MIS-C
advertisement
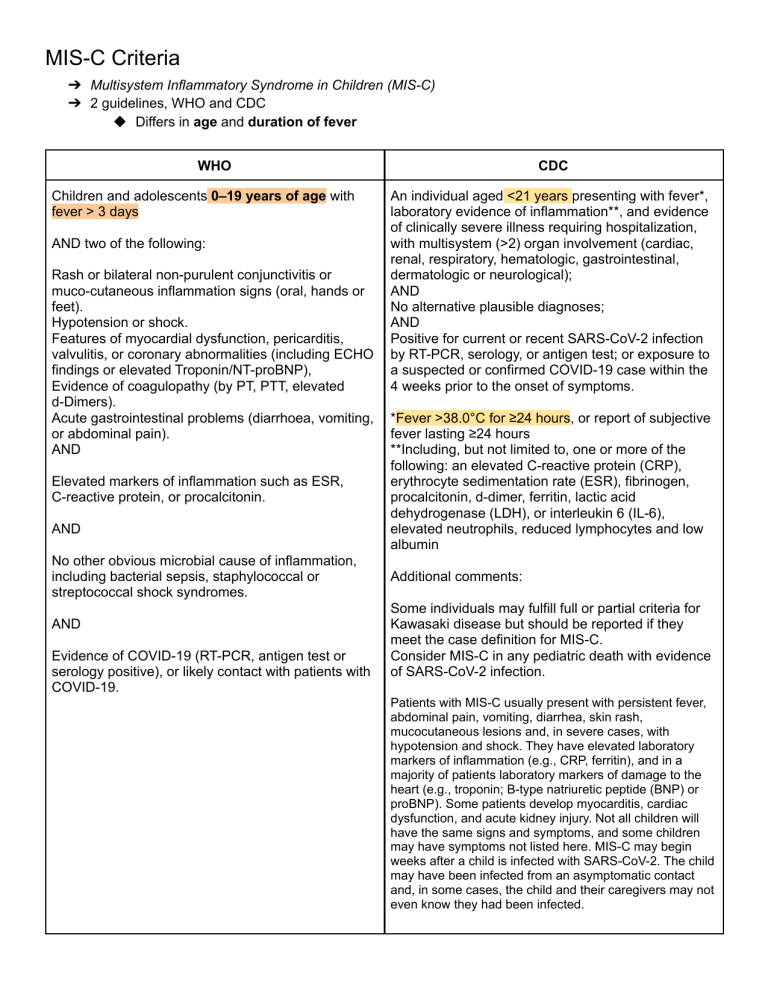
MIS-C Criteria ➔ Multisystem Inflammatory Syndrome in Children (MIS-C) ➔ 2 guidelines, WHO and CDC ◆ Differs in age and duration of fever WHO Children and adolescents 0–19 years of age with fever > 3 days AND two of the following: Rash or bilateral non-purulent conjunctivitis or muco-cutaneous inflammation signs (oral, hands or feet). Hypotension or shock. Features of myocardial dysfunction, pericarditis, valvulitis, or coronary abnormalities (including ECHO findings or elevated Troponin/NT-proBNP), Evidence of coagulopathy (by PT, PTT, elevated d-Dimers). Acute gastrointestinal problems (diarrhoea, vomiting, or abdominal pain). AND Elevated markers of inflammation such as ESR, C-reactive protein, or procalcitonin. AND No other obvious microbial cause of inflammation, including bacterial sepsis, staphylococcal or streptococcal shock syndromes. AND Evidence of COVID-19 (RT-PCR, antigen test or serology positive), or likely contact with patients with COVID-19. CDC An individual aged <21 years presenting with fever*, laboratory evidence of inflammation**, and evidence of clinically severe illness requiring hospitalization, with multisystem (>2) organ involvement (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic or neurological); AND No alternative plausible diagnoses; AND Positive for current or recent SARS-CoV-2 infection by RT-PCR, serology, or antigen test; or exposure to a suspected or confirmed COVID-19 case within the 4 weeks prior to the onset of symptoms. *Fever >38.0°C for ≥24 hours, or report of subjective fever lasting ≥24 hours **Including, but not limited to, one or more of the following: an elevated C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), fibrinogen, procalcitonin, d-dimer, ferritin, lactic acid dehydrogenase (LDH), or interleukin 6 (IL-6), elevated neutrophils, reduced lymphocytes and low albumin Additional comments: Some individuals may fulfill full or partial criteria for Kawasaki disease but should be reported if they meet the case definition for MIS-C. Consider MIS-C in any pediatric death with evidence of SARS-CoV-2 infection. Patients with MIS-C usually present with persistent fever, abdominal pain, vomiting, diarrhea, skin rash, mucocutaneous lesions and, in severe cases, with hypotension and shock. They have elevated laboratory markers of inflammation (e.g., CRP, ferritin), and in a majority of patients laboratory markers of damage to the heart (e.g., troponin; B-type natriuretic peptide (BNP) or proBNP). Some patients develop myocarditis, cardiac dysfunction, and acute kidney injury. Not all children will have the same signs and symptoms, and some children may have symptoms not listed here. MIS-C may begin weeks after a child is infected with SARS-CoV-2. The child may have been infected from an asymptomatic contact and, in some cases, the child and their caregivers may not even know they had been infected. Laboratory Testing ● Testing aimed at identifying laboratory evidence of inflammation as listed in the Case Definition section is warranted. ● Similarly, SARS-CoV-2 detection by RT-PCR or antigen test is indicated. ● Where feasible, SARS-CoV-2 serologic testing is suggested, even in the presence of positive results from RT-PCR or antigen testing. Any serologic testing should be performed prior to administering intravenous immunoglobulin (IVIG) or any other exogenous antibody treatments. Other Evaluations Given the frequent association of MIS-C with cardiac involvement, many centers are performing cardiac testing including, but not limited to: ● ● ● echocardiogram; electrocardiogram; cardiac enzyme or troponin testing (per the center’s testing standards); and ● B-type natriuretic peptide (BNP) or NT-proBNP. Other testing to evaluate multisystem involvement should be directed by patient signs or symptoms. Additionally, testing to evaluate for other potential diagnoses should be directed by patient signs or symptoms. American College of Rheumatology MIS-C Treatment Guidelines Common clinical features ➔ Fever ➔ mucocutaneous findings (rash, conjunctivitis, edema of the hands/feet, red/cracked lips, and strawberry tongue) ➔ myocardial dysfunction ➔ cardiac conduction abnormalities ➔ Shock ➔ gastrointestinal symptoms ➔ Lymphadenopathy ➔ Neurologic involvement (severe headache, altered mental status, cranial nerve palsies, or meningismus, in select patients) ➔ Nonspecific Cardiac involvement Left ventricular (LV) dysfunction (20-55%), coronary artery dilation or coronary artery aneurysm (CAA) 20%, and electrical conduction abnormalities. Valvular dysfunction and pericardial effusion (less frequently) Full diagnostic evaluation: ECG and echocardiogram (to include quantification of LV size and systolic function using end-diastolic volume (and z-score) and ejection fraction (EF) ) Systemic inflammation: In addition to the ESR and CRP level, MIS-C patients typically demonstrate other markers of inflammation, including high d-dimer levels, moderately elevated ferritin levels (often ranging from 500 to 2,000 ng/dl), profoundly increased procalcitonin levels in the absence of bacterial infection, and increased lactate dehydrogenase (LDH) levels. MIS-C Kawasaki Disease African descent and possibly those of Hispanic descent Japan found in children ranging from age 3 months to age 17 years diagnosed before age 5 years Commonly present with LV dysfunction and shock <10% present with KD shock syndrome gastrointestinal and neurologic symptoms more frequently encountered Reported to occur but less likely Lower platelet count, lower absolute lymphocyte count, and higher CRP levels Cardiac management of MIS-C Repeat echocardiograms be obtained from all children with MIS-C at a minimum of 7–14 days and then 4–6 weeks after the initial presentation For those patients with cardiac involvement noted during the acute phase of illness, another echocardiogram at 1 year after MIS-C diagnosis could be considered. Children with LV dysfunction and CAAs will require more frequent echocardiograms. Long-term complications of myocardial inflammation not known. Cardiac magnetic resonance imaging at 2–6 months post–acute illness in those patients who had moderate-to-severe LV dysfunction will allow for evaluation of fibrosis and scarring. For patients with electrical conduction abnormalities. EKG should be performed at a min- imum of every 48 hours in patients who are hospitalized and at each follow-up visit. Treatment A stepwise approach to immunomodulatory treatment in MIS-C is recommended, with intravenous immunoglobulin (IVIG) and/or glucocorticoids considered as first-tier agents. Both IVIG and glucocorticoids, either alone or in combination, are the most commonly used immunomodulatory medications reported to date in MIS-C patients IVIG at a dose of 2 gm/kg low-to-moderate doses (1–2 mg/kg/day) of glucocorticoids were sufficient to treat many MIS-C patients Anakinra is a recommended treatment for MIS-C patients who are refractory to IVIG and/or glucocorticoids. 22% of MIS-C patients recovered with supportive care. some patients with mild symptoms may require only close monitoring, without the use of IVIG and/or glucocorticoids Antiplatelet and anticoagulation therapy in MIS-C ➢ Patients with MIS-C describe marked abnormalities in the coagulation cascade, including prominent elevations in d-dimer and fibrinogen levels, a variable effect on the platelet count, and a high clot strength as determined by thromboelastography ➢ With increased risk of thrombosis ➢ Antiplatelet agents such as aspirin are recommended in patients with KD, because of the presence of platelet activation, thrombocytosis, altered flow dynamics in the affected coronary arteries, and endothelial damage characteristic of this disease . ○ Accordingly, low-dose aspirin (3–5 mg/kg/day up to 81 mg once daily) is recommended in all MIS-C patients with KD features, CAAs, and thrombocytosis. ○ Anti-acid treatments should be used to prevent gastrointestinal complications in MIS-C patients who are taking steroids and aspirin