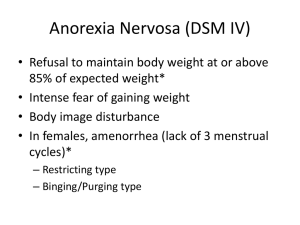
EATING DISORDERS Major Types Anorexia Nervosa - starving Bulimia Nervosa – binging + purging (through vomiting) Binge-Eating Disorder – binging (& distressing over it) Underlying these eating disorders is the drive to become thin Media age of onset: 18 to 21 years Tend to be culturally specific o Until recently, were not found in developing countries where there is limited access to food Recently going global o More than 90% of the severe cases are young females who live in a socially competitive environment o “pro-ana” (anorexia) and “pro-mia” (bulimia) websites and social networks provide grounds for propagation. o Strongest etiological contribution seems to be sociocultural rather than psychological or biological factors persistent lack of recognition of the seriousness of the current low body weight. Specify current severity: The minimum level of severity is based, for adults, on current body mass index (BMI) (see below) or, for children and adolescents, on BMI percentile. The ranges below are derived from the World Health Organization categories for thinness in adults; for children and adolescents, corresponding BMI percentiles should be used. The level of severity may be increased to reflect clinical symptoms, the degree of functional disability, and the need for supervision. Mild: BMI ≥ 17 kg/m² Moderate: BMI 16-16.99 kg/m² Severe: BMI 15-15.99 kg/m² Extreme: BMI < 15 kg/m² BMI – a measure of body fat based on height and weight = weight in kg/(height in m) ² < 18.5 = underweight ANOREXIA NERVOSA Diagnostic Criteria A. Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children and adolescents, less than that minimally expected. B. Intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight. C. Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or 18.5 – 24.9 = normal 25 – 29.9 = overweight 30 – 34.9 = obese 35> = extreme obese Clinical Description - - Has the highest mortality rate of any psychological disorder (included in Barlow & Durand) resulting from restriction of energy intake (Criterion A) o 20% of those who have the disorder die as a result of it Literally means “nervous loss of appetite” o Those with AN, however, often have healthy appetite but has an intense fear of gaining weight or of becoming fat (Criterion B) o - Compared to those with bulimia, they have extraordinary control over their diet and are proud of it. o Many of those with bulimia have a history of anorexia Marked disturbance in body image (Criterion C) o Disturbance in which one’s body image is experienced o Undue influence of body weight or shape on self-evaluation Losing weight means selfcontrol, maintaining or gaining weight is lack of it o Persistent lack of recognition of the seriousness of the current low body weight Two Subtypes - Restricting Type - involves limiting calorie intake Binge-eating-purging Type o Compared to those with bulimia, they binge on relatively small amounts of food and purge more consistently Based on the “last 3 months,” as each subtype may only be a phase Medical Consequences Amenorrhea – cessation of menstruation Dry skin Brittle hair or nails Sensitivity to or intolerance of cold temperatures Downy hair (lanugo) on the limbs and cheeks Cardiovascular problems If vomiting, electrolyte imbalance and resulting cardiac & kidney problems Comorbid Disorders Anxiety disorders, esp. obsessive-compulsive disorder Depressive disorder (71% of cases) Substance abuse (27% of cases) BULIMIA NERVOSA & BINGE EATING DISORDER BULIMIA NERVOSA Diagnostic Criteria 307.51 (F50.2) A. Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following: 1. Eating, in a discrete period of time (e.g., within any 2-hour-period), an amount of food that is definitely larger than what most individuals would eat in a similar period of time under similar circumstances 2. A sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating) B. Recurrent inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics or other medications; fasting; or excessive exercise C. The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months. D. Self-evaluation is unduly influenced by body shape and weight E. The disturbance does not occur exclusively during episodes of anorexia nervosa. Specify if: In partial remission: after full criteria for bulimia nervosa were previously met, some, but not all, of the criteria have been met for a sustained period of time In full remission: after full criteria for bulimia nervosa were previously met, none of the criteria have been met for a sustained period of time Specify current severity: The minimum level of severity is based on the frequency of inappropriate compensatory behaviors (see below). The level of severity may be increased to reflect other symptoms and the degree of functional disability. Mild: an average of 1-3 episodes of inappropriate compensatory behaviors per week Moderate: an average of 4-7 episodes of inappropriate compensatory behaviors per week Severe: an average of 8-13 episodes of inappropriate compensatory behaviors per week Extreme: an average of 14 or more episodes of inappropriate compensatory behaviors per week. Clinical Description - - - Like those with anorexia, people with bulimia have a morbid fear of gaining weight and losing control over eating. o Unlike those with anorexia, those with bulimia have a sense of lack of control over eating (Criterion A.2), which they are ashamed of. Attempts to compensate for the binging (criterion B) by o Purging techniques Self-induced vomiting Using laxatives – drugs that relieve constipation Using diuretics – drugs that result in loss of fluids through increased urination o Excessive exercising Self-evaluation is unduly influenced by body shape & weight (Criterion D) Medical Consequences - - Repeated vomiting causes the ff: o Salivary gland enlargement – which gives the face a chubby appearance o Erosion of the dental enamel on the inner surface of the front teeth o Tear in the esophagus o Electrolyte imbalance – chemical imbalance of bodily fluids, including sodium and potassium levels can result in cardiac arrhythmia (disrupted heartbeat), seizures and renal failure more body fat laxative abuse o severe constipation o permanent colon damage Comorbid Disorders anxiety disorders – historically (80.6% of cases) or concurrently (66%) depressive disorder – historically (50% - 70%) or concurrently (20% of cases) substance abuse (36.8%) BINGE EATING DISORDER Clinical Description - - binge-eating (and marked distress over it) minus extreme compensatory behaviors of those with bulimia new in DSM-5 o elevated to a disorder because of its own pattern of heritability different from anorexia and bulimia, greater likelihood of occurrence in males, and later age of onset. Diagnostic Criteria 307.51 (F50.8) A. Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following: 1. Eating, in a discrete period of time (e.g., within any 2-hour-period), an amount of food that is definitely larger than what most individuals would eat in a similar period of time under similar circumstances 2. A sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating) B. The binge-eating episodes are associated with three (or more) of the following: 1. Eating much more rapidly than normal 2. Eating until feeling uncomfortably full 3. Eating large amounts of food when not feeling physically hungry 4. Eating alone because of feeling embarrassed by how much one is eating 5. Feeling disgusted with oneself, depressed or very guilty afterward. C. Marked distress regarding binge eating is present D. The binge eating occurs, on average, at least once a week for 3 months E. The binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa. BED vs. Obesity Only BED Have concerns about shape and weight Associated with more severe obesity than obesity without BED Some (33%) binge-eat to alleviate “bad moods” or negative affect Obesity Not necessarily concerned about shape and weight Associated with less severe obesity TREATMENT FOR EATING DISORDERS - Treatment program CBT-E (Enhanced Cognitive Behavioral Therapy) IPT (Interpersonal Therapy) Medication o Vyvanse – seems to help people change their behaviors because it is a stimulant; it can be addictive and have side effects; should be monitored by physician o SSRI antidepressants o Anticonvulsant topiramate – which seem to help with binge eating and the thoughts that accompany it. BULIMIA Best treatment: combination of either CBT-E or IPT and SSRI antidepressant (Selective Serotonin Reuptake Inhibitors) Medication: Fluoxetine or Prozac – seem to change chemicals in the part of the brain that affect distorted thoughts seen in Bulimia; help people regain control over their bingeing and purging behaviors ANOREXIA NERVOSA CBT-E or IPT Nutritional Support – team works toward helping people with Anorexia gain weight safely while changing their distorted thinking about food and their bodies. Medication – not shown to be effective to treat Anorexia Nervosa