Uploaded by
basheer.nassrallah
Reduced Consciousness in Children: Clinical Biochemistry Guidelines
advertisement

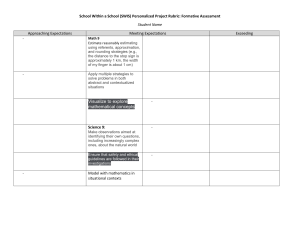
Review Article Guidelines for the investigation and management of a reduced level of consciousness in children: implications for clinical biochemistry laboratories R Bowker1, A Green2 and J R Bonham3 Abstract Addresses 1 Academic Department of Child Health, Queen’s Medical Centre, Nottingham; 2 Department of Clinical Chemistry, Birmingham Children’s Hospital, Birmingham; 3 Department of Clinical Chemistry, Sheffield Children’s (NHS) Foundation Trust, Sheffield S10 2TH, UK Correspondence Dr J R Bonham Email: jim.bonham@sch.nhs.uk This article was prepared at the invitation of the Clinical Sciences Reviews Committee of the Association for Clinical Biochemistry Whenever a child presents to hospital with a reduced level of consciousness, admitting clinicians have to decide the underlying cause rapidly so that the correct emergency treatment can be initiated. Unfortunately, the clinical presentations of many of the possible diagnoses are very similar. The diagnosis often results from investigations within the clinical biochemistry laboratory. In the past, clinicians have had limited guidance on which tests to request when presented with a child with a reduced level of consciousness. Guidelines have recently been developed relating to all aspects of management of the child in a coma. Due to a lack of evidence in the literature regarding the most appropriate first line tests for children with a reduced level of consciousness, a formal consensus process (‘Delphi consensus’) was performed using a large multidisciplinary panel of experts. The recommendations reached by this process include the list of initial (‘core’) tests to request for all children with a reduced level of consciousness (excluding those immediately after suffering a convulsion and those involved in obvious trauma). Depending upon the results of these ‘core’ tests and the clinical condition of the child, further tests may be requested later. The key point is that all the samples have been taken at the time of presentation to provide the best chance of reaching a diagnosis and correctly treating the child. The article reviews the recommended core investigations and further tests and discusses how individual laboratories can help to implement the guidelines jointly with their Emergency and Paediatric Departments. Ann Clin Biochem 2007; 44: 506–511 Introduction One of the greatest clinical challenges a paediatrician or emergency physician faces is how to manage a child who presents with an acute reduced level of consciousness, re£ected in a score of less than 15 on the modi¢ed Glasgow coma score (GCSo15), or is only responsive to voice, pain, or is unresponsive on the Alert,Voice, Pain, Unresponsive (AVPU) scale, which scores the consciousness of patients as alert, responding to voice, responding to pain or being unresponsive. About 30 children in every 100,000 per year present to hospital with a reduced level of consciousness not due to trauma (‘non-traumatic coma’).1 In this group, there is a 40% mortality rate.1 The list of possible causes of non-traumatic coma is very long but the most common are infection, drug intoxication, seizures and inherited metabolic diseases. 506 Most of the conditions which cause a reduced level of consciousness in children are clinically very di⁄cult to di¡erentiate from one another, as the symptoms and signs overlap. Clinicians therefore rely heavily on laboratory information to reduce the di¡erential diagnosis list and focus appropriate treatment strategies. Up until now there has been no expert advice on which tests to request when a child presents with a reduced conscious level. For example, the chance of diagnosing the cause of a rare encephalopathy has been largely dependent on the experience of the reviewing doctor and the liaison and input from the laboratory. Rare metabolic conditions by their very nature are not encountered frequently by paediatricians or emergency department sta¡. These conditions may not even enter the di¡erential diagnosis list, when investigations are being considered. There is anecdotal evidence that delays in diagnosing rare causes of a reduced level of r 2007 The Association for Clinical Biochemistry Reduced level of consciousness in children consciousness are commonplace. Such delays in diagnosis can have devastating consequences for the child. Providing advice on the initial investigations to perform in children with a reduced level of consciousness should reduce the diagnostic delays and for the children with rare metabolic conditions improve their outcome. An evidence-based guideline has now been developed for UK practice.2 Where evidence was not available a formal consensus process was used to help form the recommendations. These recommendations include: the initial screening panel of tests which should be performed on all children with a reduced conscious level -- the ‘core investigations’; the investigations to request if hyperammonaemia is detected; the investigations to request if hypoglycaemia is detected; the investigations to request if ketoacidosis without hyperglycaemia is detected; the investigations to request if no cause is detected after reviewing the core investigations. This review will summarize the main recommendations from the guidelines and speci¢cally focuses on how the clinical biochemist and paediatrician can work together to rapidly diagnose the treatable encephalopathies. Core investigations Once the decision has been made to investigate a child for a reduced level of consciousness, the clinician faces two challenges: (1) obtaining blood and urine and possibly cerebrospinal £uid or other samples from a sick child; (2) prioritizing the tests to ensure the treatable causes are detected promptly. A large multi-professional UK panel involved in diagnosing and treating children with encephalopathies have drawn up a list of core investigations2 which balance the need to capture all the major treatable causes, without requiring an excessive amount of blood. The core investigations are listed in Figure 1 as they appear in the guideline. Due to di¡erences in laboratory practice across the National Health Service (NHS), clinicians will need local guidance from their clinical chemistry department as to which bottles and what volumes are required to perform these tests. The laboratory should provide speci¢c details. All children Perform the following in all children with reduced conscious level except those post trauma and those within 1 h post convulsion (see pages 4 and 5) 507 Capillary Glucose Blood gas (capillary, venous, arterial) Urinalysis (dipstick at bedside) Laboratory glucose (even if capillary glucose normal) Urea and electrolytes (Na, K, Cr) Liver function tests Plasma ammonia Full blood count Blood culture 1−2 ml plasma to be separated, 1−2 ml plain serum frozen and saved 10 ml urine to be frozen and saved Figure 1 The core investigations for children with a reduced level of consciousness Hyperammonaemia Analytical aspects One test which requires special mention is plasma ammonia. All hospitals with neonatal units, paediatric wards and emergency admissions for children should provide a robust and reliable service for measuring blood/plasma ammonia 24 h a day, seven days a week.3 Laboratory sta¡ must be aware of the artifactual reasons for a falsely high ammonia concentration (see Sampling errors below). The majority of laboratories in the UK employ automated enzyme-based (glutamate dehydrogenase) methods or dry slide chemistry for the measurement of plasma ammonia. Re£ectance meters employing dry chemistry strips for whole blood ammonia analysis can be used for the initial assessment of patients with suspected hyperammonaemia; however, the working range of some of the older meters is limited and they are therefore not suitable for the monitoring of hyperammonaemia when patients are being treated. Elevated results obtained by meters must be con¢rmed by an alternative laboratory method.4 The laboratory has a responsibility to make the clinician aware of this limitation. Use of such meters as point-of-care testing devices on clinical units such as the emergency department are discouraged as they are prone to misuse unless sta¡ are regularly trained and quality control procedures are in place. Despite these concerns, the results of a national audit recently conducted by MetBioNet, a UK-based stakeholder alliance of 17 laboratories specializing in the investigation and diagnosis of inherited metabolic disorders, indicate that these meters remain in widespread use (19 of 100 respondents) and this is a potential cause for concern unless their operation is carefully regulated. A raised ammonia concentration can be the ¢rst suggestion that the patient has a metabolic encephalopathy. Several studies have shown that a better clinical Ann Clin Biochem 2007; 44: 506–511 508 Bowker et al. outcome is observed when the patient is exposed to hyperammonaemia for as short a period as possible.5,6 The cut-o¡ for requiring active treatment for a raised plasma ammonia is not clear cut,7 but most clinicians would start treatment when the ammonia is greater than 200 mmol/L.2 rated. It is important to warn clinicians about interpreting high ammonia concentrations if the sample had not been free £owing when it was taken, before initiating treatments and all elevated ammonia results should be con¢rmed with a second specimen before starting treatment. Sampling errors Causes of a raised ammonia Erroneously high ammonia concentrations can occur when the blood sample has been di⁄cult to take or has been left to stand as whole blood at room temperature for more than 15 min before the plasma has been sepa- A raised ammonia may be caused by a number of di¡erent conditions, listed in Table 1. Further specialist tests will be required to diagnose the underlying cause of the hyperammonaemia. From the sample collected with Table 1 Causes of pathologically raised plasma ammonia Causes of hyperammonaemia Relative NH3 concentration Initial investigations Inherited metabolic disorders Defects of the urea cycle N-acetylglutamate synthetase deficiency Carbamyl phosphate synthetase deficiency Ornithine transcarbamylase deficiency Arginosuccinate synthetase deficiency Arginosuccinate lyase deficiency Arginase deficiency þ þ þ þ þ þþ Urine orotic acid Enzyme assay in liver or Plasma and urinary skin biopsy tissue amino acids and urinary depending upon the disorder organic acids DNA analysis in some cases þ þþ þþþ þþ Urinary organic acids and amino acids Blood acyl carnitine profile Enzyme assay. DNA analysis in some cases Plasma free carnitine and acylcarnitine profile Urinary organic and amino acids Skin fibroblast flux assays Specific enzyme assay DNA analysis in some cases Organic acidurias Propionic acidaemia Methylmalonic acidaemia Isovaleric acidaemia 3-Hydroxy-3-methylglutaryl coenzyme A (CoA) lyase deficiency Multiple carboxylase deficiency Disorders of fatty acid oxidation Multiple acyl CoA dehydrogenase deficiency Very long chain acyl CoA dehydrogenase deficiency Long chain hydroxyacyl CoA dehydrogenase deficiency Medium chain acyl CoA dehydrogenase deficiency Carnitine acyl carnitine translocase deficiency Carnitine transporter deficiency Carnitine palmitoyl transferase 1 deficiency Other inherited metabolic disorders Hyperammonaemia, hyperornithinaemia, homocitrullinaemia syndrome Lysinuric protein intolerance Hyperinsulinism hyperammonaemia syndrome Mitochondrial respiratory chain defects Pyruvate dehydrogenase deficiency Ann Clin Biochem 2007; 44: 506–511 Confirmatory test þþþ þ þþ þþ þþþ þþ þþ þþ þ þ þ þ þ Urinary orotate Urinary organic and amino acids þ Intermediary metabolites þ / þ þ þ including lactate, free fatty acids and 3-hydroxybutyrate Insulin measurement Muscle enzyme and DNA studies in mitochondrial disorders Enzyme assay in some cases Reduced level of consciousness in children 509 Table 1 Continued Causes of hyperammonaemia Acquired hyperammonaemia Illness/sepsis Urinary tract infection with a urease-producing organism Ribavarin therapy 5-Fluorouracil toxicity Portosystemic shunting Haemorrhage in the gastrointestinal tract Renal tubular acidosis type 1 Relative NH3 concentration Initial investigations Confirmatory test þþ Clinical assessment Microbiology results and lack of other metabolic diagnoses þ Blood glucose and liver enzyme assay Abnormal liver biopsy and lack of other metabolic diagnoses þ þþþ þþþ þþþ Drug/therapy clinical history Absence of other metabolic causes þ þ þ þ þ þ þ þ þ þ þ þ þ þ þ Reye’s syndrome Drugs Valproate sodium Chemotherapy Parenteral nutrition Ethanol with starvation þ Blood ammonia approximately 600–2000 mmol/L Blood ammonia approximately 200–600 mmol/L þþþ Blood ammonia o200 mmol/L þþ the core investigations already sent to the laboratory, the following investigations should be undertaken and may require referral to a Regional Centre: plasma acylcarnitines plasma amino acids urine amino acids urine organic acids urine orotic acid Treatment Treatments are available to reduce the concentration of ammonia. These include prompt intervention with intravenous glucose and insulin to induce anabolism and reduce further proteinolysis together with the pharmacological use of sodium benzoate or sodium phenylbutyrate to form benzoyl glycine and phenylacetyl glutamine which are excreted thereby removing waste nitrogen. Arginine supplementation is also frequently given as an anaplerotic compound in the urea cycle. In severe cases continuous veno-venous haemo¢ltration may be the treatment of choice. The sooner these treatments are started the better, therefore it is vital that the clinician is made aware of an abnormally high ammonia concentration as soon as it is detected. Appropriate initial therapeutic interventions should be immediately available in all hospitals with neonatal units or paediatric wards undertaking emergency admission to help reduce brain injury. Subsequent transfer to a Regional centre may be indicated to arrange de¢nitive treatment including continuous veno-venous haemo¢ltration. Hypoglycaemia Hypoglycaemia is often one of the ¢rst diagnoses to be considered in a child with a reduced level of consciousness. This is often established at the bedside using a capillary sample and one of the many types of glucometer. These devices are less accurate and more imprecise than standard laboratory methods. In particular, at low concentration they may overestimate true glucose results when compared with standard laboratory methods.8 The national guideline recommends that all children with a decreased level of consciousness should have a laboratory glucose sent to con¢rm the bedside capillary result.2 Therapeutic correction of hypoglycaemia may reduce counter-regulatory hormone concentrations (adrenaline, noradrenaline, cortisol and glucagon) and consequently make laboratory investigations such Ann Clin Biochem 2007; 44: 506–511 510 Bowker et al. as intermediary metabolites (lactate, free fatty acids and 3-hydroxybutyrate) more di⁄cult to interpret and the disturbances observed in urinary organic acid patterns and blood acylcarnitine pro¢les less prominent. Therefore it is important that, if possible, all the investigations are undertaken before the glucose infusion is started. All laboratories serving hospitals with neonatal units or paediatric wards should establish a protocol to investigate unexplained hypoglycaemia in childhood and a useful summary of the causes and investigation is available.9 It may be valid to repeat the tests at a later date just before feeds or even, in rare instances, in a fasted state, although this can be very hazardous in a child with a predisposition to hypoglycaemia. Ketoacidosis Sick children often have a metabolic acidosis due to poor cardiac function and resultant tissue hypoperfusion. If there are ketones in the urine, then that child is in a state of catabolism. A catabolic state is normal after a period of starvation, but it may also signify the presence of a decompensating inherited metabolic illness. The di⁄culty is deciding when to investigate for these rarer causes of ketoacidosis. While mild elevations of plasma lactate are not uncommon and may be related to sampling, an unexplained elevated lactate, greater than 3.5 mmol/L should prompt further metabolic investigations to exclude an organic acidaemia, aminoacidopathy, fat oxidation defect or mitochondrial enzyme defect. The lactate concentration can be measured on the £uoride oxalate sample sent with the core investigations, but more frequently can be ascertained from blood gas analysis. Elevated lactate results identi¢ed in this way should be con¢rmed using standard laboratory methods if systematic di¡erences exist or reference ranges di¡er. The further tests required when ketoacidosis is detected in the core investigations are: plasma lactate plasma amino acids urine amino acids urine organic acids plasma acylcarnitines The de¢nitive tests to detect the underlying cause may sometimes require a skin ¢broblast biopsy for enzyme assay or a sample of muscle for mitochondrial studies. A muscle biopsy should be considered if the child’s condition deteriorates rapidly, so that a diagnosis may be made for genetic counselling of the parents at a later date if the child does not recover. Ann Clin Biochem 2007; 44: 506–511 The initial treatment for signi¢cant ketoacidosis is to induce anabolism. This is achieved with a high concentration glucose infusion and an insulin infusion if hyperglycaemia develops. Once the underlying cause is identi¢ed this may help identify more speci¢c treatment. Cause unknown In many circumstances, the cause of a reduced level of consciousness remains unknown after completion of the core tests. If the clinical picture, glucose, ammonia and pH have not provided any clues or if there is evidence of raised intracranial pressure or an intracranial abscess is suspected, it is advised that the patient is treated for infection and further tests are requested, including imaging studies of the head. An important cause of coma is drug ingestion,1,9 be that accidental in the toddler age group or deliberate in the older child. The further laboratory tests to request at this stage include urinary organic and amino acids and blood acylcarnitine pro¢le to exclude an occult metabolic cause. Urine toxicology should rapidly identify the presence of substances in the child which may cause a reduced level of consciousness. The panel of tests should include drugs of abuse and any relevant medicines which the child may have encountered in the home. This will need an accurate history to be taken from the parent or carer. Implementation of the guidelines For clinical guidelines to have an impact on patient outcomes they have to be successfully adopted and used by health-care professionals. In the case of children with a reduced level of consciousness, the success of the guideline depends on the appropriate investigations being requested at presentation and this requires e¡ective collaboration between clinicians and laboratory sta¡. Although the investigations requested should be uniform for each patient, there will be variation between di¡erent laboratories in how the tests are conducted. The local requirements of each laboratory need to be available to the clinician taking the blood sample. Far too often, precious blood which a junior doctor has struggled to obtain is rendered un-useable by being sent in the wrong bottle. As junior doctors move between hospitals as part of their training, it is easy to see how such mistakes happen if they are not reminded of the individual laboratories requirements. A project being established by a network of clinical laboratories, MetBioNet, which hopes to address this by encouraging local laboratories to help create an Reduced level of consciousness in children investigation package for clinicians. The pack should include: Investigation request forms, appropriately ¢lled in with the core investigations for biochemistry, haematology and microbiology. The correct blood bottles required for the core investigations. Information on how much blood is required in each bottle to enable meaningful analysis. Information on how quickly these samples need to reach the laboratory. In situations where only limited sample volumes are obtained, the priority for analysis will depend on the results of the initial investigations, for instance if a urea cycle disorder is considered, plasma amino-acid analysis may be a priority, whereas if hypoglycaemia is prominent and a fat oxidation defect is suspected acylcarnitine analysis would take priority. Once a laboratory ‘kit’ is established and available, the clinical team can access this when an unconscious child presents, sending o¡ the correct tests in the correct bottles without delay or confusion. The cost of implementing the recommendations for the core investigations is di⁄cult to quantify. Most large hospitals have the ability to perform the core investigations on site without the need to invest in new technology. As the number of children who present with a reduced level of consciousness is relatively small, these recommendations are unlikely to have any direct sta⁄ng implications and the marginal costs of performing the core investigations is small. Consequently, cost should not be a barrier to implementation and the bene¢ts of potentially avoiding serious longterm neurological injury are profound. The guideline has been endorsed by the Royal College of Paediatrics and Child Health and by the British 511 Association for Emergency Medicine and was developed with input from the Royal College of Pathologists along with many other organizations. It is hoped that by standardizing care patients will have improved outcomes. A national audit will assess the implementation and use of the guideline and best practice implementation examples can be shared. The guideline is freely available at www.nottingham.ac.uk/paediatric-guideline References 1 Wong C, Forsyth R, Kelly T, Eyre J. Incidence, aetiology, and outcome of non-traumatic coma: a population based study. Arch Dis Child 2001; 84: 193–9 2 Bowker R, Stephenson T, Atkinson M, et al. The Paediatric Accident and Emergency Research Group. Evidence-based guideline for the management of decreased conscious level in children. 2006. Available at www.nottingham.ac.uk/paediatric-guideline 3 Losty H. Guidelines for the investigation of hyperammonaemia for inherited metabolic disorders (appendix). 2004. UK National Metabolic Biochemistry Network. www.metbio.net 4 Anderson D, Pennock CA, Henderson MJ, Holton JB. The ammonia checker. Ann Clin Biochem 1984; 21: 69 5 Fitzgerald J, Angelides A. The prognostic significance of peak ammonia levels in Reye Syndrome. Pediatrics 1982; 70: 997–1000 6 Uchino T, Endo F, Matsuda I. Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J Inher Metab Dis 1998; 21(Suppl. 1): 151–9 7 Tokatli A, Coskun T, Ozalp I. Fifteen years’ experience with 212 hyperammonaemic cases at a metabolic unit. J Inher Metab Dis 1991; 14: 698–706 8 Balion C, Grey V, Ismaila A, Blatz S, Seidlitz W. Screening for hypoglycaemia in the neonatal intensive care unit (NICU) with the Abbott PCx glucose meter. BMC Pediatr 2006; 6: 28 9 Bonham JR. The investigation of hypoglycaemia during childhood. Ann Clin Biochem 1993; 30: 238–47 Accepted for publication 14 August 2007 Ann Clin Biochem 2007; 44: 506–511