were usually required; or (iii) severe, if the patient was unable to function normally or had to visit emergency units for pain relief. In order to obtain more precise data, attempts were made to improve the patients' recall of the timing of the onset of symptoms and the time they initially reported their symptoms to a physician. They were asked about their age at menarche, when they were married or became pregnant, the date they delivered their children, their school and job activities, and their use of analgesics or visits to emergencies rooms. M.S.Arruda et al. Discussion The overall median time of 7.0 years from onset of symptoms to a diagnosis of endometriosis observed in the present study was similar to that reported by both The National Endometriosis Society of Great Britain and the Australian Endometriosis Association (Had®eld et al., 1996), and was also in agreement with these authors' own ®ndings, which indicated a mean delay in diagnosis of 11.7 and 7.9 years for women in the USA and UK respectively. The delay in diagnosis in infertile patients was shorter than that in patients with pelvic pain, and was similar to that reported elsewhere (Dmowski et al., 1997). This is most likely a consequence of a better established protocol to investigate infertile women, which includes diagnostic laparoscopy. The age at onset of symptoms was inversely associated with the delay in diagnosing endometriosis. Although 88 (44%) of the present patients initially reported their symptoms to their physicians before the age of 20, only seven (3.5%) were diagnosed with endometriosis before that age. Unfamiliarity with menstrual cramps during the ®rst years after menarche, and the widespread notion that menstrual periods are painful, are two possible reasons why these women took longer to seek help. However, it is dif®cult to understand why the median period from initial consultation to a diagnosis was 9.0 years when symptoms started during adolescence, but only 3.0 years when they started at the age of 30 years or more. Physicians might consider painful menstruation a physiological condition, even when severe, subsiding with analgesics or oral contraceptives. It is also possible that adolescents might be less convincing and persuasive than older women when reporting symptoms, and may also feel uncomfortable when reporting the occurrence of pain during intercourse. Among the adolescent patients interviewed, only one patient reported dyspareunia spontaneously as the main complaint, and 49 758 reported it as a secondary complaint. In addition, a physical examination may be more dif®cult in adolescents, especially if they are not sexually active. Although symptoms of pain are reported by almost one-third of all gynaecological patients, and about 50% of menstruating adolescents and young women suffer from painful menstruÈ zaksit et al., 1995), endometriosis should be suspected ation (O in adolescents because it is a common cause of pain and dysmenorrhoea, affecting 45±70% of those with chronic pelvic pain (Propst and Laufer, 1999). One study comparing preoperative pelvic examination and ultrasonographic ®ndings with laparoscopy in 45 adolescents with chronic pelvic pain showed that when both, pelvic examination and ultrasound were normal, 50% of these cases were abnormal at laparoscopy È zaksit et al. 1995). and 20% of them had endometriosis (O Despite many limitations of the Brazilian public health system, the time from an initial complaint to the diagnosis of endometriosis was no longer than is observed in the UK and USA (Had®eld et al., 1996). Although laparoscopy has become a valuable tool in the investigation of pelvic pain, laparotomy was found still to be used as a diagnostic method, especially in public hospitals where laparoscopy is still not widely available. Indeed, the high cost of laparoscopy in private institutions may force women to seek free-of-charge treatment at public hospitals, and this will result in long waiting lists for scheduled appointments at referral centres. In addition, gynaecologists might lack the skill to perform a laparoscopy and would be reluctant to refer their patients to a specialized centre. This is a phenomenon observed in all parts of the world, even in developed countries (Jones et al., 2002). The high prevalence of moderate and severe disease among the interviewed patients was expected because the present investigation was carried out at a tertiary care centre, with referred cases. As the University also has an infertility clinic to which infertile couples are usually referred, few of the present patients listed infertility as their main complaint. For these reasons, the population investigated may not re¯ect the situation of the general population with endometriosis. The overall long delay in the present study to reach a diagnosis of endometriosis corroborates with a previous observation (Kennedy, 1991): ``Women frequently complain that the diagnosis was made only after months and months of being fobbed off or ignored by doctors''. Whether or not this delay is associated with a progression of the disease stages is a controversial issue. Although some publications have attempted to support the concept that endometriosis is a progressive disease (Koninckx et al., 1991; Dmowski et al., 1997), conclusive data are still lacking. Consequently, it is impossible to be sure that an earlier diagnosis would detect endometriosis at a less severe stage of the disease, though the impact of endometriosis on the lives of these women could be minimized. Appropriate medical therapy would reduce absenteeism at school or work and make sexual intercourse more enjoyable for those with pelvic pain, while adequate therapy would be indicated for those with infertility. Downloaded from https://academic.oup.com/humrep/article/18/4/756/596537 by guest on 07 January 2022 between the intensity of pain and the stage of the disease was found, however (data not shown). A comparison was also made as to where the diagnosis was carried out, the percentage of laparoscopic procedures performed, and the delay in diagnosis for each group. Diagnoses were made at the authors' institution (a public university centre) in 106 women (53%), in a private setting in 62 (31%), and in other public hospitals in 32 (16%). The diagnosis performed laparoscopically in 66% of women at the authors' institution, and in 77 and 25% at private institutions and other public hospitals respectively. The median delay from onset of symptoms and diagnosis at the authors' hospital and other public hospitals (6.3 years) was shorter than that at private clinics (9.1 years). No correlation was found between the patients' years of formal school education and the time interval for a diagnosis of endometriosis. Women with <7 years of formal education took a median period of 0.8 years to report symptoms to a doctor, whereas those with >7 years of education took 0.9 years (P = NS). The total delay from onset of symptoms to a surgical diagnosis in these patient groups was 6.2 and 7.2 years respectively (P = NS). Diagnostic delay in women with endometriosis Acknowledgements The authors thank Edson Zangiacomi Martinez and Gislaine Carvasan for their assistance in the data analysis. These results were presented as a poster at the VIII World Congress on Endometriosis, San Diego, CA, United Sates, February 24±27, 2002. References American Society for Reproductive Medicine (1997) Revised American Society for Reproductive Medicine Classi®cation of Endometriosis: 1996. Fertil. Steril., 67, 817±821. Dmowski, W.P., Lesniewicz, R., Rana, N., Pepping, P. and Noursalehi, M. (1997) Changing trends in the diagnosis of endometriosis: a comparative study of women with pelvic endometriosis presenting with chronic pelvic pain or infertility. Fertil. Steril., 67, 238±243. Had®eld, R., Mardon, H., Barlow, D. and Kennedy, S. (1996) Delay in the diagnosis of endometriosis: a survey of women from the USA and the UK. Hum. Reprod., 11, 878±880. Jones, K.D., Fan, A. and Sutton, C.J.G. (2002) The ovarian endometrioma: why it is so poorly managed? Hum. Reprod., 17, 845±849. Kennedy, S.H. (1991) What is important to the patient with endometriosis? Br. J. Clin. Pract. Sump. Suppl., 72, 8±10. Koninckx, P.R., Meuleman, C., Demeyere, S., Lesaffre, E. and Cornillie, F.J. (1991) Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply in®ltrating endometriosis is associated with pelvic pain. Fertil. Steril., 55, 759±765. Noether, G.E. (1987) Sample size determination for common nonparametric tests. J. Am. Statist. Assoc., 39, 823±829. È zaksit, G., Caglar, T., Zorlu, C.G., Cobanoglu, O È ., Cicek, M., Batioglu, S. O and GoÈkmen, O. (1995) Chronic pelvic pain in adolescent women: diagnostic laparoscopy and ultrasonography. J. Reprod. Med., 40, 500±502. Propst, A. and Laufer, M.R. (1999) Endometriosis in adolescents: incidence, diagnosis and treatment. J. Reprod. Med., 44, 751±758. Submitted on January 29, 2002; resubmitted on November 19, 2002; accepted on November 28, 2002 759 Downloaded from https://academic.oup.com/humrep/article/18/4/756/596537 by guest on 07 January 2022 The present study provides evidence of the situation regarding the diagnosis of endometriosis in a less-developed country. There are some methodological limitations to be considered, however: the precise date of the onset of symptoms and the date that these symptoms were reported to a physician were totally dependent on the patients' ability to remember facts that very often occurred a long time ago. Even with the investigators' efforts to improve the patients' recollection of dates and times, this may not be absolutely accurate. In addition, it is dif®cult to assign a precise stage of the disease retrospectively for patients referred to this service, on the basis of surgical records alone. To minimize this limitation, patients who could not have their disease stage assigned were excluded from the study. Despite all of these possible biases, personal interviews might provide more accurate information than self-answered questionnaires sent by mail. Another possible criticism of the present study is the very small number of patients included in the infertility group. Although pain and infertility have different starting points, and also have different in¯uences on any decision to perform laparoscopy, the statistical power of the non-parametric test used enabled comparisons to be made between the two groups. Hence, it was decided to retain this group in order to show the important differences in the delay to a diagnosis of endometriosis in both groups. In conclusion, the present study shows that the delay in diagnosing endometriosis was considerably long, and especially so in young women with pelvic pain and in adolescents. Clearly, more information about endometriosis must be made available to general physicians and gynaecologists in order to reduce the time taken to diagnose this condition.