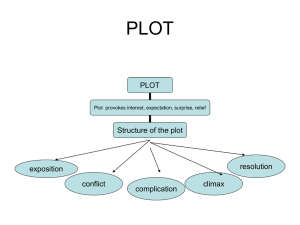
OPERATIVE TECHNIQUES Olivier Delalande, M.D. Fondation Ophtalmologique A. de Rothschild, Pediatric Neurosurgery Unit, Paris, France Christine Bulteau, M.D. Fondation Ophtalmologique A. de Rothchild Pediatric Neurosurgery Unit, Paris, France Georges Dellatolas, M.D., Ph.D. INSERM U 472, Biostatistic and Epidemiology Unit, Hôpital P. Brousse, Villejuif, France Martine Fohlen, M.D. Fondation Ophtalmologique A. de Rothschild, Pediatric Neurosurgery Unit, Paris, France Claude Jalin, M.D. Fondation Ophtalmologique A. de Rothschild, Pediatric Neurosurgery Unit, Paris, France Virginie Buret, Psy. Fondation Ophtalmologique A. de Rothschild, Pediatric Neurosurgery Unit, Paris, France Delphine Viguier, M.D. INSERM U 472, Biostatistic and Epidemiology Unit, Hôpital P. Brousse, Villejuif, France Georg Dorfmüller, M.D. Fondation Ophtalmologique A. de Rothschild, Pediatric Neurosurgery Unit, Paris, France Isabelle Jambaqué, Psy., Ph.D. Université Paris Descartes, Laboratoire Cognition et Comportement, Cedex, France Reprint requests: Olivier Delalande, M.D., Fondation Ophtalmologique A. de Rothschild, Service de Neurochirurgie Pédiatrique, 25–29 rue Manin, 75940 Paris Cedex 19-France. Email: odelalande@fo-rothschild.fr Received, March 24, 2006. Accepted, September 8, 2006. NEUROSURGERY VERTICAL PARASAGITTAL HEMISPHEROTOMY: SURGICAL PROCEDURES AND CLINICAL LONG-TERM OUTCOMES IN A POPULATION OF 83 CHILDREN OBJECTIVE: Hemispherotomy techniques have been developed to reduce complication rates and achieve the best possible seizure control. We present the results of our pediatric patients who underwent vertical parasagittal hemispherotomy and evaluate the safety and global long-term outcome of this technique. METHODS: Eighty-three patients underwent vertical parasagittal hemispherotomy by the same neurosurgeon (OD) between 1990 and 2000. We reviewed all patients between 2001 and 2003 for a standard global evaluation. The general principle is to achieve, through a posterior frontal cortical window, the same line of disconnection as performed with the classic hemispherectomy, while leaving the majority of the hemisphere intact along with its afferent and efferent vascular supply. RESULTS: Seventy-four percent of the patients were seizure-free; among them, 77% were seizure-free without further drug treatment. Twelve percent rarely had seizures (Engel Class II) and 14% continued to have seizures (Engel Class III or IV). The results varied according to the etiology, but this variation was not statistically significant. The early postoperative course was uneventful for 94% of the children, and shunt placement was necessary in 15%. We found a correlation between the preoperative delay and the Vineland Adaptive Behavior score: children with a longer duration of seizures had lower performances. CONCLUSION: Vertical parasagittal hemispherotomy is an effective surgical technique for hemispheric disconnection. It allows complete disconnection of the hemisphere through a cortical window with good results in terms of seizure outcome and a comparably low complication rate. KEY WORDS: Children, Epilepsy surgery, Hemispherectomy, Hemispherotomy, Long-term outcome Neurosurgery 60[ONS Suppl 1]:ONS-19–ONS-32, 2007 A mong the patients who experienced pharmacologically refractory seizures associated with a clinical hemispheric syndrome owing to a diffuse pathology of one cerebral hemisphere (21), functional hemispherectomy presents an effective surgical procedure and has the highest rate of seizure control (9, 31). Approximately 77 to 80% of the patients who underwent an operation were seizure-free in the first reported series. Such a surgical procedure has been largely proposed in children with catastrophic epilepsy associated with a congenital or acquired hemispheric cerebral pathology. The classical procedure of anatomic hemispherectomy (5, 15, 17) was progressively abandoned by neurosurgeons to DOI: 10.1227/01.NEU.0000249246.48299.12 avoid long-term complications or, in some cases, fatal outcomes, mainly owing to cerebral hemosiderosis that resulted from dead space produced by removal of the entire hemisphere (10, 16, 19, 22), as well as immediate postoperative risks such as considerable intraoperative blood loss (3, 20). Adams (1) proposed to turn subdural dead space into epidural dead space. In 1983, functional hemispherectomy was introduced by Rasmussen (22) based on a combination of partial anatomic excision and disconnection of the remaining lobes. Furthermore, hemidecortication was proposed by removing only the gray matter, sparing as much as possible of the white matter and avoiding opening of the ventricle (2, 12, 32, 33). However, the effi- VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 | ONS-19 DELALANDE ET AL. ciency of this technique on seizure control was diminished, especially in the group of children with diffuse cortical dysplasia (4). To further decrease complication rates, new surgical procedures have been developed that reduce the volume of brain removal and increase the ratio of disconnection to resection. These surgical techniques require a smaller skin incision and bone flap, which offers the advantages of reducing blood loss and avoiding the exposure of large venous sinuses. This concept replaces the term “hemispherectomy” with “hemispherotomy,” as proposed by Olivier Delalande in 1992 (7). Various modifications of the hemispherotomy have been described (3, 7, 8, 24, 25, 27, 28). The peri-insular hemispherotomy proposed by Villemure and Mascott (28) and the so-called “modified lateral hemispherotomy” (3) are the largest reported series to date. However, they are more difficult to perform in children born with cerebral malformation (hemimegalencephaly or cortical dysplasia) because of abnormal brain parenchyma and ventricular anatomy. Moreover, in these series, different hemispherectomy techniques were applied with a relatively short-term follow-up period and small number of patients. Holthausen et al. (11) reported on the largest retrospective multicenter study to date. In that study, there was a complete disappearance of seizures in approximately 50 to 70% of the patients. The surgical technique with the best results was the “hemispherotomy technique.” But, long-term postoperative outcome (⬎5 yr) seems to be less effective, with a decrease of seizure-free patients from 76% at 1 year postoperatively to 58% at the time of the 5-year follow-up examination (14). Moreover, it is accepted that postoperative seizure outcome is influenced by the underlying pathology, with the worst outcome in the group of “hemispheric cortical dysplasia” compared with patients with Sturge-Weber syndrome, Rasmussen encephalitis, or vascular insults. We present the vertical approach of hemispherotomy that we have used for the past 15 years, which differs from the previous techniques in two main aspects: 1) the major principle is to further reduce the extent of brain resection by increasing the amount of disconnection, thereby introducing the concept of hemispherotomy and 2) the use of the vertical approach rather than the lateral approach offers the possibility of doing exactly the incisions performed in anatomic hemispherectomy, based on reliable landmarks. This allows the surgeon ensure that an effective total disconnection of the hemisphere is achieved. The technique that we propose to call “vertical parasagittal hemispherotomy” (VPH) is described in this article because it differs from the previous surgical techniques of functional hemispherectomy. The aim of this retrospective study is to report on our results of a large population of children operated by the same surgical technique (VPH) and by the same neurosurgeon (OD) to appreciate the safety of this technique and evaluate the global long-term outcome. PATIENTS AND METHODS The patient is operated on in the supine position with the head in a neutral position, but slightly elevated in the horizon- ONS-20 | VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 tal plane. A small parasagittal frontoparietal craniotomy (approximately 3 ⫻ 5 cm, 1 to 2 cm from the midline, one-third anterior and two-thirds posterior to the coronal suture) is performed with the posterior frontal and central region exposed (Fig. 1A). A limited cortical resection of approximately 3 ⫻ 2 cm is performed, reaching the ependyma of the ventricular roof (Figs. 1B, 1C, 2, and 3). The ventricle is opened, thereby delineating the midline region as well as the posterior aspect of the thalamus, and anteriorly the foramen of Monro. Following the roof of the lateral ventricle mesially, the corpus callosum is identified. By using the ultrasonic aspirator with a low level of vibration (10–20%), the callosal resection is first performed posteriorly towards the splenium (Figs. 1B, 1C, 2, and 3). The midline is always easy to find at this level because the falx cerebri is close to the upper part of the splenium. The resection of the splenium has to be pursued until the roof of the third ventricle and the arachnoid of the cisterna ambiens are exposed. Then, the posterior column of the fornix is cut at the level of the ventricular trigone, from the arachnoid of the cistern ambiens reaching laterally to the choroidal fissure, behind the pulvinar (Figs. 1F, 1G, and 2). The next step consists of performing an incision lateral to the thalamus. Posteriorly, there is no connection at the level of the ventricular trigone. Laterally, one can see the posterior part of the choroid plexus of the temporal horn (Figs. 1F, 1G, and 2), which serves as a guide for the incision lateral to the thalamus. This incision is performed strictly vertically and extends from the trigone to the most anterior part of the temporal horn (Figs. 1I, 1J, 2, 3, 4, and 5), by unroofing the temporal horn entirely, anterior to the coronal plane of the foramen of Monro (cpfM). The incision has to remain within the white matter as laterally as possible to avoid any damage to the lateral aspect of the thalamus. As a next step, the completion of the callosotomy is achieved anteriorly, thereby resecting the genu until just above the anterior commissure (Figs. 1O, 1P, and 2). Just as for the posterior part of the corpus callosum, the section is performed intracallosally to the interhemispheric cistern. The pericallosal arteries (pca) are most often seen through the pia mater. The resection of the genu through the ventricular roof most often requires lifting the patient up to have good visibility anteriorly. It is then necessary to resect the most posterior part of the gyrus rectus (Figs. 1R and 1S). This resection allows one to visualize, across the arachnoid, the first segment of the anterior cerebral artery (aca) and the optic nerve (on), and provides space for a straight incision oriented anterolaterally through the caudate nucleus towards the anterior part of the lateral incision (Figs. 1T, 1U, 2, 3, and 4). This last dissection will cut all the connections from the anterior temporal lobe, the amygdala, and the frontal lobe. The hemispherotomy is now complete, having isolated the entire epileptic cortex from the subcortical structures (Fig. 2A). The whole disconnection is easily performed with the ultrasonic aspirator and with minimal hemorrhage. Perforating arterial branches from the anterior and middle cerebral artery can be easily spared by using a low level of vibration. On the outside, there may be venous bleeding, particu- www.neurosurgery-online.com VERTICAL PARASAGITTAL HEMISPHEROTOMY larly in cases of hemimegalencephaly, but this bleeding is rarely considerable and is usually easily controlled. Two modifications have been implemented since this technique was initiated. The cortical window initially reached the midline. This made the callosotomy easier, but it was then usually necessary to cut large veins close to the sagittal sinus. The cortical window was displaced laterally as described above. Using the lateral approach, it is always possible to spare large veins; a smaller vein can be sacrificed, provided it only drains the cortical region to be removed. The size of the window has been considerably reduced in all cases except for hemimegalencephaly. In the latter cases, the thickness of the brain and anatomic abnormalities make the procedure more difficult, and a larger route is a condition to avoid any damage to the remaining brain. In hemimegalencephaly, the shape of the anterior part of the corpus callosum is sometimes large and/or the frontal horn of the lateral ventricle might be atretic (Fig. 2, B and C). One has to keep in mind that the anatomic guidelines are the upper part of the corpus callosum and the midline arteries. A careful analysis of the three-dimensional anatomy of the affected hemisphere has to be done in cases of hemimegalencephaly and some rare cases of complex hemispheric dysplasia. One must be aware that the brain midline cannot be in the cranial midline. In all of the cases we have encountered, the falx cerebri posteriorly, the roof of the temporal horn laterally, and the pericallosal arteries anteriorly are always remarkable landmarks that should be followed. In all other indications, hemispheric atrophy and lack of change of gross anatomy makes the procedure easy, allowing a narrower route. The hemispherotomy dissection has to be large enough to be assessed by axial and coronal magnetic resonance imaging (MRI) scans. All the children in this series had MRI scans at 3 months postoperatively to exclude complications such as active hydrocephalus or subdural hygroma. The line of the hemispheric disconnection was visible on the axial, sagittal, and coronal planes in all cases (Fig. 2A). We performed a retrospective study of all patients who underwent hemispheric disconnection for hemispheric refractory epilepsy between April 1990 and September 2000. Eightythree patients underwent hemispherotomy by the same surgical technique (VPH) and by the same neurosurgeon (OD). Preoperative evaluation included clinical, neurophysiological (video electroencephalographic [EEG] telemetry), and neuroradiological (MRI) investigations in all patients with or without neuropsychological testing, single-photon emission computed tomography, Wada testing, and functional MRI scans. All data were discussed at our multidisciplinary staff conferences. Sixtyfive children were from France and 18 were from other countries. Postoperative follow-up examinations were performed at 3 months and 1 year. They included a clinical evaluation, assessment of seizure outcome, cerebral MRI scans, and EEG. Thereafter, most of the children were seen for clinical evaluation, depending on the evolution, until the end of the antiepileptic drug treatment. To analyze the long-term neurological, cognitive, and social outcome of this large population, we have reviewed all French patients and have included an NEUROSURGERY external medical assessment of our foreign population in the period from December 2000 to June 2003. We reviewed the French patients during a 2-day hospitalization at our institution for a standard global evaluation, including seizure outcome, postoperative course, neurological examination, behavioral outcome, and cognitive assessment. Seizure outcome was assessed using the Engel classification (9). Neurological examination included ability to walk and speak, motor and sensibility function, height, weight, head circumference (HC), developmental milestones before and after surgery, type of schooling, weekly rehabilitation schedule, socioprofessional status of parents, and systematic questioning of the parents to evaluate the progress in terms of language, motor, behavior, and any other problems that they had observed since hemispherotomy. We also recorded preoperative data (age of onset of seizures, type of seizures, frequency of seizure at the time of surgery, psychomotor development and clinical status of the child, EEG, and MRI scans) from the medical file of each patient. Behavioral outcome was evaluated using the Vineland Adaptive Behavior Scale (26). This scale is well known to assess four behavioral domains (i.e., communication, socialization, daily living skills, motor skills) in handicapped individuals from birth to adulthood and requires only the information provided by the caretaker of the patient, but not the direct involvement of the child. For all non-French patients, we sent a medical file to the referring epileptologist in each country to analyze the epilepsy and antiepileptic drug treatment and neurological and global social outcome. We present the results of the whole population with respect to seizure outcome, surgery related events, global neurological long-term outcome, and Vineland score assessment. Statistical Analysis Statistical analysis was performed using SAS software (SAS Institute, Cary, NC). The analysis focused on factors associated with the Vineland scores (composite and specific scores), indicating functional outcome. The main associated factors examined were etiological group, age at onset of the seizures, preoperative delay, postoperative follow-up, and the side of the hemispherotomy. The general linear model procedure was used for relations between categorical and continuous variables; the Spearman Rho was used for relations between continuous variables. RESULTS Of the 83 patients (45 boys and 38 girls), 43 (52%) underwent a left hemispherotomy and 40 a right hemispherotomy. The mean age of onset of seizure was 2.1 years (standard deviation [SD], 3.3 yr; range, 0.0–13.5 yr), the mean age at hemispherotomy was 8 years (SD, 7.3 yr; range, 0.2–36yr), and the mean age at the time of evaluation was 12.4 years (SD, 7.7 yr; range, 1.4–37.5 yr). We calculated a preoperative delay of 5.9 years (SD, 6.3 yr; range, 0.25–28.7 yr) as the delay between the age of VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 | ONS-21 DELALANDE ET AL. A B I P Q C D J K R S FIGURE 1. Sequences of the surgical steps for the VPH. A, a parasagittal frontoparietal craniotomy (3 ⫻ 5 cm, 1–2 cm from the midline, one-third anterior and two-thirds posterior to the coronal suture) is performed with the posterior frontal and central region exposed. B–E, in the first step, a lim- ited cortical resection of approximately 3 ⫻ 2 cm is performed (Arrow 1) followed by a posterior callosotomy (Arrow 2). F–H, section of the floor of the ventricular trigone (Arrow 3) in the second step. Arrow 4, posterior part of the temporal horn. I–N, in the third step, a laterothalamic incision onset of seizures and the hemispherotomy and a postoperative follow-up period of 4.4 years (SD, 2.7 yr; range, 0.03–11.3 yr) as the time duration between the hemispherotomy and the age of the evaluation. The medical characteristics are summarized in Table 1. We reviewed all of the French (n ⫽ 65) patients except one (Patient 61) and received the most recent data for all nonFrench (n ⫽ 18) patients except for two (Patients 101 and 103). For these three patients, we picked up data in the medical file from the preceding follow-up visit. The etiology was determined according to the underlying pathology based on imaging and pathological examination. Four groups were identified and consisted of the following: 30 children (36%) with a multilobar cortical dysplasia (MCD; Group 1), 25 children (30%) with Rasmussen encephalitis (RE; Group 2), 10 children (12%) with Sturge-Weber syndrome (SW; Group 3), and 18 children (22%) with ischemic-vascular sequellae (Seq; Group 4). In Group 1, 10 patients presented a large cortical dysplasia, 19 had a hemimegalencephaly, and one had ONS-22 | VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 www.neurosurgery-online.com VERTICAL PARASAGITTAL HEMISPHEROTOMY E F G H L M N O T U V W (Arrow 5) following the roof of the temporal horn of the ventricle is made. O–Q, the fourth step is an anterior callosotomy (Arrow 6). R–S, the fifth step is the resection of the posterior part of the gyrus rectus (Arrow 7). T–X, the sixth step involves the dissection between the resected part of the gyrus rectus and the anterior part of the laterothalamic incision (Arrow 8). X a “hemimicroencephaly.” In Group 4, 11 children had ischemic lesions owing to vascular insult, three had a hemiplegia hemiconvulsion epilepsy syndrome, and three had ischemic sequellae after meningitis. Onset of seizures, the age at hemispherotomy, and the age at evaluation varied significantly according to the etiology (P ⬍ 0.0001) and was earlier in the MCD group and later in the RE group. Preoperative delay tended to be lower in the MCD group than in the other three groups (P ⫽ 0.04). The duration of the postoperative follow-up period was not statistically different between the groups (Table 2). Before hemispherotomy, all of the patients experienced generalized seizures, partial seizures, and/or status epilepticus, but only the MCD group exhibited infantile spasms (57%). The NEUROSURGERY VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 | ONS-23 DELALANDE ET AL. TABLE 1. Results of the 83 patients in this studya Age at Patient onset no. (yr)/sex Age at hemispherotomy (yr) Side Postoperative course Age at evaluation (yr) Multilobar cortical dysplasia Group 1 (n ⫽ 30) 1 0.1/M 1.0 L No complication 8 0.03/F 0.3 L No complication 9 0.16/M 3.9 L No complication 11 0.0/M 0.6 R VPS 12 14 17 0.0/F 0.0/F 4.2/M 22 25 29 32 33 37 4.5 1.5 5.9 7.2 2.6 1.7 7.5 L L L No complication No complication VPS 11.2 5.0 8.5 0.0/M 0.2/M 0.01/M 0.15/F 0.0/F 0.04/M 0.6 7.9 0.3 6.8 1,0 3.6 L R R R L R No complication No complication VPS Scar infection + VPS SDPS No complication 4.0 9.8 5.0 11.3 7.8 5.4 40 43 46 0.08/M 0.0/F 0.0/F 0.4 0.7 0.8 L R L No complication VPS VPS 2.4 3.6 7.3 52 0.08/M 1.2 R SDPS, Ventricul, VPS 3.3 53 55 0.04/M 0.0/F 18.2 0.4 R L No complication SDPS 23.8 11.7 56 0.05/M 6.7 L No complication 12.8 60 62 0.5/F 0.0/M 2.0 1.1 R L No complication No complication 3.5 12.2 70 73 77 0.5/M 0.01/F 0.3/F 3.1 0.4 6.0 R L L 11.8 4.8 9.2 78 0.0/M 11.9 R 79 0.4/F 2.0 L 80 101 114 0.2/F 0.0/F 0.0/M 14.9 2.8 1.0 R R R No complication No complication Severe hydrocephalus at 8 d PO: external derivation, VPS (3 wk PO). Still invalid Insipidis diabetus with metabolic acidosis. Deceased at 3 d PO Reoperated at 18 mo after H. Deceased 2 mo later (infectious disease) Latex allergy. Deceased at 3d PO No complication No complication Rasmussen encephalitis Group 2 (n ⫽ 25) 2 6.0/F 18.9 L No complication 13 9.7/M 17.5 R No complication 15 2.6/F 3.3 R No complication 20 5.7/F 10.6 R No complication 23 7.8/F 14.5 R No complication 24 2.0/F 4.2 L No complication 26 1.2/M 8.7 R No complication 35 13.5/M 16.1 L No complication 45 4.3/F 5.9 R No complication 49 13.0/F 22.7 L No complication ONS-24 | VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 Seizure outcome None None None No Sz during 1yr PO, then daily None None Only 2 Sz at 4 mo PO None None None None Decrease Sz (1/mo) Decrease Sz intensity, but still daily None None No Sz during 8 mo PO, then weekly Decrease Sz, but still weekly None Two episodes of fall (possibly Sz) at 8 yr PO Stopped Sz after H and no seizures at 3 yr PO None No Sz during 8 yr PO, then recurrence only during night (stopped by carbazepine) None None Partial Sz (1/mo to 1/wk) Engel grade Vineland communication Ia Ia Ia IVa 48 89 43 36 Ia Ia Ic 36 Not done 50 Ia Ia Ia Ia IIIa IIIa 70 32 73 35 27 49 Ia Ia IIIa 70 78 47 IIIa 52 Ia Id 20 45 IIc 27 Ia IIa 73 19 Ia Ia IIIa Not done Not done Not done Not done 2.8 3.5 29.0 19.4 9.8 14.3 16.7 5.8 9.9 17.1 13.3 29.9 Stop Sz during 8 mo PO, then weekly IIIa Not done None None Ia Ia Not done Not done Not done None None None Only 4 Sz at 4 mo PO None None None None None Rare episodes of loss of consciousness with fall (stopped by diazepam) Ia Ia Ia Ic Ia Ia Ia Ia Ia IIc 27 57 85 49 62 Not done 48 47 93 19 www.neurosurgery-online.com VERTICAL PARASAGITTAL HEMISPHEROTOMY TABLE 1. continued Age at Patient onset no. (yr)/sex Age at hemispherotomy (yr) Side Postoperative course Age at evaluation (yr) 50 54 3.3/M 1.9/M 8.9 4.1 R R No complication No complication 17.1 11.4 58 63 5.5/M 3.2/F 9.0 14.8 L L No complication No complication 12.7 24.0 65 66 69 71 74 75 82 83 103 10.0/F 4.8/F 10.3/F 4.0/M 3.7/M 2.2/M 6.2/M 7.2/F 3.9/F 13.6 5.8 14.0 5.7 9.6 16.8 13.4 36.0 13.2 R R R R R R R L L No complication No complication No complication No complication No complication No complication No complication No complication No complication 17.3 11.8 17.7 10.7 13.0 24.0 14.6 37.5 13.5 115 10.5/F 14.3 L No complication 18.9 116 3.6/M 13.1 R No complication 21.6 Sturge-Weber syndrome Group 3 (n ⫽ 10) 6 0.1/M 22.7 L No complication 25.3 21 28 39 41 42 57 61 72 105 0.1/M 0.0/F 0.3/F 0.2/M 0.2/M 0.5/F 0.1/M 0.5/M 0.03/F 5.9 0.4 13.9 1.9 1.8 20.6 4.4 1.0 0.6 L L L R L R L R R No complication No complication No complication No complication No complication No complication No complication No complication No complication Ischemic-vascular sequelae Group 4 (n ⫽ 18) 3 0.08/M 6.0 R No complication 4 0.3/F 20.5 L Cutaneous infection of ear 5 0.4/M 11.3 R No complication 7 1.7/M 13.5 R No complication 10 0.6/M 5.9 R No complication 18 0.5/M 20.0 L Ventricul 19 0.01/F 2.5 L SDPS 27 7.8/F 13.3 L No complication 30 1.8/M 5.4 L No complication a 8.7 4.4 16.3 6.3 10.4 24.4 13.5 6.2 4.1 15.8 22.4 13.2 16.5 10.5 28.2 3.7 16.6 13.6 31 34 36 38 0.5/F 0.0/F 0.0/M 0.7/M 3.3 1.2 4.4 5.5 L L L L No complication Ventricul No complication No complication 8.7 2.2 9.3 9.5 44 47 0.07/M 0.4/M 5.5 26.7 L L No complication No complication 6.5 30.1 48 51 67 0.0/M 1.0/F 1.5/M 5.6 4.3 11.6 L R R No complication No complication No complication 9.8 8.7 18.0 Seizure outcome Engel grade None No Sz during 4yr PO, then rare left clonic seizure (stopped by valproate) None Rare Sz during 3 yr PO, then no Sz None None None None None None None None Decrease Sz mainly during night Stop Sz during 2 yr PO, then recurrence (1/mo–1/3 mo) Stop Sz during 1 yr PO, then recurrence mainly during night Vineland communication Ia IIa 37 66 Ia Ic 58 19 Ia Ia Ia Ia Ia Ia Ia Ia IIIa Not done Not done Not done Not done Not done Not done 61 57 Not done IIa 40 IIIa Not done Fall on back at 3 mo and 1 yr PO (possibly Sz) None None None None None None None None Partial Sz (<1/trim) IIa 19 Ia Ia Ia Ia Ia Ia Ia Ia IIb 29 Not done 28 54 44 19 Not done Not done Not done None None None Left hemibody Sz rarely None None TC Sz only with fever None Daily Sz and 2 status epilepticus (stopped with stiripentol) None None None Rare Sz after head injury at 3 yr PO (stopped by valproate) None No Sz during 6 mo PO, then only during night None None None Ia Ia Ia IIIa Ia Ia IIb Ia IV b 19 20 31 Not done 34 19 51 74 19 Ia Ia Ia IIa 39 68 49 47 Ia IId 39 19 Ia Ia Ia 50 81 Not done L, left; R, right; VPS, ventriculoperitoneal shunt; Sz, seizure; PO, postoperative; SDPS, subdural peritoneal shunt; ventricul, ventriculocysternostomy; H, hemispherotomy; TC, tonic-clonic. NEUROSURGERY VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 | ONS-25 DELALANDE ET AL. A FIGURE 2. Parasagittal (A), coronal (B), and axial (C) MRI scans demonstrating the lines of disconnection of the VPH. Pre- (D) and postoperative (E) axial MRI scans of Patient 43 demonstrating right hemimegalencephaly with a large anterior part of the corpus callosum. B D C seizure frequency was daily or weekly in 82% of the children. Nine children underwent other surgery before hemispherotomy, which was inefficient on seizures. These previous surgeries included focal resection (Patients 12, 23, 53, 54, 58, 71, and 83), porencephalic cyst uncapping (Patient 3), and complete callosotomy (Patient 25). After hemispherotomy, 74% of the children (n ⫽ 60) were seizure free (Engel Class I); among these, 76.6% (n ⫽ 46) were free of antiepileptic drugs (Fig. 3). Ten children (12%) had rare seizures (Engel Class II). Eleven children (14%) continued to have seizures and were classified as Engel Class III (n ⫽ 9) or Engel Class IV (n ⫽ 2). The results varied according to the etiology, but this variation was not statistically significant (Fig. 4). In terms of seizure outcome, the best results were achieved in patients with Rasmussen encephalitis and Sturge-Weber disease with 92 and 100% classified in Engel Class I or II, respectively. These percentages were 88 and 75%, respectively, for ischemic-vascular sequellae and cerebral malformation. We did not find any changes in the long-term outcome according to the seizure frequency outcome. There was the same proportion of patients classified as Engel Class I or II regardless of the duration of the follow-up period (Fig. 5). The postoperative course was uneventful for 67 children (80.7%). Transfusion was necessary in 8% of the children. Thirteen children (15.7%) developed postoperative hydrocephalus, for which ventriculocisternostomy was performed in two (Patients 34 and 18), ventriculoperitoneal shunt in seven (Patients 11, 17, 29, 32, 43, 46, and 77), a subdural peritoneal shunt in three (Patients 19, 33, and 55), and all three procedures in one child (Patient 52). One of the children who had ventriculoperitoneal shunt placement developed a local wound infection associated with meningitis (Patient 32). Another child (Patient 77) developed severe intracranial hypertension 8 days ONS-26 | VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 E postoperatively. She underwent external ventricular drainage, then ventriculoperitoneal derivation, but remained in a bedridden state. The cerebral MRI scan, performed at 3 months postoperatively, exhibited a large area of low attenuation in the frontoparietal region on the right side (contralateral to the side of hemispherotomy) in keeping with an extensive cerebral www.neurosurgery-online.com VERTICAL PARASAGITTAL HEMISPHEROTOMY TABLE 2. Medical characteristics according to etiologya Etiology Group 1 (MCD) Group 2 (RE) Group 3 (SW) Group 4 (Seq) P value Age (yr) at onset of seizures (SD) [min–max] Age (yr) at hemispherotomy (SD) [min–max] Age (yr) at evaluation (SD) [min–max] Preoperative delay (yr) (SD) [min–max] Postoperative follow-up (yr) (SD) [min–max] 0.2 (0.76) [0–4.2] 3.7 (4.5) [0.3–18.2] 7.4 (4.7) [1.4–23.8] 3.4 (4.4) [0.3–18.2] 4.3 (3.0) [0.03–11.3] 5.9 (3.5) [1.3–13.5] 12.6 (7.0) [3.3–36.0] 17.2 (7.2) [5.7–37.5] 6.7 (6.0) [0.7–28.7] 4.7 (2.9) [0.3–10.2] 0.3 (0.2) [0.04–0.6] 7.3 (8.6) [0.4–22.7] 12.0 (7.8) [4.1–25.3] 7.1 (8.5) [0.3–22.5] 4.6 (2.4) [2.5–9.0] 1.0 (1.8) [0–7.8] 9.2 (7.1) [1.2–26.7] 13.5 (7.6) [2.2–30.1] 8.5 (7.1) [1.2–26.2] 4.2 (2.6) [0.9–9.7] <0.0001 <0.0001 <0.0001 0.04 0.96 a MCD, multilobar cortical dysplasia; RE, Rasmussen encephalitis; SW, Sturge-Weber syndrome; Seq, ischemic-vascular sequelae; SD, standard deviation ; min, minimum; max, maximum. infarction. Postoperatively, three children died (3.6%), two of them within the first week after hemispherotomy. An 11-yearold boy (Patient 78) developed severe diabetes insipidus with refractory hypernatremia and died on the fourth postoperative day. A 15-year-old girl (Patient 80) died 3 days postoperatively owing to a latex allergy (diapers). The third child, a 2-year-old girl (Patient 79) with hemimegalencephaly, was reoperated (by the same neurosurgeon) 18 months after the first hemispherotomy for recurrent seizures. This was the only child in our series who underwent a ”second-look” surgery for persisting or recurring seizures. As the hemispherotomy was intraoperatively proved to be complete in this case, it was not necessary to perform any other surgical procedure, and the girl was uneventfully discharged at home 10 days postoperatively. She was, however, rehospitalized 1 month later in a context of infectious disease (fever, otitis, gastroenteritis) and clinical deterioration rapidly occurred, requiring intensive care 4 days later. She died 8 days after the onset of her symptoms. The family refused autopsy. The hemiparesis was more important in the upper extremity. Sixty-one children (84%) were able to walk alone or with help, and the ability to walk was preserved in all the children who walked alone before surgery. Among the children who did not acquire independent walk (n ⫽ 12), seven were in the youngest patient group (< 4 yr at evaluation). Four children had a severe mental deficiency associated with multiple cortical dysplasia and one had Rasmussen encephalitis (Patient 63), but lost the ability to walk several years before surgery. When hemispherotomy was performed early in life, the ability to walk was acquired between the age of 19 months and 4 years 4 months. The degree of spasticity of the hemiparetic limbs was different in the RE and the Seq groups than in the other two groups. Whereas the wrist was retracted in the majority of the first two groups (58 and 64%, respectively), the joints showed only a slight retraction or were suppler in most patients in the latter two groups (85%). When testing the ability of the hemiparetic upper limb, 61% were able to put the hand on the head and 30% on the back; none of the children was operated on for this NEUROSURGERY FIGURE 3. Bar graph showing the outcome of the whole population with respect to seizures (mean follow-up period, 4.4 yr; SD, 2.7 yr). FIGURE 4. Bar graph showing outcome seizure versus etiology. FIGURE 5. Bar graph showing the global seizure outcome (Engel classification) according to the duration of the follow-up period. VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 | ONS-27 DELALANDE ET AL. guage in 91 and 82%, respectively, but a worsening in motor function in 26%, particularly concerning the hand function on the hemiparetic side. Vineland Adaptive Behavior Scale FIGURE 6. Scatterplot showing the Vineland communication score versus preoperative delay. spasticity. Ten children (14%) acquired voluntary prehension of the hand on the hemiparetic side and were able to grab a small object (e.g., a pencil). Nevertheless, none of them had fine prehension (thumb-index pincer) or the ability to put a pearl in a bottle. Thirty-six percent of the children were able to hold a small object, and the remaining 50% had no finger movement. Weight was normal in 77%, height in 80%, and HC in 81%. A low weight (<2 SD) was observed in 7% of the children, a low height in 12%, and a low HC in 12%. For these three parameters, an increase (>2 SD) was observed for 9, 8, and 7%, respectively, of the children postoperatively. For sixty-nine patients, we obtained sufficient data concerning school placement and re-education schedules. Considering their routine daily life, all of them had several types of reeducations each week. According to age, thirty-three children (56%) between 3 and 20 years of age (n ⫽ 59) were able to go to school. Among them, 13 were in normal school (nine in nursery school and four in elementary school) and 20 were in specialized schools. Twenty-six (44%) were in an institution. After the age of 20 (n ⫽ 10), all of them were in an institution except one who was in protected employment. Globally, when we asked the parents how they evaluated the outcome of the child, they reported an improvement in behavior and lan- These results concern 58 out of 65 French patients. Seven patients were not included, either because the families were not reliable (Patients 7, 14, and 28) or the patients could not be reviewed (Patients 61, 78, and 79). We did not analyze the results of Patient 83 because she had lobar resection 10 years before hemispherotomy (Fig. 6; Tables 3 and 4). The mean Vineland Composite Score was low (43 ⫾ 15) compared with the norm (100 ⫾ 15), but with heterogeneity according to the domain. The children achieved higher scores in socialization (57 ⫾ 19) compared with communication (45 ⫾ 20) or daily living skills (41 ⫾ 21) (P ⬍ 0.0001). For the socialization and communication domains, there was a wide range of scores, ranging from 19 to 89. The lowest score was observed for motor skills (39 ⫾ 14). For instance, no child was able to ride a bicycle without training wheels or catch a small ball from a distance of 10 feet. According to the side, children with right hemispherotomy showed a better communication score than children with left hemispherotomy. As a function of etiology, the Rasmussen group had the best results in all four domains (Table 3). Preoperative delay was negatively and significantly associated to all the Vineland scores, except for motor skills. The longer the duration of epilepsy, the lower the scores (Fig. 6; Table 4). This relation was similar in right and left hemispherotomy, and it was observed in all four etiological groups. However, it was especially strong in Group 1 (MCD), Group 2 (RE), and Group 3 (SW). Considering the MCD and SW groups (n ⫽ 27) with early onset of seizures, nine had a Vineland communication score of more than 50; of them, eight (91%) had a preoperative delay less than 2 years. Inversely, in the RE and Seq groups (n ⫽ 30), 18 had a Vineland communication score less than 50; of them, 14 (78%) had a preoperative delay of more than 4 years. TABLE 3. Results of the Vineland scalea No. of patients Communication Daily living skills Socialization Motor skills Global score Total (SD) 58 45 (20) 41 (21) 57 (19) 39 (14) 43 (15) Side Right (SD) Left (SD) 24 34 52 (22)b 41 (19)b 43 (21) 40 (22) 59 (20) 55 (20) 53 (21) 46 (20) 47 (18) 41 (16) Etiology G1: MCD (SD) G2: RE (SD) G3: SW (SD) G4: Seq (SD) 21 15 6 16 49 (20) 51 (21) 32 (14) 41 (20) 40 (20) 53 (24) 31 (14) 36 (19) 58 (17) 62 (19) 50 (26) 54 (23) 40 (14)c 64 (23)c 42 (18)c 53 (20)c 43 (15) 51 (18) 35 (15) 40 (17) a SD, standard deviation; MCD, multilobar cortical dysplasia; RE, Rasmussen encephalitis; SW, Sturge-Weber syndrome; Seq, ischemic-vascular sequelae. P ⫽ 0.04. c P ⫽ 0.004. b ONS-28 | VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 www.neurosurgery-online.com VERTICAL PARASAGITTAL HEMISPHEROTOMY TABLE 4. Vineland statistical analysisa Medical characteristics Communication Daily living skills Socialization Motor skills c Global score Age onset of seizure Preoperative delay Postoperative follow-up 0.06 –0.61e –0.37d 0.20 –0.47d –0.34c 0.04 –0.44d –0.18 0.39 0.10 –0.23 0.16 –0.51e –0.31b Right side (n ⫽ 24) Age at onset of seizure Preoperative delay Postoperative follow-up 0.31 –0.65d –0.02 0.39 –0.44b –0.14 0.26 –0.52b –0.08 0.58c 0.07 –0.16 –0.37 –0.54c –0.06 Left side (n ⫽ 34) Age at onset of seizure Preoperative delay Postoperative follow-up –0.17 –0.62d –0.48c 0.08 –0.45c –0.40b –0.11 –0.37b –0.21 0.26 0.12 –0.29 0.005 –0.47c –0.38b Group 1 (MCD) (n ⫽ 21) Age at onset of seizure Preoperative delay Postoperative follow-up 0.13 –0.59c –0.60c 0.12 –0.53b –0.58c –0.06 –0.61c –0.33 0.02 –0.35 0.28 0.07 –0.59b –0.54b Group 2 (RE) (n ⫽ 15) Age at onset of seizure Preoperative delay Postoperative follow-up –0.29 –0.70c –0.26 0.27 –0.60b –0.46 –0.52b –0.57b 0.003 –0.16 –0.43 –0.36 –0.10 –0.78d –0.35 Group 3 (SW) (n ⫽ 6) Age at onset of seizure Preoperative delay Postoperative follow-up –0.20 –0.93c 0.61 0.21 –0.76 0.51 0.31 –0.60 0.03 0.67 –0.09 –0.06 0.03 –0.87b 0.49 Group 4 (Seq) (n ⫽ 16) Age at onset of seizure Preoperative delay Postoperative follow-up 0.01 –0.62b –0.43 0.06 –0.41 –0.48 –0.15 –0.34 –0.36 0.16 0.29 –0.25 –0.003 –0.46 –0.045 Total (n ⫽ 58) Side Etiology a MCD, multilobar cortical dysplasia; RE, Rasmussen encephalitis; SW, Sturge-Weber syndrome; Seq, ischemic-vascular sequelae. b P < 0.05. c P < 0.01. d e P < 0.001. P < 0.0001. This is a large population of children with epilepsy treated by hemispheric disconnection with the same surgical approach and conducted by the same surgeon. Moreover, we were able to obtain recent data for 94% of the operated patients with an important long-term follow-up period. In this article, we described the VPH. We assume that with this vertical approach, a complete disconnection of the affected hemisphere can be achieved and that it offers the advantage of a clear intraoperative assessment of completeness of the hemispherotomy and preservation of an intact vessel supply. Moreover, the incision is limited to the minimum necessary cut to reach to a functional exclusion of the entire hemisphere by respecting the same section as in anatomic hemispherectomy. This technique ensures that the anatomic landmarks take into account the surgical concept of a central core of the hemisphere proposed by Wen et al. (31). The central core of a hemisphere consists of the extreme, external, and internal capsules, claustrum, lentiform and caudate nuclei, and thalamus. Externally, this core is covered by the insula and surrounded by the fornix, choroid plexus, and lateral ventricle. Wen et al. (31) proposed key anatomic landmarks for hemispherotomy techniques that can be used to disconnect the hemisphere from its lateral surface around the insula, through the lateral ventricle, and toward the midline. The parasagittal approach realizes the incision around the central core and makes it easier to assess the completeness of the disconnection. In our popula- NEUROSURGERY VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 | ONS-29 The age at the onset of seizures was not significantly related to the Vineland scores, except for motor skills. The later the onset of epilepsy, the better the motor skills score (P ⬍ 0.01). In the total population, the postoperative follow-up period was negatively correlated with the composite communication and daily living skills scores. The longer the follow-up period, the lower the scores. However, this relation was dependent on the side, being significant only for patients undergoing left hemispherotomy, and on the etiological group, being significant only in the MCD group. In this group, the discrepancy between chronological age and mental age, as evaluated by the Vineland scale, increased with the duration of the postoperative follow-up period. DISCUSSION DELALANDE ET AL. tion, only one child (Patient 79) underwent reoperation for seizure recurrence, despite no signs of incomplete disconnection on the postoperative MRI scans. The hemispherotomy was intraoperatively proven to be complete and no other surgical procedure was performed. Compared with the three techniques of lateral hemispherotomy (24, 25, 27), the interruption of the associative and commissural neuronal fibers is complete because the incision is the same as in the anatomic hemispherectomy (18). It allows a complete disconnection, including the insular cortex, when the lateral approaches require its removal. Furthermore, all the incisions are in a vertical plane. Therefore, it seems more logical to achieve surgery through a vertical route. The long distance between the surface and the deep incisions are not a disadvantage with modern microscopes and a relatively thin ultrasonic aspirator. Moreover, our technique allows the utmost degree of vessel preservation within the disconnected hemisphere (middle cerebral artery and main venous drainage systems), reducing the risk of brain swelling secondary to ischemia (6). In the “modified” lateral hemispherotomy described by Cook et al. (3), the principle of this technique was to create a working space around the ventricular system by removing most of the thalamus, basal ganglia, and caudate nucleus associated with early ligation of the MCA. This technique was compared with anatomic and functional hemispherectomy and resulted in fewer perioperative risks and a shorter hospital stay than the two older techniques. Postoperative mortality and morbidity was reported in detail by Cook et al. (3) and Jonas et al. (14), who compared the advantages and disadvantages associated with each hemispherectomy technique (anatomic, functional, and modified lateral hemispherectomy). They demonstrated that modified lateral hemispherotomy seemed to have the lowest complication rate (35, 34, and 11%, respectively) and a reduced necessity of shunt (78, 9.4, and 22%, respectively), even if the modified lateral hemispherotomy technique suggests a higher shunt rate than that with the functional hemispherectomy technique. In our population treated by VPH, the necessity for shunt placement was 16% (the complication rate for the others was 6%), suggesting that this technique is successful in improving the safety of hemispherotomy technique. Compared with the other disconnection techniques, VPH can be easier to perform in the group of patients with hemispheric cortical cerebral dysgenesis associated with “catastrophic epilepsy.” These children exhibit seizures, beginning in the first weeks of life, which are usually uncontrolled by the antiepileptic drugs, and evolving in refractory epilepsy with a poor intellectual outcome. It seems, therefore, important to propose an early, safe, and reliable hemispheric disconnection. We have pointed out that shunt placement was necessary in 13 children (16%), among them were 10 in the MCD group (33% of Group 1) and three in the Seq group (17% of Group 4), but none in the two other groups. It is difficult to understand why hydrocephaly is so common in the hemimegalencephaly population. The intraoperative evidence of an abnormal deep venous drainage that is interrupted could be an explanation, ONS-30 | VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 but we have never seen any brain swelling that should happen in such a situation. Concerning the efficacy on seizures, 74% of the patients were seizure-free with no seizure recurrence in a long-term followup period and no necessity to reoperate. Among the surgical techniques for epilepsy, hemispherectomy and hemispherotomy carry the best results in terms of seizure freedom, which permits, after a sufficient follow-up period, the reduction and termination of antiepileptic drug treatment in a high percentage of patients. In our population, we successfully stopped antiepileptic drug treatment in 77% of the group classified as Engel Class I. The factors affecting seizure control are not completely elucidated, but several authors have suggested that differences in etiology, as well as the technique of hemispheric disconnection, explains a portion of this variability. Globally, with lateral hemispherotomy, the rate of patients becoming seizure-free has been indicated to be between 68 and 88% (14, 28). For the modified lateral hemispherotomy, there was a seizure-free outcome in the first 2 postoperative years of 82.7 and 66.7% in patients with cortical dysplasia and Rasmussen encephalitis, respectively. However, the score decreased at 5 years postoperatively to 60.5 and 62.5% (14). The largest study on seizure outcome was reported by Holthausen et al. (11) in a population of 333 hemispherectomies from 13 different centers with a minimum follow-up period of 6 months. The percentage of seizure-free patients was better in the “hemispherotomy” techniques (85.7% were seizure-free) and in the group of patients including Rasmussen, Sturge-Weber, and vascular insults (94.6% became seizure-free). The other group of patients, including cerebral dysplasia and other etiologies (sequellae of infections, postmeningitis, postencephalitis) became seizurefree in 68% of the cases. In our population, Groups 2 (RE), 3 (SW), and 4 (Seq) also presented the best result on seizure outcome with 80, 80, and 78%, respectively, being graded as Engel Class I. It should be mentioned that patients classified in Group 4 concerned various origins of ischemic lesions, among them ischemic perinatal lesions, hemorrhage, postinfectious, and hemiconvulsion hemiplegia epilepsy syndrome. Some of these patients could be classified as other or “miscellaneous” in some studies, which may explain why we do not have as good a result as in the two other groups. Moreover, because the resection of the cortex was standardized in the frontal area according to the vertical approach, but not primarily directed to the anatomopathological diagnosis, it was not possible to make extensive pathological examination for this group. Finally, the MCD group had the least favorable outcome, with only 66% of patients becoming seizure-free. This group also had the highest rate of postoperative shunting (33%). In this group of etiology, there is some difficulty proving that the opposite hemisphere is not affected because there are bilateral interictal EEG abnormalities, and sometimes bilateral neuropathological changes following autopsy (13, 23). Considering the group of children who had undergone surgery before hemispherotomy, seven had focal resection, one www.neurosurgery-online.com VERTICAL PARASAGITTAL HEMISPHEROTOMY had callosotomy, and one had surgery for a porencephalic cyst. Among the seven children undergoing focal resection, five presented with a Rasmussen encephalitis (20% of the RE group) and hemispherotomy was avoided to preserve hand motor function because the children were not yet hemiplegics. However, focal surgery was not efficient because these children remained with frequent epileptic seizures. Therefore, it seemed that the indication of hemispherotomy could be considered in patients with Rasmussen syndrome, even without a complete hemiparesis, but with progressive neuropsychological alterations and/or frequent status epilepticus (29). According to the global long-term evolution assessed by the Vineland scale, we found a strong correlation between the preoperative delay and global long-term outcome according to the three domains of communication, socialization, and daily life ability. The shorter the duration of the seizures, the better the postoperative status of the child in all four etiological groups. These results corroborated with those of Jonas et al. (14), who used the Vineland scale in the postoperative course in a population of 52 children treated by hemispherectomy or hemispherotomy. They suspected that patients with seizure duration of 3 years or less had a better outcome. In our series, we confirmed the significance of performing surgery early after the onset of seizures and proposed to decrease the preoperative delay to 2 years or less, especially in children with MCD and SW who have seizure onset early in life. Although these children made significant progress in the development, we found a negative correlation between the postoperative follow-up duration and the Vineland score, but only in the group of children in whom hemispherotomy was performed on the left side. These children tended to have a less impressive outcome because the discrepancy between chronological age and mental age, as evaluated by the Vineland scale, increased with the duration of the postoperative follow-up period. To our knowledge, we are the first to report on the effect of the long-term follow-up periods on global development. We may hypothesize that, in this group of children, the right hemisphere tends to be unable to develop the same abilities as the left side in the domain evaluated by the Vineland scale. Regarding correlation with global outcome, we should acknowledge that there may be other confounding factors (e.g., preoperative cognitive development, antiepileptic drug, delay coming to surgical attention), which could interfere with prognosis, independent of when the surgery is performed. Further prospective studies are needed. CONCLUSION VPH is a surgical procedure for hemispheric disconnection that, with a low rate of complications, seems to be at least as safe as the other common procedures. Moreover, this procedure allows the achievement of good control for seizures, with 74% of the patients becoming seizure-free. This procedure must be proposed as soon as possible after the onset of epilepsy when a NEUROSURGERY hemispheric syndrome has been precisely documented. Prospective studies should be conducted to confirm these results on a larger population and with longer outcome duration. REFERENCES 1. Adams CB: Hemispherectomy: A modification. J Neurol Neurosurg Psychiatry 46:617–619, 1983. 2. Carson BS, Javedan SP, Freeman JM, Vining EP, Zuckerberg A, Lauer JA, Guarnieri M: Hemispherectomy: A hemidecortication approach of 52 cases. J Neurosurg 84:903–911, 1996. 3. Cook SW, Nguyen ST, Hu B, Yudovin S, Shields WD, Vinters HV, van de Wiele BM, Harrison RE, Mathern GW: Cerebral hemispherectomy in pediatric patients with epilepsy: Comparison of the three techniques by pathological substrate in 115 patients. J Neurosurg 100 [Suppl 2]:125–141, 2004. 4. Cosgrove GR, Villemure JG: Cerebral hemicorticectomy for epilepsy. J Neurosurg 79:473–474, 1993. 5. Dandy WE: Removal of right cerebral hemisphere for certain tumors with hemiplegia: Preliminary report. JAMA 90:823–825, 1928. 6. Daniel RT, Villemure JG: Hemispherotomy Techniques. J Neurosurg 98:438–439, 2003. 7. Delalande O, Pinard JM, Basdevant C, Gauthe M, Plouin P, Dulac O: Hemispherotomy: A new procedure for central disconnection. Epilepsia 33 [Suppl 3]:99–100, 1992. 8. Delalande O, Fohlen, Jalin, Pinard JM: From hemispherectomy to hemispherotomy, in Lüders HO, Comair YG (eds): Epilepsy Surgery. Philadelphia, Lippincott Williams & Wilkins, 2001, ed 2, pp 741–746. 9. Engel J: Outcome with respect to epileptic seizures, in Engel J (ed): Surgical Treatment of the Epilepsies. New York, Raven Press, 1987, pp 553–571. 10. Holthausen H, Pieper T: Complications of hemispherectomy, in Lüders HO, Comair YG (eds): Epilepsy Surgery. Philadelphia, Lippincott Williams & Wilkins, 2001, ed 2, pp 879–883. 11. Holthausen H, May TW, Adams TB, Andermann F, Comair Y, Delalande O, Duchowny M, Freeman JM, Hoffman HJ, May P, Oppel F, Oxbury JM, Peacock WJ, Polkey C, Resnick T, Schramm J, Shewmon DA, Tuxhorn I, Vigevano F, Villemure JG, Wyllie E, Zaiwalla Z: Seizures posthemispherectomy, in Tuxhorn I, Holthausen H, Boenig H (eds): Paediatric Epilepsy Syndromes and their Surgical Treatment. London, John Libbey, 1997, pp 749–773. 12. Ignelzi RL, Bucy PC: Cerebral hemidecortication in the treatment of infantile cerebral hemiatrophy. J Nerv Ment Dis 147:14–30, 1968. 13. Jahan R, Mischel PS, Curran JG, Peacock WJ, Shields DW, Vinters HV: Bilateral neuropathologic changes in a child with hemimegalencephaly. Pediatr Neurol 17:344–349, 1997. 14. Jonas R, Nguyen S, Hu B, Asarnow RF, LoPresti C, Curtiss S, de Bode S, Yudovin S, Shields WD, Vinters HV, Mathern GW: Cerebral hemispherectomy: Hospital course, seizure, developmental, language, and motor outcomes. Neurology 62:1712–1721, 2004. 15. Krynauw RA: Infantile hemiplegia treated by removing one cerebral hemisphere. J Neurol Neurosurg Psychiatry 13:243–267, 1950. 16. Laine E, Pruvot P, Osson D: Ultimate results of hemispherectomy in cases of infantile cerebral hemiatrophy productive of epilepsy [in French]. Neurochirurgie 10:507–522, 1964. 17. Lhermitte J: Ultimate results of hemispherectomy in cases of infantile cerebral hemiatrophy productive of epilepsy [in French]. Encéphale 23:314–323, 1928. 18. Morino M, Shimizu H, Ohata K, Tanaka K, Hara M: Anatomical analysis of different hemispherotomy procedures based on dissection of cadaveric brains. J Neurosurg 97:423–431, 2002. 19. Oppenheimer DR, Griffith HB: Persistant intracranial bleeding as a complication of hemispherectomy. J Neurol Neurosurg Psychiatry 29:229–240, 1966. 20. Piastra M, Pietrini D, Caresta E, Chiaretti A, Viola L, Cota F, Pusateri A, Polidori G, Di Rocco C: Hemispherectomy procedures in children: Haematological issues. Childs Nerv Syst 20:453–458, 2004. 21. Prayson RA, Bingaman W, Frater JL, Wyllie E: Histopathologic findings in 37 cases of functional hemispherectomy. Ann Diagn Pathol 3:205–212, 1999. VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 | ONS-31 DELALANDE ET AL. 22. Rasmussen T: Hemispherectomy for seizures revisited. Can J Neurol Sci 10:71–78, 1983. 23. Robain O, Floquet C, Heldt N, Rozenberg F: Hemimegalencephaly: A clinicopathological study of four cases. Neuropathol Appl Neurobiol 14:125–135, 1988. 24. Schramm J, Kral T, Clusmann H: Transsylvian keyhole functional hemispherectomy. Neurosurgery 49:891–901, 2001. 25. Schramm J, Behrens E, Entzian W: Hemispherical deafferentation: An alternative to functional hemispherectomy. Neurosurgery 36:509–516, 1995. 26. Shimizu H, Maehara T: Modification of peri-insular hemispherotomy and surgical results. Neurosurgery 47:367–373, 2000. 27. Sparrow SS, Balla DA, Cicchetti DV: Vineland Adaptative Behavior Scales (VABS). Circle Pines, American Guidance Service, 1984. 28. Villemure JG, Mascott CR: Peri-insular hemispherotomy: Surgical principles and anatomy. Neurosurgery 37:975–981, 1995. 29. Villemure JG, Vernet O Delalande O: Hemispheric disconnection: Callosotomy and Hemispherotomy, in Cohadon F (ed): Advances and Technical Standards in Neurosurgery. Vienna, Springer-Verlag, 2000, vol 26, pp 25–78. 30. Vining EP, Freeman JM, Pillas DJ, Uematsu S, Carson BS, Brandt J, Boatman D, Pulsifer MB, Zuckerberg A: Why would you remove half a brain? The outcome of 58 children after hemispherectomy—The Johns Hopkins Experience: 1968–1996. Pediatrics 100:163–171, 1997. 31. Wen HT, Rhoton AL Jr, Marino R Jr: Anatomical landmarks for hemispherotomy and their clinical application. J Neurosurg 101:747–755, 2004. 32. Wilson PJ: Cerebral hemispherectomy for infantile hemiplegia. A report of 50 cases. Brain 93:147–180, 1970. 33. Winston KR, Welch K, Adler JR, Erba G: Cerebral hemicorticectomy for epilepsy. J Neurosurg 77:889–895, 1992. Acknowledgments This work was supported by Pfizer Laboratory (MS, MN). We thank Francine Lussier, M.D., Ph.D. (Montreal, Canada) for translation into the French version of the Vineland Adaptative Behavior Scale, Maryse Lassonde, Psy, Ph.D., (Montreal, Canada) for advice, and Philippe Mercier, M.D., Ph.D. (Angers, France) and Etienne Delalande (Paris, France) for help with the figures. ONS-32 | VOLUME 60 | OPERATIVE NEUROSURGERY 1 | FEBRUARY 2007 COMMENTS T he authors provide a retrospective study on a series of 83 cases using the vertical parasagittal hemispherotomy technique. This technique provides seizure outcome and complication rates comparable to other contemporary series of hemispherotomy and functional hemispherectomy. However, the shunt rate is somewhat higher (> 16%). After the initial publication (1), this is the first article in which the reader can easily follow the description of the surgical technique itself. Devin Binder Johannes Schramm Bonn, Germany 1. Delalande O, Pinard JM, Basdevant C: Hemispherotomy: A new procedure for central disconnection. Epilepsia 33 [Suppl 3]:99–100, 1992. T hese authors have much experience and success with this particular hemispheric disconnection technique. As I have learned from the patients in this study, the important factor is getting the hemisphere disconnected with the least amount of trauma to the patient as possible. The authors report their wonderful outcomes in terms of both seizure-free and complication rates. It is important for the epilepsy surgeon to appreciate the individuality of each patient who is a candidate for hemispheric disconnection and to apply the most suitable technique for that patient. For example, minimally invasive techniques may be more suitable for patients with perinatal stroke, whereas a modified functional or anatomic technique may be better suited to patients with hemimegalencephaly. Regardless, the surgeon must be comfortable with the technique performed and this requires adequate training and ongoing experience in the surgical care of these patients. William E. Bingaman Cleveland, Ohio www.neurosurgery-online.com