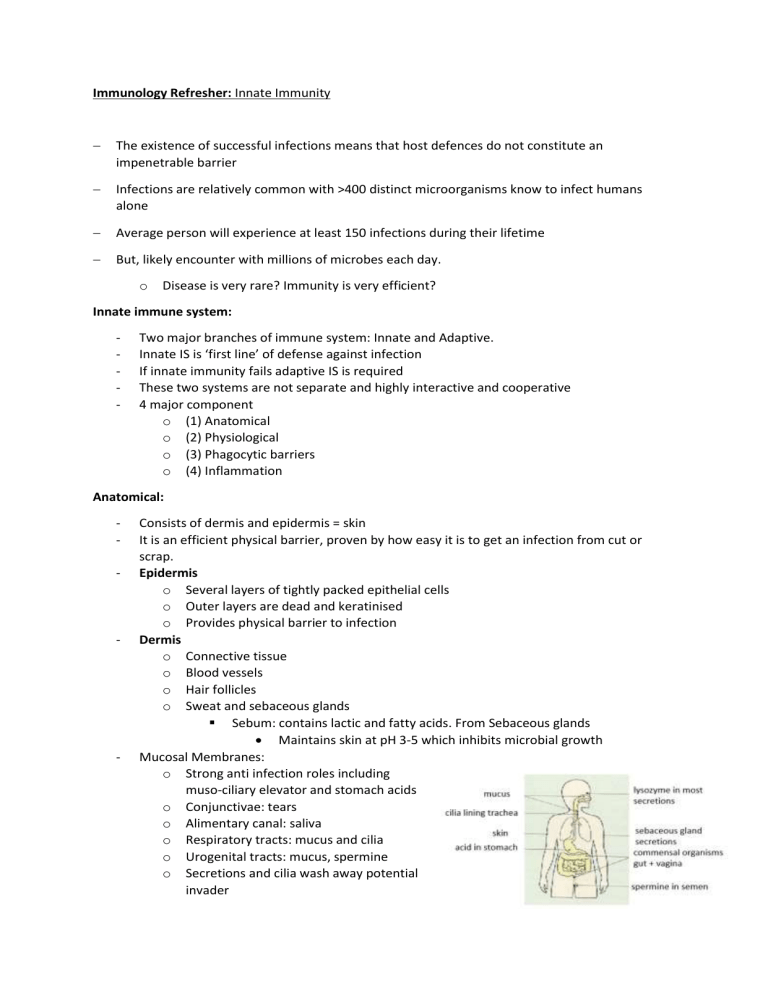
Immunology Refresher: Innate Immunity The existence of successful infections means that host defences do not constitute an impenetrable barrier Infections are relatively common with >400 distinct microorganisms know to infect humans alone Average person will experience at least 150 infections during their lifetime But, likely encounter with millions of microbes each day. o Disease is very rare? Immunity is very efficient? Innate immune system: - Two major branches of immune system: Innate and Adaptive. Innate IS is ‘first line’ of defense against infection If innate immunity fails adaptive IS is required These two systems are not separate and highly interactive and cooperative 4 major component o (1) Anatomical o (2) Physiological o (3) Phagocytic barriers o (4) Inflammation Anatomical: - - - Consists of dermis and epidermis = skin It is an efficient physical barrier, proven by how easy it is to get an infection from cut or scrap. Epidermis o Several layers of tightly packed epithelial cells o Outer layers are dead and keratinised o Provides physical barrier to infection Dermis o Connective tissue o Blood vessels o Hair follicles o Sweat and sebaceous glands Sebum: contains lactic and fatty acids. From Sebaceous glands Maintains skin at pH 3-5 which inhibits microbial growth Mucosal Membranes: o Strong anti infection roles including muso-ciliary elevator and stomach acids o Conjunctivae: tears o Alimentary canal: saliva o Respiratory tracts: mucus and cilia o Urogenital tracts: mucus, spermine o Secretions and cilia wash away potential invader o o o o Secretions also contain anti-bacterial and anti-viral substances Mucus can trap microorganisms (MOs) and cilia can move mucus+MOs from infected area Normal flora: natural, non-invasive, symbiotic MOs that colonise host. Normal flora can outcompete pathogens for attachment sites and nutrients It is a key anti-microbial agent as young babies with underdeveloped immune system = flora helps prevent infection. Physiological Barriers: - - Temperature, pH and various soluble factors can prevent MOs from growing o e.g. gastric juices: very few MOs can survive passage through the stomach at such low pH One of the reason newborns more susceptible to gastrointestinal diseases because stomach contents are less acidic Example of soluble factors: o Lysozyme: hydrolytic enzyme in mucus and tears. cleaves peptidoglycan in bacterial cell walls o Interferons: group of proteins produced by virus-infected host cells Signal to neighbouring un-infected cells to induce an anti-viral state o Soluble factors also include the complement proteins: Complement: serum proteins that circulate in an inactive state that is activated by specific and non-specific mechanisms Four functions in immune response Lysis of cells, bacteria and viruses o Can lyse enveloped viruses o Through MAC Opsonisation, which promotes phagocytosis – key o = coating of bacteria (e.g.) to allow identification by phagocytes which have complement receptors (to detect opsonized C3b) and FC receptors to detect the Fc domain of bound antibodies. o Phagocytes exhibit weak binding to pathogens without opsinisation. o Trigger activation of other IS factors Immune clearance: clumps complexes together to aid clearance from body Cell of the immune system: - Innate immune cells = from myeloid progenitors (except NK cell) Phagocytic Barriers: - Binding of opsins to receptors rearranged the cytoskeleton = allows pseudopod to extend around pathogen to form phagosome. Phagocytosis: o Uptake of material from environment (can include whole MOs) o Once engulfed the vesicle containing the material can fuse to lysozyme containing vesicle o This degrades material o Insoluble material removed from cell by exocytosis o Subversion: Some pathogens survive in phagocytic cells E.g. Salmonella directs uptake and resides intracellularly in Salmonellacontaining vesicle used a type 3 secretion system Prevents phago-lysosomal fusion Provides protected niche within the macrophage, allow it systemic movement. Inflammation: - - - Is the non-specific initial response to tissue injury and pathogen detection. 5 major effects: o Redness o Heat To prevent microbe replication as most microbes have a very small range of temperatures at which replication can occur. o Swelling Causes by recruit of fluid containing signalling molecules and immune cells. o Pain Consequence of swelling, will prevent further injury through use. o Loss of use Histamine is released by damaged tissues. Histamine increases blood flow to the area and causes the capillaries to become leaky, allowing phagocytes and blood clotting factors to the area of damage. Pathogens are recognised, ingested and kill by phagocytes o o - - G-protein-coupled receptors on phagocytes link microbe recognition with increased efficiency of intracellular killing o NADPH Oxidase produces oxygen free radicals which attack nucleic acids NETosis can occur. = programmed death of neutrophils in response to activation. Released DNA and other molecules forms fibrillar net that traps micro-organisms. o The DNA net is covered in anti-microbial factors. Microbial recognition and tissue damage initiates an inflammatory response, releasing cytokines, soluble signally molecules. o Chemokines are a subset of cytokines and recruit immune cells down a gradient. o Immune cells are activated when they leak capillaries. - - Systemic effects occur with local infection. Cytokines get into the peripheral blood stream, and change the surface or circulating immune cells and the endothelial wall in a gradient like fashion = this increases the interaction of leukocytes (WBCs) with the endothelium, slowing them in the blood until they stop at the highest concentration = where infection is. This triggered extravasion and activation, delivering the WBCs to the site of infection, down a gradient. Normal vs too much cytokine activation: o Think about what pathogen causes vs hosts effect. o Systemic infection: macrophage may be activated in the liver – secreting TNFa into the blood directly = making the blood vessels too leaky. o =systemic oedma, decreasing blood volume & collapsing vessels = increase in immune cells. Intra vescular coagulation and organ failure. o Protective response vs pathogenic response. - - Cytokines made by macrophages and dendritic cells induce a systemic reaction known as the acute-phase response o Interferons induced by viral infection make several contributions to host defense o o Intracellular receptors recognise viral DNA/RNA in host and induce anti-viral states in surrounding cells. This may include stopping the formation of activated ribosome, sacrificing cells around the infected one but stopping the spread. Innate Lymphoid Cells amplify signals of innate immunity and have killing features similar to that of cytotoxic T cells, but do not express antigen-specific receptors. = NK Cells - - NK cells are activated by type I interferon and macrophage-derived cytokines They bridge the gap between innate and adaptive immune system. NK cells has inhibitors from MHC1 on healthy cells and activator receptors = stress induced cell antigens on infected cells. - - - o Other viruses may cause an increase in cell stress antigen. 3 major events in inflammation: - - Vasodilation: o causes redness and temp increase know as: erythema o increase in diameter of blood vessels o engorgement of capillary networks as vessels are constricted Increase in capillary permeability o Causes increase in influx of fluid (exudate) into tissue Causes swelling: known as edema Influx of phagocytes from capillaries due to increase permeability o Diapedesis or Extravasation Inflammation Cascade: - - - Initiation and mediators of inflammation poorly understood MOs cause start cascade Damaged host cells start cascade Plasma proteins and products of immune cells can start cascade Factors that can initiate inflammation: o HISTAMINE: principle mediator Chemical released by damaged host cells Binds receptor on nearby capillaries and venules This causes vasodilation and increased permeability Anti-histamines used in allergy treatment o ACUTE-PHASE PROTEINS Found in serum and their concentration in tissue is dramatically increased during inflammation e.g. C-reactive protein: major acute-phase protein produced by the liver. Binds C-polysaccharide found in bacterial and some fungal cell walls Binding activates the complement system o Kinins: Small peptides usually inactive in plasma Tissue injury activates them Can cause vasodilation and increased permeability e.g. Bradykinin: this also stimulates pain receptors in infected area This has protective role preventing further contact with inflamed area o Platelets and fibrin Vasodilation and increased permeability allows clotting factors such as platelets to enter infected area Insoluble fibers of Fibrin are deposited This walls off inflamed area protecting rest of body from potential infection May be subverted – some microbes may benefit from being walled off from adaptive immune system. As infection is being cleared: o MOs are phagocytosed and killed by Innate and Adaptive IS o Accumulation of dead cells, digested material and fluid make up PUS As inflammation subsides: o Debris cleared by phagocytic cells o Tissue is repaired o Capillaries grow into fibrin clot o o Clot dissolves New connective tissue laid down & Scar tissue forms