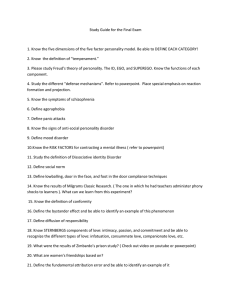
Personality Ingrained, enduring pattern of behaving and relating to the self, others, and environment Includes perceptions, attitudes, emotions These behaviors are consistent across a broad range of situations Personality Disorders Negative behaviors toward others, such as being manipulative, dishonest, deceitful, or lying Anger and/or hostility Irritable, labile moods Lack of guilt or remorse, emotionally cold and uncaring Impulsivity, distractibility, poor judgment Irresponsible, not accountable for own actions Risk-taking, thrill-seeking behaviors Mistrust Exhibitionism Entitlement Dependency, insecurity Eccentric perceptions Personality Disorders Not diagnosed until age 18 Maladaptive behavior patterns can often be traced to early childhood or adolescence Types of Personality Disorders Cluster A—odd or eccentric behaviors o Paranoid personality disorder o Schizoid personality disorder o Schizotypal personality disorder Cluster B—erratic or dramatic behaviors o Antisocial personality disorder o Borderline personality disorder o Histrionic personality disorder o Narcissistic personality disorder Cluster C—anxious or fearful behaviors o Avoidant personality disorder o Dependent personality disorder o Obsessive personality disorder Treatment Based on disorder type and severity Medications Group and individual therapy Schizotypal, narcissistic, or obsessive–compulsive personality disorders are least likely to engage or remain in any treatment Psychopharmacology Four symptom categories that underlie personality disorders o Cognitive–perceptual distortions, including psychotic symptoms o Affective symptoms and mood dysregulation o Aggression and behavioral dysfunction o Anxiety Psychopharmacology Aggression o Lithium, benzodiazepines Mood dysregulation o Lithium, carbamazepine (Tegretol), valproate (Depakote), haloperidol Emotional detachment, cold and aloof emotions and disinterest in social relations o Risperidone (Risperdal), olanzapine (Zyprexa), quetiapine (Seroquel) Individual and Group Psychotherapy Goals o o o o o Building trust Teaching basic living skills Providing support Decreasing distressing symptoms such as anxiety Improving interpersonal relationships Individual and Group Psychotherapy Relaxation and meditation – anxiety Case manager or therapist – basic living skills Assertiveness training groups Cognitive-behavioral therapy o Thought stopping o Positive self-talk o Decatastrophizing Paranoid Personality Disorder Pervasive mistrust and suspiciousness of others May appear aloof and withdrawn Guarded and hypervigilant Mood may be labile, quickly changing from quietly suspicious to angry or hostile Paranoid Personality Disorder Interventions Approach client in a formal, businesslike manner and refrain from social chit-chat or jokes Being on time, keeping commitments, and being especially straightforward are essential to the success of the nurse–client relationship Involve them in formulating their care plan Help clients validate ideas before taking action o Helps prevent clients from acting on paranoid ideas or beliefs Schizoid Personality Disorder Pattern of detachment from social relationships and a restricted range of emotional expression in interpersonal Constricted affect and little, if any, emotion Aloof and indifferent, appearing emotionally cold, uncaring, or unfeeling No leisure or pleasurable activities Rich and extensive fantasy life No disordered or delusional thought processes Schizoid Personality Disorder Indecisive and lack future goals or direction Self-absorbed and loners in almost all aspects of daily life Indifferent to praise or criticism and are relatively unaffected by the emotions or opinions of others Interventions focus on improved functioning in the community o Referrals to social services or local agencies for assistance – housing o Case manager – help obtain services, health care, manage finances Schizotypal Personality Disorder Pattern of social and interpersonal deficits marked by acute discomfort with and reduced capacity for close relationships Cognitive or perceptual distortions and behavioral eccentricities May develop schizophrenia Odd appearance Schizotypal Personality Disorder Wander aimlessly Frequently use words incorrectly, which makes their speech sound bizarre Lack the ability to experience and to express a full range of emotions Anxiety around other people Cannot engage in superficial conversations Schizotypal Personality Disorder Cognitive distortions o Ideas of reference Involve the client’s belief that events have special meaning for him or her o Magical thinking Believes he or she has special powers Schizotypal Personality Disorder Interventions Encourage the client to establish a daily routine for hygiene and grooming Role-play interactions with the client Social skills training o Helps clients talk clearly to others and reduce bizarre conversations Antisocial Personality Disorder Pattern of disregard for and violation of the rights of others o Usually involves deceit and manipulation History o Childhood enuresis, sleepwalking, and acts of cruelty are characteristic predictors o Adolescence - lying, truancy, sexual promiscuity, cigarette smoking, substance use, and illegal activities Antisocial Personality Disorder Appearance is usually normal Views of the world are narrow and distorted Oriented, no sensory-perception alterations, average to above average IQ Poor judgement Appear confident, self-assured, and accomplished Manipulate and exploit those around them Do not seek treatment voluntarily unless they perceive some personal gain from doing so Antisocial Personality Disorder Interventions Limit setting is an effective technique that involves three steps: o Stating the behavioral limit (describing the unacceptable behavior) o Identifying the consequences if the limit is exceeded o Identifying the expected or desired behavior Example of Limit Setting Client may approach the nurse flirtatiously and attempt to gain personal information: “It is not acceptable for you to ask personal questions. If you continue, I will terminate our interaction. We need to use this time to work on solving your job-related problems.” Antisocial Personality Disorder Interventions Confrontation o Technique designed to manage manipulative or deceptive behavior o Point out a client’s problematic behavior o Remain neutral and matter-of-fact o Avoid accusing the client Confrontation Example Nurse: “You’ve said you’re interested in learning to manage angry outbursts, but you’ve missed the last three group meetings.” Client: “Well, I can tell no one in the group likes me. Why should I bother?” Nurse: “The group meetings are designed to help you and the others, but you can’t work on issues if you’re not there.” Antisocial Personality Disorder Interventions Teach problem-solving skills Assist in managing emotions o Encourage them to identify sources of frustration, how they respond to it, and the consequences Encourage the client to take a time-out Antisocial Personality Disorder Interventions Help the client to identify specific problems at work or home that are barriers to success in fulfilling roles Assess the use of drugs and alcohol Borderline Personality Disorder Pervasive pattern of unstable interpersonal relationships, self-image, and affect as well as marked impulsivity (x3 more common in women) History o Many report disturbed early relationships with their parents that often begin at 18 to 30 months of age o Childhood sexual abuse, physical or verbal abuse, parental alcoholism o Tend to use transitional objects Borderline Personality Mood is dysphoric o Unhappiness o Restlessness o Malaise o Loneliness o Boredom o Frustration o Feeling empty Mood is unstable and erratic Minor changes precipitate emotional crisis Borderline Personality Splitting o Thinking about oneself and others is polarized and extreme Excessive and chronic fear of abandonment Fully oriented; intellectual capacity intact Impaired judgement and lack of care and concern for safety Suicidal threats, gestures, attempts are common Self-mutilation is common Borderline Personality Feelings for others are often distorted, erratic, and inappropriate History of poor work and school performance May engage in binging and purging, substance abuse, unprotected sex, or reckless behavior such as driving while intoxicated Borderline Personality Interventions Safety is a priority No self-harm contract o Client promises not to engage in self-harm and to report to the nurse when he or she is losing control Explore the self-harm behavior o Identify trigger situations, moods, or emotions that precede self-harm and to use more effective coping skills to deal with the trigger issues Borderline Personality Interventions Help establish boundaries Client: “You’re better than my family and the doctors. You understand me more than anyone else.” Nurse: “I’m interested in helping you get better just as the other staff members are.” (establishing boundaries) Borderline Personality Interventions Cognitive restructuring o Help clients recognize negative thoughts and feelings and replacing them with positive patterns of thinking Thought stopping o Technique to alter the process of negative or self-critical thought patterns Positive self-talk o Client reframes negative thoughts into positive ones Borderline Personality Interventions Decatastrophizing o Technique that involves learning to assess situations realistically rather than always assuming a catastrophe will happen “So what is the worst thing that could happen?” or “How likely do you think that is?” Borderline Personality Interventions Structuring the client’s daily activities o At a loss about how to manage unstructured time and may engage in desperate behaviors o Planning activities can help clients manage time alone Written schedule Histrionic Personality Disorder Pervasive pattern of excessive emotionality and attention seeking Speech is colorful and theatrical Overall appearance is normal (may overdress) Overly concerned with impressing others with their appearance Histrionic Personality Disorder Exaggerate emotions inappropriately Rapid shifts in mood Like to be center of attention Exaggerate intimacy of relationships Histrionic Personality Disorder Interventions Give clients feedback about their social interactions with others, including manner of dress and nonverbal behavior Example: o “When you embrace and kiss other people on first meeting them, they may interpret your behavior in a sexual manner. It would be more acceptable to stand at least 2 ft away from them and to shake hands.” Histrionic Personality Disorder Interventions Teach and role-play social skills Be specific and model social skills o Eye contact, engage in active listening, respecting personal space Narcissistic Personality Disorder Characterized by a pervasive pattern of grandiosity, need for admiration, and lack of empathy Arrogant or haughty attitude Lack ability to recognize or empathize with the feelings of others Narcissistic Personality Disorder May express envy and begrudge others any recognition or material success Preoccupied with fantasies of unlimited success, power, brilliance, beauty, or ideal love Underlying self-esteem is fragile and vulnerable Hypersensitive to criticism Sense of entitlement Trouble working with others Narcissistic Personality Disorder Interventions Use self-awareness skills to avoid anger and frustration with these clients Teach about comorbid medical or psychiatric conditions, medication regimen, and any needed self-care skills in a matter-of-fact manner Set limits Individual psychotherapy is most effective treatment Avoidant Personality Disorder Pervasive pattern of social discomfort, low self-esteem, and hypersensitivity to negative evaluation May be anxious, fidget, and make poor eye contact Shy, fearful, socially awkward, and easily devastated by real or perceived criticism Low self-esteem Avoidant Personality Disorder Reluctant to do anything perceived as risky Strongly desire social acceptance and human companionship o Fear rejection and humiliation Avoidant Personality Disorder Interventions Help clients practice self-affirmation and positive self-talk Reframing Decatastrophizing Teach social skills Dependent Personality Disorder Characterized by a pervasive and excessive need to be taken care of, which leads to submissive and clinging behavior and fears of separation Runs in families Most common in the youngest child Dependent Personality Disorder Anxious; pessimistic, self-critical Others hurt their feelings easily Preoccupied with unrealistic fears of being left alone to care for themselves Keeping and finding a relationship occupies much of their time Difficulty making decisions “Any relationship is better than no relationship at all.” Dependent Personality Disorder Interventions Help clients express feelings of grief and loss over the end of a relationship while fostering autonomy and self-reliance Help clients identify their strengths and needs May need assistance in daily functioning Teach problem-solving and decision-making Obsessive-Compulsive Personality Disorder Preoccupation with perfectionism, mental and interpersonal control, and orderliness at the expense of flexibility, openness, and efficiency Demeanor is formal and serious Answer questions with precision and much detail A need to be perfect beginning in childhood Obsessive-Compulsive Personality Disorder Difficulty expressing emotions Affect is restricted; appear anxious and fretful or stiff and reluctant Preoccupied with orderliness Problems with judgement and decision-making Low self-esteem; harsh, critical, judgmental of self Difficulty in relationships Obsessive-Compulsive Personality Disorder Interventions Help clients view decision-making and completion of projects from a different perspective Cognitive restructuring techniques o “What is the worst that could happen?” or “How might your boss (or your wife) see this situation?” Encourage the client to take risks Community-Based Care Care for clients with personality disorders occurs primarily in the community-based settings Acute psychiatric settings – if there are safety concerns for short periods Points to Consider When Working with Clients with Personality Disorders Talking to colleagues about feelings of frustration will help you deal with your emotional responses so you can be more effective with clients Clear, frequent communication with other health care providers can help diminish the client’s manipulation Do not take undue flattery or harsh criticism personally; it is a result of the client’s personality disorder Set realistic goals, and remember that behavior changes in clients with personality disorders take a long time. Progress can be slow.