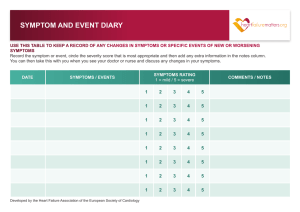
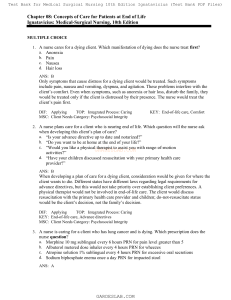
Suggested Answers to Case Studies, Chapter 43, Loss, Grief, and Dying 1a. Factors that contribute to a patient experiencing a “good death” include: Control of symptoms Preparation for death Opportunity to sense a completion of one’s life Good relationships with health care professionals 1b. Care that would be deemed “excellent” for dying patients include: Care that is guided by the values and preferences of the individual patient, maintaining patient independence and dignity Care that attends to the needs of both patient and family Care that focuses on symptom relief, not limited to pain, using both pharmacologic and nonpharmacologic methods Care from all health professionals that have received insightful, culturally sensitive, in-depth training in optimal care for dying patients Provision of adequate funding to research continual improvement in end-oflife care 1c. The best way to meet the needs of a patient who is dying and wants to discuss difficult family conversations is to: Be willing to discuss patient fears and doubts openly Serve as a nonjudgmental listener 1d. Strategies to promote personal communications with patients include: Keep lines of communication open with your patient Provide counseling and death education when patient asks for/needs information Do not provide false reassurance Be willing to engage in personally uncomfortable (yet appropriate) discussions that meet your patient’s needs---your needs are not the priority Be vulnerable to cry, as appropriate Utilize nonverbal communication 1e. Physical signs and symptoms that can signal impending death include: Difficulty talking or swallowing Nausea, flatus, abdominal distention Urinary and/or bowel incontinence or constipation Loss of movement, sensation, and reflexes Decreasing body temperature with cold or clammy skin Weak, slow, or irregular pulse Decreasing blood pressure Noisy, irregular, or Cheyne--Stokes respirations Restlessness and/or agitation Cooling, mottling, and cyanosis of the extremities and dependent areas 2a. The nurse’s role in active euthanasia is one of refusal. It violates the American Nurse Association Code for Nurses to participate in active euthanasia. 2b. Palliative care is holistic care provided across the health--illness continuum. It involves symptom management for patients with chronic conditions. This patient and family might benefit from shifting away from curative care, which includes hospitalization and treatment. The patient’s code status involves aggressive measures to sustain life. Palliative care enables the patient to stay home and have symptoms addressed to ensure comfort. An advanced directive for this patient would be a do-not-resuscitate code status, lifting ethical and legal requirements for life-sustaining measures. 2c. An appropriate reaction of a nurse to the death of a patient for which the nurse has offered care for a significant amount of time includes grieving stages: Denial and isolation Anger Bargaining Depression Acceptance