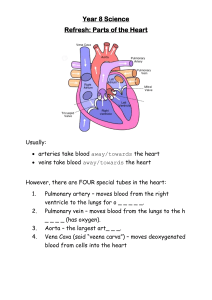
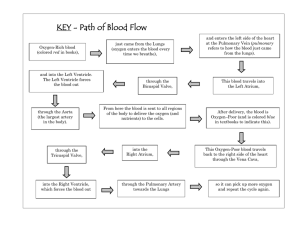
BAROMETRIC PRESSURE AT SEA LEVEL – 760 NUMBERS FOR O2 INSIDE AND OUTSIDE OF THE BODY – INSIDE: 14%, OUTSIDE 20.93% NUMBERS FOR CO2 INSIDE AND OUTSIDE OF THE BODY – INSIDE: 5.5%, OUTSIDE: 0.03% AMOUNT OF PRESSURE IS LOST IN TRACHEA – 47mmHG Heart: Heart Terms: CardiacHeart Rate (HR)Stroke Volume (SV)VO2maxSA nodeAV NodeIntrinsic Rhythmicity/AutorhythmicityForamen Ovale- Fick Equation- 𝑉𝑂2 = 𝑄 𝑥 (𝑎 − 𝑣𝑂2𝑑𝑖𝑓 ) VO2- is the amount of oxygen consumed, usually presented in absolute (L/min) or relative (mL/kg/min) values. Q- Cardiac output, or heart rate (HR) multiplied by stroke volume. Stroke Volume- The volume of blood pumped per beat. a-vO2dif- The amount of oxygen in venous blood returning to the heart, subtracted from the amount of oxygen in the blood that left the heart (on the arterial side) - - According to the Frank-Starling law of the heart the stroke volume of the heart increases as the heart responds to an increase in blood volume in the ventricles before contractionand when all other factors remain constant. In short, the heart pumps what it gets. More blood in equals more blood out. There is no such thing as “deoxygenated” blood in a living creature Blood flow through the heart: - - Blood returns to the heart from the superior (blood from the head and neck, arms and shoulders) and inferior (pretty much blood from every other part of the body) vena cava. Irrespective of where the blood comes from, it winds up being deposited into the right atrium, the first stop in the gas exchange process. From the right atrium blood flows through the tricuspid valve into the right ventricle. Blood then flows into the right ventricle, through the pulmonary valve, and into the right and left lungs via the pulmonary artery. (Arteries carry blood from the heart, while veins carry blood to the heart regardless of oxygen or carbon dioxide concentration.) After gas exchange, blood, now rich in oxygen and much, much lower in carbon dioxide, flows into the left atrium. - Blood then flows through the mitral valve into the left ventricle then through the aortic valve and out into the body. Blood flows into the heart, then into the lungs, and back to the body for distribution to the rest of the body. How the heart beats mechanically - - The heart must be in an orchestrated and precise pattern. Both atria, and then both ventricles, must contract and relax, in the order. While blood is flowing from the superior and inferior vena cava into the right atrium, the left atrium is filling with freshly-oxygenated blood from the lungs. Now filled, the atrium pushed blood, more or less simultaneously, to the ventricles (Lub portion). The “Dub” portion occurs when the ventricles are pushing blood out of the heart, from the right to left ventricles into the pulmonary and systemic circuits respectively. Blood from the right ventricle needs only a small push, into the lungs, to accomplish its goal of moving blood from the heart to the pulmonary circuit. The left ventricle has a much larger task, that of moving blood from the heart throughout the systemic circuit. A much more-forceful contraction is certainly necessary for the heart to successfully complete this task. Notice how much thicker this ventricle is when compared to the right ventricle. HEART VALVES - - The contracting heart is a rather violent event. If you take an individual and have them lay on a flat hard surface, you can see them physically move with each heartbeat. The fibrous skeleton is largely responsible for absorbing this contraction. This cartilage-like part of the heart also serves as the scaffolding around which the heart is built and contains the valves that (when working normally) control blood flow to and from the four chambers of the heart. Cardiac muscles contracts much more quickly than does skeletal muscle. While the latter requires an action potential to be sent down the axon (from either the brain or the spinal cord), across the synaptic cleft, down the transverse tubules and then relies on the release of calcium to bind with troponin, moving tropomyosin from the actin binding site and enabling the crossbridge cycle to initiate, cardiac muscle moves much more quickly. Electrical Flow: Step 1: SA Node activity and atrial activation begins. Time =0 Step 2: Stimulus spreads across the atrial surfaces and reaches the AV node. Time = 50msec Step 3: There is a 100-msec delay at the AV node. Atrial contraction begins. Time = 150msec Step 4: The impulse travels along the interventricular septum within the AV bundle and the bundle branches to the purkinje fibers and via the moderator band, to the papillary muscles of the right ventricle. Time = 175msec Step 5: The impulse is distributed by Purkinje fibers and relayed throughout the ventricular myocardium. Atrial contraction is completed, and ventricular contraction begins. Time = 225msec. - The sinoatrial (SA) node initiates the first impulse. Often called the pacemaker of the heart, the SA node sends the first “signal” (Impulse). This signal really travels in two directions. The flow of - - this signal goes from the SA node to the AV (atrio-ventricular) node, down the monderator band and the left and right bundles branch that separate the right and left ventricles from each other, and through the Purkinje fibers. This is the main highway of flow. These nodal cells establish the rate of contraction; the conducting fibers are responsible for the distribution of the contractile stimulus to the myocardium. But nothing can happen on the highway unless the feeder roads are included. These feeder roads are the intercalated discs. While the signals initiates in the SA node and then is carried to the AV node, the intercalated discs spread this electrical impulse across the right and left atria. This wave of depolarization spreads in a similar fashion to a paper towel absorbing water, if you were to drip a table spoon of water onto a paper towel you would see water spreading in every direction quite rapidly. Both atria contract, pushing blood into the empty ventricles. The atria then “relax” and fill the blood while the ventricles simultaneously contract, pushing blood into the pulmonary artery (The pulmonary tract) for gas exchange or into the aorta (systemic tract) for distribution to the body. Athletes Heart - Cardiac muscle, like skeletal muscle, is very “plastic” in the both types of muscle adapt and change in response to a variety of stimulation. Increased muscle mass increased mitochondrial density, and increase in capillary density in those muscles, all resulting in an increased demand for energy (oxygen). The heart responds to such demands by increasing one component of the Fick equation in particular, stroke volume (SV). “Stroke” refers to the heart beat, and “volume” refers to the amount of blood ejected with each beat of the heart. - - - Notice that as the training impulse (TRIMP, which multiplies the duriation of an exercise training session by the average heart rate achieved during that session, which is then adjusted for the exercise intensity as a function of the heart rate reserve). Note that an increase in TRIMP equates to an increase in exercise intensity and duration. A typical cardiac or pulmonary rehabilitation exercise program is quite low in both intensity and duration in comparison to a typical endurance athlete’s training plan. The intensity (speed, difficulty, etc) and duration (time) are both a factor of training; in addition to the skeletal muscle, hormone and cellular adaptations that take place following both low-and high- intensity endurance training, cardiac muscle also adapts in response to this type of training. These adaptations in the heart result in a more “efficient” heart in that the pumping ability of the heart is increased following both types of training, albeit to a much greater degree in the endurance trained athlete compared with a typical cardiac rehabilitation patient. With increased intensity comes increased change; while we will see improvements in stroke volume (SV) in a cardiac rehabilitation patient following a supervised exercise training intervention, the improvements seen in an endurance-trained athlete will be markedly-improved by comparison. With an increased metabolic demand comes an improved heart; the heart will respond to this increased demand (for oxygen) by delivering more blood, hence more oxygen. While the maximum heart rate (HRmax) of an individual cannot be improved following exercise training, the amount of blood that individual delivers with each beat can. Referring back to the Fix equation, we know that an improvement on the left side of the equation, in this case improved CO via an increased SV, will result in an increase on the left (VO2 or the amount of oxygen consumed per minute). If the heart can deliver more blood with each beat, the body can be supplied more oxygen. This improved delivery results in the ability to perform more work, whether this be as a measure of increased intensity or an improved quality of life – think of a heart transplant patient who could not walk a flight of stairs prior to exercise intervention now enjoying a normal quality of life, where stairs are no longer a barrier, but rather an easy obstacle to overcome. What is the primary purpose of lungs? - Gas exchange Definition of patent - open Definition of foramen - hole Definition of ovale - oval-shaped What are the four sections of the heart? - RA, RV, LA, LV What are the four valves of the heart? - Tricuspid valve, bicuspid valve, pulmonary valve, aortic valve What is the barometric pressure at sea level - 760 #s for O2 inside and outside body - In: 14.5%, Out: 20.93% #s for CO2 inside and outside the body - Inside: 5.5%, Outside 0.03% What amount of pressure is lost in trachea and why? - 47 mmHG and due to water vapor What is intrinsic rhymicity? - Heart beats on its own for a little bit when cut off from rest of body. SA node is pace maker for heart HR is not always equal to exercise or exercise intensity, why? - Drugs are one example that can cause tachycardia (high HR) What is the primary purpose of the heart - Deliver oxygenated blood to tissues How long does the heart spend its life at rest? - Spends 1/3 of its life at rest What is the Fick Equation - VO2= CO x (a-vO2 Dif) What does VO2 stand for - Volume of Oxygen What are the elements of CO - Heart Rate and Stroke Volume What is Stroke Volume - The amount of blood pushed through the heart each beat Why would athlete have lower HRs? - They have a chronic adaptation of stroke volume which allows more blood to be pumped each beat, so they need less pumps per minute to properly supply their tissues. How is the heart selfish and smart? - Takes the best blood for itself Blood Flow through the Heart - SVC and IVC --> Right atrium through the tricuspid valve --> Right ventricle through the pulmonary valve to the pulmonary arteries --> lungs --> pulmonary veins --> left atrium through the bicuspid valve to the left ventricle through the aortic valve to the aorta --> rest of body Why is the left ventricular wall thicker? - Has to be much thicker because the force of contraction needs to be strong enough to push blood all the way down to feet and rest of body What is pericarditis - Infection in pericardial lining What cavity do the heart and lungs sit in? - Pericardial cavity What is the purpose of intercalated discs? - Having intercalated discs help the heart to be connected mechanically, chemically, and electrically. helps to spread the wave of depolarization (like water on a paper towel) and helps with contraction Characteristics of cardiocytes - Interconnected via intercalated discs, a lot of mitochondria and vascularity, almost completely aerobic (hence the large amount of mitochondria), and smaller than skeletal muscle What separates atrial muscle cells and ventricular muscle cells? - the fibrous skeleton What is the fibrous skeleton? - The "Trunk of the Tree" What are the purposes of the fibrous skeleton? - Stabilizes muscle cells and valves, distributes force of contraction Reinforces valves, prevents overexpansion Physically isolates atrial muscle cells from ventricular muscle cells which helps coordinate contractions Supports muscle cells, vessels, and nerves Where does the Right Atrium receive blood from? - Superior and Inferior Vena Cavas What type of blood enters the RA? - Deoxygenated What is the interatrial septum? - Separates right and left atria What is a foramen ovale? - Hole between left and right atrium for blood exchange in a fetus. At birth lungs can function so this is supposed to close What happens if the foramen ovale does not close? - Increased CO2 and decreased O2 What is the fossa ovalis? - The depression in the RA where the foramen ovale was located during development. Sometimes this remains patent and can lead to heart failure Where does the RV receive blood from? - Receives blood from the RA after it has passed through the tricuspid valve (AV valve) What is the purpose of chordae tendinae? - Limits cusp movement, prevents back flow of blood into RA A possible cause for a heart murmur - Pulmonary regurgitation, blood drips back through the pulmonary valve which causes less blood to be available for gas exchange What is the Cardiac Cycle? - The period between the start of one beat to the beginning of the next What is systole? - Contraction What is diastole? - Relaxation What happens during systole? - Blood ejected from chamber into another chamber or the arterial trunk (heart contracting) What happens during diastole? - Chamber fills with blood, prepares for next cycle (at rest) Electrical Flow through the heart - SA node --> depolarization across the atria --> AV node --> depolarization wave progresses to proximal portion of inter ventricular septum via the Bundle of His which divides into left and right bundle branches which goes to Purkinje fibers via moderator band to papillary muscles of RV What is a unique characteristic of Nodal cells? - Membranes spontaneously depolarize. AP sweeps through connective tissue. Cells determine HR. Nodal cells depolarize at different rates The first nodal cell to reach threshold - The pacemaker cell, found in the SA node Why is HR not 80-100 bpm? - ANS slows spontaneous depolarization due to release of Ach from parasympathathetic neurons that slow depolarization How many bpm does SA node generate? - 80-100 bpm What changes at SA node can alter HR - Changes in resting potential or spontaneous depolarization at SA node Brachycardia - low HR Tachycardia - High HR What moves blood? - Pressure What are the arterial layers - Intima, Media, Adventitia Is there gas exchange through arteries or veins? - No, only gas exchange occurs in capillaries Internal elastic membrane - pleated, expands with pressure from heart beat, opens and closes (like grandpa in his elastic pants) Intima - Inner layer of the artery, thick in largest arteries, endothelial lining, layer of connective tissue with elastic fibers Media - middle layer of the artery. smooth muscle in framework of connective tissue. changing diameter changes BP What will sympathetic activation do to the Media - Constriction, vasoconstriction will lead to increase in blood pressure Vasodilation - relaxation of smooth vessels increases the diameter of the lumen, decreased blood pressure results How much blood is on venous vs. arterial side? - 2/3 on venous side, 1/3 on arterial side Adventitia - outermost layer of the after, forms connective tissue sheath around vessel. Thick layer that contains collagen and elastic fibers that blend into adjacent tissues. Stabilizes and anchors vessels Why is it advantageous to have more blood on venous side? - there is extra stuff ready to flow back to the heart for gas exchange What are muscular arteries affected by? - ANS, EPI, NE --> regulate blood flow to individual organs and muscle What are muscular arteries? - Distribution arteries, i.e. femoral artery, brachial artery What is the purpose of muscular arteries? - Transport blood to skeletal muscle and internal organs What are arterioles? - Very small (30 micrograms). Control blood flow between arteries and capillaries Poorly defined adventitia, media not complete What causes a change in arterioles? - They change in diameter in response to local conditions or to endocrine stimulation. What are capillaries? - The smallest blood vessels, size of 1 RBC What is the purpose of capillaries? - Permit exchange between blood and interstitial fluid. Aid in return/waste products, etc. Two types of capillaries - Continuous (has doors) or Fenestrated (Swiss cheese) What are sinusoids - Similar to fenestrated capillaries except have larger pores and thinner basal lamina. Flattened, irregular; following contours of organs. Permit exchange of fluids, large solutes. Blood flow is slow to allow for max absorption Found in liver, bone marrow, suprarenal gland What are venous valves also called? - Skeletal muscle pump Why do we have a skeletal muscle pump? - BP in venules/med-sized veins is too low to oppose force of gravity What are venous valves? - One-way valves that prevent back flow of blood and their movement pushes blood toward the heart Primarily in lower extremities What are are skeletal muscle pumps not found? - the vena cavas What is a damaged skeletal muscle pump? - Varicose veins Veins or arteries are more capable of stretching? - Veins stretch 8x that of arteries What is the primary blood reservoir - Liver What percent of blood in pulmonary circuit? - 10% What percent of blood in heart - 7% What percent of blood in arteries - 13% What percent of blood in capillaries - 7% What percent of blood in systemic venous system (i.e. liver, bone marrow, skin) - 64% What percent in large veins - 18% What are the two types of arteriosclerosis and what is the common result? - Focal calcification and atherosclerosis. Increased blood pressure What is focal calcification - gradual degeneration of smooth muscle, deposition of calcium salts on inside of arteries What is atherosclerosis - Damage to endothelial lining, formation of lipid deposits in media (in vessel wall); most common form of arteriosclerosis Percentage of N inside and outside body - 79.2% Relative Oxygen consumption - 3.5mL/Kg/min Absolute Oxygen consumption - 0.25-0.3 L/min Why are lungs great places for viruses? - High temperatures, lots of carbon dioxide, 100% humidity, and plenty of nutrients. Lungs are similar to external organ in that everything you breathe in comes into contact with them When does larynx close? - during swallowing What are lumen of trachea? - C-shaped cartilaginous rings that hold open the trachea How many times does the bronchial tree before gas exchange - 17-19x What is the main muscle of inspiration and expiration - The diaphragm How do you technically breathe? - The diaphragm pulls down making the thoracic cavity larger. Now there is a vacuum in there and difference in pressure so air wants to go in and goes through fastest route (nose and mouth) What do alveoli sacs look like in during inhale and exhale - Grapes (inhale) and raisins (exhale) Why can't you breathe with a pneumothorax? - there is a lack of pressure gradient because air is escaping into the thoracic cavity and the lung won't inflate against the pressure. By cutting open side one creates a negative pressure and air inside the cavity will flow outside the body allowing the lung to expand. What is the purpose of the thorax? - Provides structure and protection to heart and lungs. Allows for lung volume to change from 1.0-2.5 L to 6-8L. Men generally have larger lungs because they are bigger Do lungs ever fully deflate? - No, this would be bad because then they would stick together What is the purpose of visceral pleura - lubrication Where does gas exchange occur? - In alveoli and capillaries When does gas exchange occur? - When freshly inspired air comes in contact with capillary blood How much of breath is not used? - 1/3 Why is 1/3 of breath not used - Must pass through conducting airways where some air will remain, termed "anatomic dead space" Transport of gasses in alveoli - O2 goes from alveoli into blood, and CO2 in blood goes into alveoli (due to % differences of O2 and CO2 inside and outside the body, hi--> low) What is structural interdependence - Local distortion is opposite by surrounding tissue, i.e. like a trampoline, surrounding parts of lung will support a partial collapse What is the purpose of surfactant - Regulate osmolarity, water pressure, collateral air pathways Helps prevent collapse of alveoli What do Type I alveolar cells do - Create air sacs What do Type II alveolar cells do - Secret surfactant, absorb Na and H20 How does one measure respiratory mechanics - spirometry, measures how much air you have in lung What is tidal volume - The amount of air entering and leaving lungs with regular breathing What is residual volume? - The air that always keeps the lungs slightly inflated, 1/6 of air What is vital capacity? - 5/6 of air, how much lung you have to work with. From maximum inhalation to maximum exhalation What is inspiratory reserve volume? - how much air above tidal volume What is expiratory reserve volume? - how much air below tidal volume what is inspiratory capacity? - wherever in tidal volume, how much more you can breathe in What is forced vital capacity (FVC) - blowing out as fast and hard as you can What is FEV1 - Forced expiratory volume in one second, a good indicator of obstruction in lung. #1 indicator for lung transplant is low FEV1 The effect of pregnancy on diaphragm? - Things expand and diaphragm gets pushed up The effect of pregnancy on total lung capacity - Drops a little bit, lose some residual volume what happens to tidal volume when pregnant? - Tidal volume increases by about 30% either with more breaths or deeper breaths. This costs a log of energy What happens to expiratory reserve volume when pregnant? - A little smaller What happens to inspiratory capacity while pregnant - Increases What happens to vital capacity while pregnant - does not change How many O2 molecules does hemoglobin carry - 4 molecules of O2 What helps assist in O2 transport to tissues? - Decrease in pH, increase in CO2 in blood, increased temperature (all this happens during exercise so think of that) What is fetal circulation - In fetal circulation blood bypasses the lungs because we aren't using them. Uses the foramen ovale to move blood from right atrium to left atrium. Mom's oxygen and nutrients are transferred across the placenta to the fetus What happens with an increase in 2,3-DPG - lower O2 affinity to Hb, increased affinity for deoxyhemoglobin than oxygenated Hb. Releases oxygen to tissues What happens within hours of hypoxia (can occur with high altitude, airway obstruction, or heart failure) - Increase in 2,3-DPG to help unload O2 to tissues How does altitude training work against you? - Lose adaptations of body within a couple of days and you feel like crap while training so its not very effective What happens when you hyperventilate? - Decrease in CO2, sensed by the carotid bodies and body tells you to pass out What are the results of high altitude for days to weeks? - Increase in 2,3-DPG which helps to increase oxygen unloading to tissuesand increase in EPO which increases RBC How does EPO work? - instant increase in RBCs which leads to an increase oxygen carrying capacity in body. Too much ego = blood clots How much more is afffinity for Hb for CO than O2 - 200-250x. CO is dangerous because it can fully saturate Hb at low levels and block sites for oxygen What is DLCO - diffusion capacity of the lungs What is DLCO made up by - Diffusion process through alveolar membrane (gets harder as you get older) and resistance of RBC and chemical combination with Hb How long is diffusion? - 0.25s for gas diffusion, RBC spend 0.75s in alveolar capillaries "transit time" What is severely limited DLCO - less than 0.25s for diffusion. A diffusion abnormality. low oxygen saturation at rest usually due to disease What is the highest altitude that people can live - About 15,000 ft What happens at 27000 ft - You can't digest so you don't eat and your body literally starts to die Why do more people die descending the mountain? - The body has been weakened by being at high altitude and getting low amounts of nutrients so we are more tired (make more mistakes) and more susceptible to illness which can lead to death. Also treatment for a lot of high altitude illnesses involve descent so sick people are more likely to be descending than ascending. What causes acute mountain sickness (AMS) - decreased air pressure and oxygen What increases risk of AMS - Faster ascent, living at a lower elevation normally, and if one has had AMS previously What are the symptoms of AMS - Poor sleep, dizziness, fatigue, decreased appetite, shortness of breath, and increased HR. More severe ones are cyanosis, coughing up blood, confusion, and non-ambulatory Treatment for AMS - Descend, supplemental O2, Drugs that increase blood flow to lungs, open airways, and a diuretic to increase urination How to prevent AMS - Ascend slowly and make frequent stops to rest 1-2 days every 2,000 ft. Supplemental O2 above 10,000 ft and eat and drink water Why would you let your fingers stay frostbitten if you know its only going to get colder? If you want to save your fingers you don't thaw your fingers because this will double the damage done to the tissues in the fingers and is more likely to lead to necrotic tissue/gangrene and amputation. Also more likely to get frostbite again because damaged tissues can't protect against cold as well as healthy tissues. also it hurts to thaw them so why put yourself through that twice Why would you not want to rapidly thaw frostbitten hands? - Potassium flux, hypokalemia, messes with the sodium potassium pump which helps to control heart contractions and can lead to heart arrhythmia or failure. What are the symptoms of High Altitude Cerebral Edema (HACE) - disturbances in consciousness, psychiatric changes, gait changes, confusion, and coma. Usually with appears alongside headache Probably won't be noticed unless by someone else, if by you its too late What is HACE - bleeding in the brain. blood flow out of arteries into the brain When is HACE most common? - abrupt ascent above 3,000m. It is more likely to occur with HAPE Is there such a thing as fully deoxygenated blood? - No, unless you are dead Pressure inside and outside body - Inside: 14.5 X 713 = 104 mmHg. Outside 20.93x 760 = 159 mmHG How does HACE present itself - Mildly drunk, anorexia (almost always), nausea, withdrawn, apathetic, inability to care for oneself and confusion. If one has a coma they are a "goner" Treatment for HACE - diuretic - peeing will help relieve pressure; descend; supplemental Oxygen, hyperbaric bag/chamber at base camps, steroid dose, and in severe cases decrease inter cranial pressure What are the symptoms of high altitude pulmonary edema (HAPE) - dyspnea at rest, cough, weak/decreased exercise, chest tightness, congestion, unable to lie flat because lungs covered in fluid Signs of HAPE - wheezing, crackle in the lungs, central cyanosis (always bad), tachycardia, tachypnea, may cough up pink foamy sputum What are some normal things at high altitudes that aren't normal at low altitudes? Hyperventilation, increased urination, frequent awakening to go pee, insomnia (probably due to cerebral hypoxia), and periodic breathing Treatment for HAPE - Descent, carry the patient because exertion would raise pressure and worsen the illness, keep warm, increase pulmonary dilation, hyperbaric 2-4hrs, diuretics, and supplemental 02 Does blood flow change during exercise? - Blood flow to the heart stays the same but muscles get more blood flow (an increase in a - vO2 difference) Why will VO2 increase with exercise (at muscle)? - An increase in vascularity "more roads" and an increase in mitochondria density "more workers" Why is diving with a Patent Foramen Ovale bad? - Bubbles are found in blood after dives, normally the lungs filter them out but bubbles in people with PFO can bypass the lungs and can cause complications Formula for pressure - Force/Area Continuous force exerted on/against an object by something in contact How much more dense is water than air? - 800x mor dense. 10mi of air = 33ft. (gain 1atm) of sea water What are the three types of decompression illness? - Decompression Sickness (DCS), Arterial Gas Embolism (AGE), Lung over expansion injuries What causes DCS? - Ascending from high pressures too fast What are some other names for DCS? - The bends, Caisson Disease What is AGE? - An embolism is anything in blood stream that can block blood flow. In AGE this is a bubble on arterial side which can block blood to parts of the body Examples Lung Overexpansion Injuries? - Pneumothorax, Mediastinal Emphysema, Subcutaneous Emphysema What is Pneumothorax? - Collapsed Lung What is Mediastinal Emphysema? - A pocket of air within the mediastinum (central cavity in the chest). Bubbles can wind up in brain What is Subcutaneous Emphysema? - More common than Mediastinal Emphysema. Air under the skin goes to base of neck and block blood flow going to the brain What is Nitrogen Narcosis? - Nitrogen does not dissolve into the blood as it should and increased percentage reaches nervous system. Causes a narcotic effect such as euphoria or anesthesia. Very similar to laughing gas O2 Toxicity - Pure O2 lethal beyond 30 ft., when down deep higher conc. of O2 raise risk of O2 toxicity What are the two types of O2 toxicity - Pulmonary and CNS. CNS is more serious than pulmonary toxicity What are symptoms of CNS O2 Toxicity - Visual disturbances, ear disturbances, nausea, twitching, irritability, and dizziness What is most serious problem with CNS O2 Toxicity? - Hyperoxic seizure, feels like a really bad cramp in every single muscle (severe convulsions). Usually lose mouth piece and drown What is the #1 killer of people diving? - Hypocapnia What is hypocapnia? - Lack of CO2 either from voluntary hyperventilation or unintentionally What does hypocapnia lead to? - Shallow water blackout Why can free divers rise rapidly whereas scuba divers cannot? - Since free divers hold their breath their body is pressurized for the surface whereas scuba diver's bodies are pressurized for whatever depth they are at What is hypercapnia? - excessive CO2 in the blood stream. Result of overexertion but can also be from dead air spaces in mask and snorkel What is hypercapnia closely related to? - Skip breathing What does hypercapnia cause? - Headaches, confusion, and feeling of air starvation. Loss of consciousness for body to reset, but this means divers drown What is Carbon Monoxide Poisoning? - Carbon Monoxide binds to Hemoglobin blocking sites for O2, CO bonds with 200x affinity to Hb. Once in respiratory system it can take 812 hours to eliminate What is High Pressure Nervous Syndrome? - There is no clear cause. Suspected that it results from helium interfering with peripheral nervous system, can be offset by using nitrogen or hydrogen. Related to deep diving (300-400ft) What are symptoms of High Pressure Nervous Syndrome? - Hand tremors, cramps, dizzy, vertigo, nausea, loss of coordination Positive Effect of Exercise and Diving - Exercising more than 12 hours before can be beneficial What exercise to avoid before diving? - Avoid rigorous exercise within hours before or after diving. Dehydration and fatigue can lead to a dive related injury and rigorous exercise may raise the # of gas micronuclei on which bubbles form What happens to most of the energy we use? - Burns off as heat What is a result of interfering with air flow? - Interfering with gas exchange Will lung volume change with exercise? - No Why is partial pressure O2 outside body 159 mmHg and inside it is 104mmHg - There is a higher concentration of O2 outside the body than inside the body. Also there is a pressure decrease inside the body due to losing it in the trachea. So a decrease in pressure and oxygen % leads to a lower partial pressure. 760x20.93 =159 and 713x0.03 = 104 Will EPO increase VO2? - Yes, by about 10-15% because Increase in RBC leads to Increase in VO2 Where is ACE found? - Highest density within the capillary beds of the lungs What is the purpose of ACE? - ACE converts Angiotensin I to Angiotensin II. People use ACE inhibitors to help with hypertension What are some effects of Angiotensin II - Increase blood volume (increased BP), systematic vasoconstriction, cardiac and vascular hypertrophy, production of aldosterone (which causes renal sodium and fluid retention) What makes Angiotensin I - Angiotensinogen in kidney interacts with Renin and forms Angiotensin I What are some fear factors? - Increased HR due to flight or fight response in which body is prepping muscles to run. Increased Breathing rate because body preparing to dump out CO2 Alveoli are held together by what? - Elastic bands/fibers What will cause increased unloading of O2 to tissues - Decrease in ph, increase in temperature, and increased 2,3-DPG Formula for max HR - 220-age What causes a decrease in VO2 with increased age? - Lower HR, less muscle available for work due to muscle atrophy, lung volume decreases What is the walk test with HAPE? - If you take pulse ox at rest the numbers will be normal. Get the person to walk and take plus ox. #s will be down if he has HAPE because of desaturation 1 kg - 2.2046lbs absolute VO2 - 0.25-0.3 L/min relative VO2 - 3.5 mL/kg/min Fick Equation - VO2= Q x (a-vO2diff) Blood Flow Through the Heart - sup. & inf. vena cava to right atrium to right ventricle to lungs to left atrium to left ventricle to body tricuspid valve - connects right atrium and right ventricle mitral valve(bicuspid) - connects left atrium and left ventricle pulmonary valve - connects right ventricle and pulmonary trunk aortic valve - connects left ventricle and aorta systole - contraction diastole - relaxation SA node - sinoatrial node (intrinsic pacemaker) oxygen in air - 20.93% carbon dioxide in air - 0.03% oxygen in lungs - 14.5% carbon dioxide in lungs - 5.5% partial pressure of O2 in air - 159 partial pressure of O2 in lungs - 104mm Hg barometric pressure @ sea level - 760mm Hg barometric pressure in lungs - 713 (lose 47 in trachea) concentration gradients go from (blank) to (blank) - high; low primary purpose of lungs - gas exchange pleats - help w/ expansion and contraction (prevents stroking out) SA node begins - depolarization of the atria AV node signals - atrial contraction(filling of the ventricles) electrical signal goes from AV node to: - bundle of His (AV bundle) electrical signal goes from bundle of His to - moderator band electrical signal goes from moderator band to - left and right bundle branches electrical signal goes from L&R bundle branches to - purkinje fibers purkinje fibers stimulate what? - ventricular contraction intrinsic rhythmicity - the heart beats on it's own--does not rely on brain to tell it to beat; pacemaker is usually SA node why is the heart both selfish and smart? - it takes the best(most highly oxygenated blood) for itself ventricular fibrillation - when the heart does not have a regular rhythm; can be deadly; "bag of worms" is HR the best indicator of how hard a person is working? - not always; things like caffeine, drugs, excitement can raise HR also intercalated discs - branch out and ensure that every cardiac cell gets stimulated & contracts; much faster than even skeletal muscle contraction fibrous skeleton - foundation for heart; provides stability and protection; keeps quadrants separate; prevents overexpansion patent - open foramen - hole ovale - oval shaped intima - innermost layer of blood vessels what special structure does the intima contain? - internal elastic membrane (lamina); aids in vessel contraction/dilation media - middle layer of blood vessels; smooth muscle that responds to SNS, hormones...etc; either vascoconstricts or vascodilates adventitia - outermost later of blood vessels; stabilizes and anchors vessels primary purpose of blood vessels - deliver blood flow; NO GAS EXCHANGE muscular arteries - ANS controls diameter depending on how much blood flow is needed "elastic" arteries - stretch depending on blood flow(found right off of the heart) arterioles - very small; have incomplete media and bad adventitia; controls blood flow between arteries and capillaries capillaries - smallest BV; exchange between interstitial fluid and blood flow ONLY done here; can be continuous or fenestrated sinusoids - similar to fenestrated capillaries but have larger pores and a thinner lamina; permits for movement of fluids and larger solutes; found in liver, bone marrow, supraglenoid glands) venous valves - one way valves that help to push blood back up to the heart against gravity; "skeletal muscle pump" activates when we move fraction of blood flow in arteries, heart, and capillaries? - 1/3 (1.5L) fraction of blood flow in veins - 2/3 (3.5L) liver - known as the primary blood reservoir arteriosclerosis - umbrella term for gradual degradation of smooth muscle due to focal calcification (deposit of Calcium) atheroslcerosis - most common type of arteriosclerosis; build up of fat in media; results in increased BP, disease, death...etc foramen ovale - opening in interatrial septum that permits blood flow from right atrium to left atrium; develops in embryo @ 5 weeks and lasts until 48hrs after birth fossa ovalis - when foramen ovale remains open; causes issues with blood flow-especially dangerous for divers heart murmur - leak in pulmonary valve why isn't HR 80-100 bpm? - at rest the PSNS slows HR (via SA node) down to 60bpm by using ACH bradycardia - slow heartbeat tachycardia - fast heartbeat why can't we breathe at high altitudes? - decreased pressure where is gas exchange done? - alveoli ONLY does CO2 go into the blood or out of it? - out of it does O2 go into the blood of out of it? - into main muscle of breathing? - diaphragm how does air go into the lungs? - the diaphragm pulls down on the lungs creating a negative pressure (like a vacuum) and brings air into the lungs what is a side stitch? - term coined for when other muscles of breathing get fatigued because they aren't used to working so hard Why couldn't the guy breathe in the 3 Kings Lung Collapse video? - his lungs couldn't overcome the pressure in his thoracic cavity (pneumothorax) pneuomthorax - abnormal collection of air/gas in pleural space what is "anatomical dead space"? - 1/3 of the air that is inspired; it isn't used, just moves around and stays in lungs what do type 1 alveolar cells do? - create the air sac what do type 2 alveolar cells do? - secrete surfactant (keeps alveoli from collapsing) how should you breathe when trapped on a sinking ship with only limited air space to breathe? - breathe out CO2 underwater so it doesn't take up too much space in the air total lung capacity - gas in lungs after maximum inspiration (VC+ RV= TLC) vital capacity - amount of gas that can be exhaled after maximal inspiration (TV+ IRV+ ERV= VC) residual volume - gas remaining in lungs after a maximal expiration tidal volume - air an individual inspires or expires during normal breathing inspiratory reserve volume - gas an individual can inhale above a tidal volume inspiration expiratory reserve volume - air an individual can exhale beyond a tidal volume expiration functional residual capacity - amount of gas remaining in lung after a tidal volume expiration (ERV + RV) inspiratory capacity - total air breathed in after tidal expiration (TV+ IRV) how many moles of O2 does 1 mole of hemoglobin hold? - 4 increased 2,3 DPG levels will do what? - increase O2 affinity to hemoglobin (dumps it off to tissues easier) when will 2,3 DPG levels increase? - high altitude, exercise why is carbon monoxide deadly? - it's affinity for binding to hemoglobin is 200x that of O2; it blocks O2 binding sites causin sudden death (no warning) VO2 - O2 consumption Q - cardiac output (SV x HR) (a-vO2diff) - difference in O2 consumption between arteries and veins what is a quick fix to hypoxia? - hyperventilation why can training bring resting heart rate down to as low as 40bpm? - training can decrease SV by 50%, so our heart no longer has to work as hard when we are resting at what altitude does digestion stop happening? - 27,000ft when does your body begin to shut down? - 27,000ft Acute Mountain Sickness (AMS) - occurs at high altitudes; drunk//disoriented, dizziness, hallucinations, sleep disturbances, cyanosis how can you prevent AMS? - ascend slowly, frequent stops, supplemental O2, eat, drink...etc High Altitude Cerebral Edema (HACE) - occurs when blood goes into brain, not just to it; change in consciousness & gait; unable to care for oneself; by the time it's noticed it's usually too late High Altitude Pulmonary Edema (HAPE) - coughing up blood, fast heartbeat, chest cyanosis, sometimes diagnosed as pneumonia; do walk test to determine is exercising at high altitudes effective? - no- adaptations only last a few days, and go away once you descend why are you more likely to die on the way down from a mountain? - body is shutting down and more tired, can't recover, AMS, HACE, HAPE Decompression Illness (DCI) - "The Bends"; results from a reduction in ambient pressure; bubbles gather near joints then pop as you ascend; most common type of diving illness two types of DCI? - adrenal gas embolism & lung overexpansion injuries why is an open foramen ovale an issue in diving? - allows bubbles to go into circulation and can cause clots Nitrogen Narcosis - pressure difference allows different amounts of nitrogen to go into brain causing a narcotic effect (can be deadly) CNS O2 Toxicity - pure O2 is lethal beyond 30ft; causes visual and ear disturbances, nausea and twitching hyperoxic siezure - the worst symptom of CNS O2 Toxicity; every muscle twitches in body (painful); diver usually loses mouthpiece and drowns hypocapnia - known as "shallow water blackout"; voluntary hyperventilation from fear/fright/stress; breathe out all co2 causing body to reset hypercapnia - skip breathing; causes headaches, confusion, starvation feeling carbon monoxide poisoning - as pressure decreases on ascend, O2 bonding fails allowing CO to bond and diver to unexpectedly pass out High Pressure Nervous Syndrome - happens when deep diving; hand tremors, cramps, dizziness, vertigo; unsure of cause--maybe helium interference with PNS; N or H offset by helium narcotic response exercise/diving effects - more than 12 hours can add a protective effect; avoid exercise before or after(may increase micronuclei for bubbles to form on) how does free diving work? - divers hold their breath until they reach the bottom (keep in less pressurized air) then breathe out hard and fast as they ascend why are you more likely to die on the ascend while diving? - bubbles in blood, CO2 reduction, carbon monoxide poisoning, AMS Angiotensin Converting Enzyme (ACE) - converts ANGI(non-active) TO ANGII(active) what do ACE inhibitors do? - inhibit ACE; keep body from raising blood pressure why wouldn't you rethaw frostbitten fingers? - 1) they would just refreeze again 2) they freeze like sharp razors, so thawing would cause serious damage to tissues/cells, making them more susceptible to frostbite again, or even amputation why shouldn't frostbite be rewarmed quickly? - due to the arteries being vascoconstricted, potassium accumulates in the fingers; if we rewarm, all of the potassium will rush back to the blood and to the heart which is deadly; potassium messes with the heart's electrical flow increase - ↑ decrease - ↓ muscle - mus, m cardiac muscle - heart - built like skeletal muscle males - m females - f ∆1 - increase in one converting or becoming - → millimol - m/mol lactate dehydrogenase - LDH lactic acid - LA heart rate - HR heart rate reserve - HRR one rep max - 1 RM three rep max - 3 RM kilograms - kg liters - L 1 kg - 2.2046 lbs 100 kgs - 220.46 lbs 1 km - 0.621371 miles 4.0 m/mol - onset of blood lactic acid (OBLA) absolute VO2 - amount of O2 one consumes (in L/min) - resting = 0.25-0.35 L/min relative VO2 - amount of O2 relative to body weight in kg (mL/kg/min) - resting = ~3.5 mL/kg/min VO2 peak - highest VO2 achieved HR max - max heart rate VO2 max - when one has an increase in workload without a concomitant increase in O2 consumption - energy is coming from non-aerobic sources Karvonen formula - max HR is 220-age +- 12.5 bpm (standard deviation) Fick equation - VO2 = Q x (a-VO2 dif) - oxygen consumption = the sum of the number of BPM x. volume of blood pumped each beat x difference between the sum of volume of O2 in venous return - the volume O2 in arterial side after leaving the heart following gas exchange in the lung how to study - look at notes, read and study, outline notes airplanes - fly at 37,000 ft Paul Winchell - developed the patent for the 1st artificial heart - voice for Tigger William Harvey - disagreed with Galen - diagrammed the circulatory system - showed how the heart beats and how blood flows heart - pumps in sequence and sufficiently - when it doesn't pump correctly, something is wrong - still can flow even if the brain is dead - in the center of the body - bone, muscle, and tissue protect it Galen - Greek physician - said the heart didn't do anything vital - believed the liver made blood intrinsic rhythmicity - heart being responsible for the its own heartbeat because it doesn't trust anything - any cell in the heart can be the pacemaker blood flow - to the heart patent - open foramen - hole ovale - oval-shaped heart rate - doesn't equate to exercise or exercise intensity cardiac injury - injury inside the heart - BAD heart disease - number one cause of death in the US - due to hypertension heart - - 1/3 of the time it is at rest, but it never stops - purpose is to deliver oxygenated blood to tissues - takes the best blood for itself = both selfish and smart - takes 7% of all the blood in the body - like one big cell low oxygenated - blood that leaves to the lungs high oxygenated - blood that goes to the heart blood flow through the heart - SVC --> Rt atria --> Tricuspid Valve --> Rt ventricle --> Pulmonic valve --> Lungs --> Lt atria --> Mitral valve --> Lt ventricle --> Aortic valve --> Aorta --> Body hypertension - left ventricle hypertrophy - vascular resistance cardiac, skeletal, smooth - muscle tissues pericardial cavity - pericardial membrane lines this - divided into visceral and parietal pericardium - epicardium bound to muscle tissue or heart membrane of parietal pericardium has dense connective tissue - parietal and fibrous pericardium form the pericardial cavity sac - filled with pericardial fluid epicardium - loose connective tissue of visceral pericardium - bound to muscle tissue of heart parietal and fibrous pericardium - form the pericardial sac pericardial fluid - lubricates the pericardial cavity fibrous pericardium - membrane of the parietal pericardium - dense connective tissue pericardial sac - - protects the heart - like a "garbage bag" - filled with lubricant - acts as a shock absorber - protects from infection structure of heart wall - epicardium, myocardium, endocardium epicardium - visceral pericardium - external surface of the heart - thin (serous) membrane myocardium - middle layer of the heart - multiple layers of heart muscle tissue - connective tissue, nerves, blood vessels - where contraction spreads endocardium - covers inner surface fo the heart intercalated discs - connects cardiac muscle cells - connected mechanically, chemically, and electrically - contraction in any cell triggers the contraction of others - contraction spreads though the myocardium fibrous skeleton of the heart - - stabilizes muscle cells through valves - support for muscle cells, vessels, and nerves - distributes the force of contraction - reinforces the valves and prevents overexpansion - model that the heart is built around - made of cartilage - isolates the atrial muscle cells from the ventricular, coordinating cardiac contractions interatrial septum - separates the left and right atria foramen ovale - lets blood flow directly from the left and right atrium - from the 5th week of embryonic development until birth, then this closes - permanently closes at ~48 hours after birth fossa ovalis - remnant of foramen ovale - sometimes doesn't close (remains patent) - can cause heart failure