Dysrhythmias & ECG Analysis: Nursing Education Material
advertisement
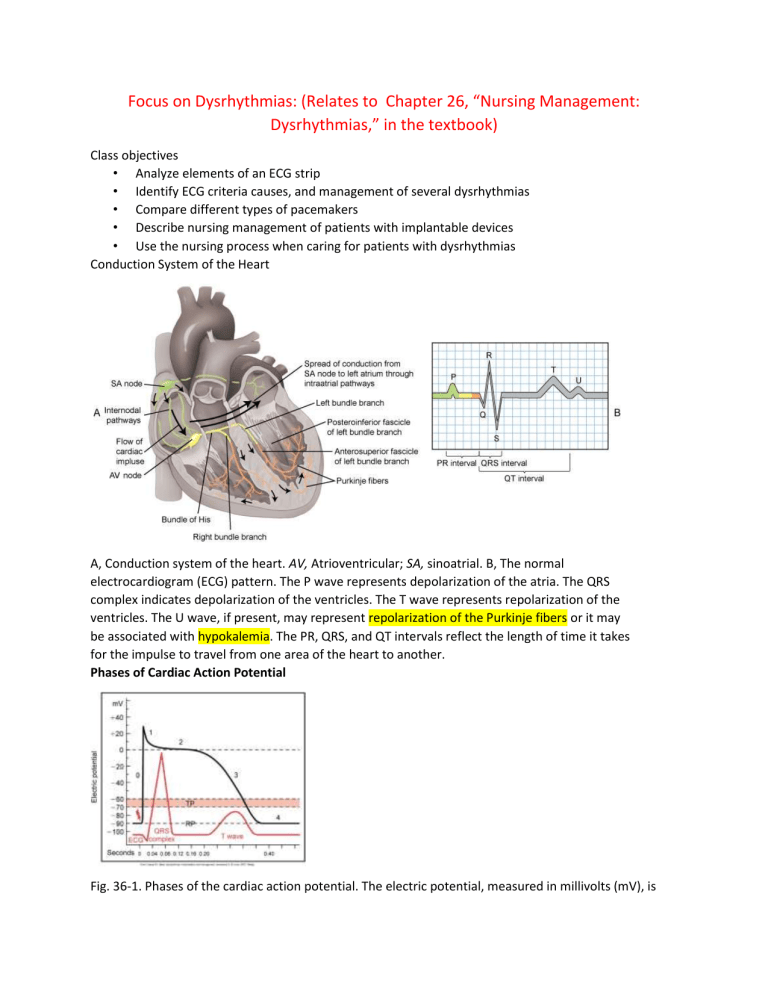
Focus on Dysrhythmias: (Relates to Chapter 26, “Nursing Management: Dysrhythmias,” in the textbook) Class objectives • Analyze elements of an ECG strip • Identify ECG criteria causes, and management of several dysrhythmias • Compare different types of pacemakers • Describe nursing management of patients with implantable devices • Use the nursing process when caring for patients with dysrhythmias Conduction System of the Heart A, Conduction system of the heart. AV, Atrioventricular; SA, sinoatrial. B, The normal electrocardiogram (ECG) pattern. The P wave represents depolarization of the atria. The QRS complex indicates depolarization of the ventricles. The T wave represents repolarization of the ventricles. The U wave, if present, may represent repolarization of the Purkinje fibers or it may be associated with hypokalemia. The PR, QRS, and QT intervals reflect the length of time it takes for the impulse to travel from one area of the heart to another. Phases of Cardiac Action Potential Fig. 36-1. Phases of the cardiac action potential. The electric potential, measured in millivolts (mV), is indicated along the vertical axis of the graph. Time, measured in seconds (sec), is indicated along the horizontal axis. There are five phases of the action potential, labeled as phase 0 through phase 4. Each phase represents a particular electrical event or combination of electrical events. Phase 0 is the upstroke of rapid depolarization and corresponds with ventricular contraction. Phases 1, 2, and 3 represent repolarization. Phase 4 is known as complete repolarization (or the polarized state) and corresponds to diastole. TP, Threshold membrane potential; RP, resting membrane potential. Assessment of Cardiac Rhythm Fig. 36-5. Time and voltage on the electrocardiogram; 6-second strip. Electrocardiogram Monitoring Every normal PR ventricle: 0.12 -0.2 sec (3-5 boxes) QRS: less than 0.12 sec (3-5 boxes) /P should be first to QRS P wave: Indicates atrial depolarization QRS complex: Indicates ventricular depolarization T wave: Indicates ventricular repolarization Interpreting Dysrhythmias: Systematic Analysis of the Electrocardiogram 1. determine the ventricular rate 2. determine the ventricular rhythm 3. determine the QRS duration 4. determine whether the QRS duration is consistent through the strip. 5. Identify the shape of the QRS- is it consistent 6. Identify p waves (is there one in front of every QRS? 7. Identify the P shape 8. Determine the PR intervals-is it consistent. Assessment of Cardiac Rhythm Fig. 36-6. When the rhythm is regular, heart rate can be determined at a glance. The estimated heart rate is 70. Within 6 sec interval it has 7 spaces. So HR is 70. Always use 1500 to divide if we count small squares/Always use 300 if we count large squares Patient Preparation • Clip excessive hair on chest wall. : know org. policy • Rub skin with dry gauze. • May need to use alcohol for oily skin • Apply electrical conductive gel. Change every 48 hours or so Need an order to take out telemetry box Normal Electrical Pattern Fig. 36-9. The electrocardiogram complex as seen in a normal sinus rhythm. 1, P wave; 2, PR interval; 3, QRS complex; 4, ST segment; 5, T wave; 6, QT interval. Isoelectric (flat) line represents the absence of electrical activity in the cardiac cells. (See Table 36-2 for timing of intervals.) The isoelectric line should be flat. If it is elevated, we are suspicious to MI damage. Normal Sinus Rhythm • Reading a strip Fig. 36-8. Normal sinus rhythm in lead II. Artifact Fig. 36-7. Artifact. A, Muscle tremor. B, Loose electrodes. 1. check leads 2. pt may be moving • Regular or irregular??? Sinus Bradycardia Sinus node fires <60 bpm. Normal rhythm in aerobically trained athletes and during sleep Fig. 36-11. A, Sinus bradycardia. P before QRS Have regular rhythm Just slow Cardiac out put is low How to check if the pt is stable: level of consciousness, dizzy. confuse., short of breath, chest pain • Clinical associations • Occurs in response to • Carotid sinus • massage: question in exam: when pt has dizziness, massage artery for 5 sec. • Hypothermia • Increased vagal tone • Lower metabolic needs (sleeping, training, hypothyroidism) • Dizzy, cool, lower consiounce, lower gag reflex • Hypotension • Pale, cool skin • Weakness • Angina • • • • Dizziness or syncope • Confusion or disorientation • Shortness of breath Administration of parasympathomimetic drugs Cause by Medications such as beta-blockers (Ex: atenolol, bisoprolol and carvedilol), calcium? Occurs in disease states • Hypothyroidism • Increased intracranial pressure • Obstructive jaundice • Inferior wall MI. Treatment depends on the cause and symptoms Atropine (0.5 mg OV every 3-5 minutes with a maximum dosage of 3 mg). Pacemaker may be required. Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions: Vasoconstrictor and Blood pressure support Sinus Tachycardia Discharge rate from the sinus node is increased as a result of vagal inhibition and is >100 bpm. Clinical associations Associated with physiologic stressors Exercise Pain Hypovolemia Myocardial ischemia Heart failure (HF) Fever (from meds: Albuterol: atropine, suedafe, leads to high HR, be alert) Clinical significance Dizziness and hypotension due to decreased CO Increased myocardial oxygen consumption may lead to angina. ST Medical Management Depends on the severity of symptoms Cardioversion Vagal maneuvers Carotid sinus massage Bearing down against a closed glottis Applying a cold stimulus to the face Forceful cough Atrial Flutter A condition in which the heart's upper chambers (atria) beat too quickly. A, Atrial flutter with a 4:1 conduction (four flutter [F] waves to each QRS complex). Rhythm is normal, but can’t count below QRS Because of atrial surgery, (Test: may have 3:1) Clinical associations: Usually occurs with CAD Hypertension Mitral valve disorders Pulmonary embolus Chronic lung disease Cardiomyopathy Hyperthyroidism Drugs: Digoxin, quinidine, epinephrine Clinical significance High ventricular rates (>100) and loss of the atrial “kick” can decrease CO and precipitate HF, angina. Risk for stroke due to risk of thrombus formation in the atria SOB shortness of breath, low blood pressure. Treatment Primary goal: Slow ventricular response by increasing AV block -adrenergic blockers Adenosine IV rapid administration immediately followed by 20 ml of saline flush and elevate the arm Electrical cardioversion may be used to convert the atrial flutter to sinus rhythm emergently and electively. Antidysrhythmic drugs (e.g., start on amiodarone, propafenone) to convert atrial flutter to sinus rhythm or to maintain sinus rhythm Antithrombotic therapy: heparin, levonox, wafering Radiofrequency catheter ablation can be curative therapy for atrial flutter. Atrial Fibrillation Total disorganization of atrial electrical activity due to multiple ectopic foci, resulting in loss of effective atrial contraction Most common dysrhythmia Prevalence increases with age. During atrial fibrillation, the atrial rate may be as high as 350 to 600 beats/minute. P waves are replaced by chaotic, fibrillatory waves. Ventricular rate varies, and the rhythm is usually irregular. When the ventricular rate is between 60 and 100, it is atrial fibrillation with a controlled ventricular response. Atrial fibrillation with ventricular rate >100 is atrial fibrillation with a rapid ventricular response. Atrial fibrillation with ventricular rate <60 is atrial fibrillation with a slow ventricular response. The PR interval is not measurable, and the QRS complex usually has a normal shape and duration. At times, atrial flutter and atrial fibrillation may coexist. Results from abnormal impulse formation, causing rapid and disorganized and uncoordinated twitching of the atrial musculature in stead of the SA node. Clinical significance Can result in decrease in Cardiac output due to ineffective atrial contractions (loss of atrial kick) and rapid ventricular response Thrombi may form in the atria as a result of blood stasis. Embolus may develop and travel to the brain, causing a stroke Risk Factors Increasing age Hypertension Diabetes Obesity Valvular heart disease Obstructive sleep apnea Hyperthyroidism Cardiac ischemia CABAG: Coronary Artery Bypass Grafting (cardiology) Clinical associations: Usually occurs with underlying heart disease Rheumatic heart disease CAD Cardiomyopathy HF Pericarditis Treatment Goals o Decrease ventricular rate (control the rhythm!) o Prevent embolic stroke! Drugs for rate control: Digoxin, beta adrenergic blockers, calcium channel blockers Long-term anticoagulation: Coumadin Ventricular rate control is a priority for patients with atrial fibrillation. Sometimes converts on it’s own within 24-48 hours. For some patients, conversion to sinus rhythm may be considered. Antidysrhythmic drugs used for conversion: Amiodarone, propafenone (most effective if given within 7 days of onset) cardioversion may be used to convert atrial fibrillation to normal sinus rhythm. If patient has been in atrial fibrillation for >48 hours, anticoagulation therapy with warfarin (Coumadin) is recommended for 3 to 4 weeks before cardioversion and for 4 to 6 weeks after successful cardioversion. Amiodarone, propafenone, or sotalol may be given to help increase success with cardioversion and help maintain rhythm. Cholesterol-lowering drugs can be prescribed to prevent new-onset of atrial fibrillation. Dofetilide (EXAM) It can treat an irregular heartbeat (arrhythmia). Chest pain. facial or flaccid paralysis. numbness or tingling of the hands, feet, or face. paralysis. pounding, slow heartbeat. swelling of the ankles, arms, face, feet, fingers, legs, lips, tongue, or throat. troubled breathing. unexplained shortness of breath. Can cause QT prolongation Monitor in hospital for QT interval and renal function while they start the drug. Check 3 days, monitor EKG Prescribe beta-blockers for at least 24 hours prior to surgery to prevent A-fib post-op. *Do not stop meds on your own! Always consult the physician! Nursing malpractice: Understanding the risks! You know the 5-6 rights! Cardiac Ablation(atrial fibrillation) Therapies : Cryoablation & Radiofrequency Doctors perform cryoablation to restore normal heart rhythm by disabling heart cells that create an irregular heartbeat. During this minimally invasive procedure, a thin flexible tube called a balloon catheter is used to locate and freeze the heart tissue that triggers an irregular heartbeat. Anything to worry about? Potential stroke! Know the risk factors Test : how to identify stork: facial symmetric, how alert they are, speech, dropping, raise their hand, ECG Changes Associated With Acute Coronary Syndrome (ACS) Infarction Physiologic Q wave is the first negative deflection following the P wave. Small and narrow (<0.04 second in duration) Pathologic Q wave is deep and >0.03 second in duration. Worry about tissue damage?? Assessment Findings •Echocardiogram • • Walls of the heart, EF (ejection fraction; how well left article pump blood) Laboratory Tests • Troponin • Creatine Kinase and its isoenzymes • Myoglobin Rapid transit to the hospital (perfusion) 12-lead Labs Begin interventions O2, Nitroglycerin, Morphine, Aspirin, Beta-Blocker, Heparin, platelet inhibitors Reperfusion therapy if indicated (thrombolytic therapy, percutaneous coronary intervention) Evaluate for reperfusion Continue therapy: Plavix, IV heparin, Bed rest 12-24 hours, statin(cholesterol) as prescribed. Drugs used in thrombolytic therapy The most commonly used clot-busting drugs -- also known as thrombolytic agents -- include: Eminase (anistreplase) (risk for bleding) Retavase (reteplase) Streptase (streptokinase, kabikinase) t-PA (class of drugs that includes Activase) TNKase (tenecteplase) Abbokinase, Kinlytic (rokinase) Nursing Considerations Thromblolytic therapy: break down blood clots Catheterization Pulse distal to the site Premature Atrial Contraction/Complex Contraction originating from ectopic focus in atrium in location other than SA node Travels across atria by abnormal pathway, creating distorted P wave May be stopped, delayed, or conducted normally at the AV node Regular rhythm with occasional abnormal P. Clinical associations Can result from Emotional stress Use of caffeine, tobacco, alcohol Hypoxia Electrolyte imbalances COPD Valvular disease Treatment Depends on symptoms beta-adrenergic blockers may be used to decrease PACs. Reduce or eliminate caffeine. Paroxysmal Supraventricular Tachycardia (PSVT) • • • • • Originates in ectopic focus anywhere above bifurcation of bundle of His Run of repeated premature beats is initiated and is usually a PAC. Paroxysmal refers to an abrupt onset and termination. Some degree of AV block may be present. Can occur in presence of Wolff-Parkinson-White (WPW) syndrome ( Fig. 36-13. Paroxysmal supraventricular tachycardia (PSVT). Arrows indicate beginning and ending of PSVT. Clinical associations • In a normal heart o Overexertion o Emotional stress o Stimulants • Digitalis toxicity • Rheumatic heart disease • CAD • Cor pulmonale Clinical significance • Prolonged episode and HR >180 bpm may precipitate ↓ CO o Palpitations o Hypotension o Dyspnea o Angina Treatment • Vagal maneuvers: Valsalva, coughing • IV adenosine • If vagal maneuvers and/or drug therapy is ineffective and/or patient becomes hemodynamically unstable, DC cardioversion should be used. If PSVT recurs in patients with WPW, they may ultimately be treated with radiofrequency catheter ablation of the accessory pathway. Junctional Dysrhythmias Dysrhythmia that originates in area of AV node when AV become the pacemaker on heart. -(4060) P wave just before inverted QRS or hidden. Rhythm is regular SA node has failed to fire, or impulse has been blocked at the AV node. Fig. 36-15. Junctional escape rhythm. P wave is hidden in the QRS complex. Clinical associations • CAD • HF • Cardiomyopathy • Electrolyte imbalances • Inferior MI • Rheumatic heart disease • Drugs: Digoxin, amphetamines, caffeine, nicotine Clinical significance • Serves as safety mechanism when SA node has not been effective • Escape rhythms should not be suppressed. • If rhythms are rapid, may result in reduction of CO and HF Treatment • If symptomatic, atropine • Accelerated junctional rhythm and junctional tachycardia caused by digoxin toxicity; digoxin is held Treatment • Beta Adrenergic blockers, calcium channel blockers, and amiodarone used for rate control for junctional tachycardia not caused by digoxin toxicity • cardioversion is contraindicated. Conduction Abnormalities! First-Degree AV Block Every impulse is conducted to the ventricles, but duration of AV conduction is prolonged. • Clinical associations: Usually occurs with • MI • CAD • Rheumatic fever • Hyperthyroidism • Vagal stimulation • Drugs: Digoxin, -adrenergic blockers, calcium channel blockers, flecainide • Clinical significance • Usually asymptomatic • May be a precursor to higher degrees of AV block • Treatment • Check medications. • Continue to monitor. Second-Degree AV Block, Type 1 (Mobitz I, Wenckebach) • • • Gradual lengthening of the PR interval due to prolonged AV conduction time Atrial impulse is nonconducted, and a QRS complex is blocked (missing). Usually block occurs at AV node, but can occur in His-Purkinje system Fig. 36-16. Heart block. B, Second-degree AV block, type I, with progressive lengthening of the PR interval until a QRS complex is blocked. Clinical associations • -adrenergic blockers • May be associated with CAD and other diseases that can slow AV conduction Treatment • If symptomatic, atropine or a temporary pacemaker • If asymptomatic, monitor with a transcutaneous pacemaker on standby • Symptomatic bradycardia is more likely with one or more of the following: Hypotension, HF, shock. P wave is nonconducted without progressive antecedent PR lengthening. Usually occurs when a block in one of the bundle branches is present Second-Degree AV Block, Type 2 (Mobitz II) Fig. 36-16. Heart block. C, Second-degree AV block, type II, with constant PR intervals and variable blocked QRS complexes. Second-Degree AV Block, Type 2 (Mobitz II) • Clinical associations – Rheumatic heart disease – – – • CAD Anterior MI Digitalis toxicity Treatment – If symptomatic (e.g., hypotension, angina) before permanent pacemaker can be inserted, temporary transvenous or transcutaneous pacemaker – Permanent pacemaker Third-Degree AV Heart Block (Complete Heart Block) • Form of AV dissociation in which no impulses from the atria are conducted to the ventricles – Atria are stimulated and contract independently of the ventricles. – Ventricular rhythm is an escape rhythm. • Ectopic pacemaker may be above or below the bifurcation of the bundle of His. Clinical associations Severe heart disease: CAD, MI, myocarditis, cardiomyopathy Systemic diseases: Amyloidosis, scleroderma -adrenergic blockers, calcium channel blockers Treatment If symptomatic, transcutaneous pacemaker until a temporary transvenous pacemaker can be inserted Drugs (e.g., atropine (initial), epinephrine): Temporary measure to increase HR and support BP until temporary pacing is initiated Permanent pacemaker as soon as possible Pacemaker spike just before P wave Premature Ventricular Contraction Contraction originating in ectopic focus of the ventricles Premature occurrence of a wide and distorted QRS complex Multifocal, unifocal, ventricular bigeminy, ventricular trigeminy, couples, triplets, R-on-T phenomena Premature Ventricular Contraction (PVC’s) ● Wide and ugly complex ● Comes in different shapes and forms ● Premature occurred of a wide distorted QRS complex ● Contraction originating in ectopic focus of the ventricles ● Premature occurrence of a wide and distorted QRS complex Types of PVC’s ● Multifocal, unifocal ● Ventricular bigeminy : every other QRS ● ventricular trigeminy, ● couples, triplets, ● R-on-T phenomenon Clinical associations of PVC’s ● Stimulants: Caffeine, alcohol, nicotine, aminophylline, epinephrine, isoproterenol ■ Digoxin: check HR for 1 mins ■ Electrolyte imbalances ● Hypoxia ● Fever ● Disease states: MI, mitral valve prolapse, HF, CAD Clinical Significance of PVC’s ● In normal heart, usually benign ● Heart Disease: PVC’s may decrease CO and precipitate angina and HF ○ Monitor patient’s response to PVCs ○ PVCs often do not generate a sufficient ventricular contraction to result in a peripheral pulse. ○ Assess apical-radial pulse rate to determine if pulse deficit exists. ● Represents ventricular irritability ● May occur ○ After lysis of a coronary artery clot w/ thrombolytic therapy in acut MI reperfusion dysrhythmias ○ Following plaque reduction after percutaneous coronary intervention Treatment ● Based on cause of PVCs ○ Oxygen therapy for hypoxia ○ Electrolyte replacement ○ Drugs: -adrenergic blockers, procainamide, amiodarone, lidocaine Ventricular Tachycardia ● ● ● ● ● ● ● ● ● ● Run of three or more PVCs Monomorphic: one look the same, polymorphic, sustained, and nonsustained Considered life-threatening because of decreased CO and the possibility of deterioration to ventricular fibrillation QRS complex is more wider than normal Big wide and ugly Life threatening Rapid cardiac rate lightheadedness due to poor perfusion Lose consciousness This means there has been some damage to the ventricles Monomorphic: one looks the same Polymorphic: doesn’t all look the same. Is associated with electrolyte abnormalities or toxicities Ventricular Tachycardia (poly) Clinical associations of Ventricular Tachycardia ● MI ● CAD ● Electrolyte imbalances ● Cardiomyopathy ● Mitral valve prolapse ● Long QT syndrome ● Digitalis toxicity ● Central nervous system disorders Clinical Significance of Ventricular Tachycardia ● VT can be stable (patient has a pulse) or unstable (patient is pulseless). ○ Sustained VT: Severe decrease in CO ○ Hypotension ○ Pulmonary edema ○ Decreased cerebral blood flow ○ Cardiopulmonary arrest Treatment of Ventricular Tachycardia ● Precipitating causes must be identified and treated (e.g., hypoxia). ● Monomorphic VT ○ Hemodynamically stable (e.g., + pulse) + preserved LV function: IV procainamide, sotalol, amiodarone, or lidocaine ○ Hemodynamically unstable or poor LV function: IV amiodarone or lidocaine followed by cardioversion ● Polymorphic VT with a normal baseline QT interval: -adrenergic blockers, lidocaine, amiodarone, procainamide, or sotalol ○ Cardioversion is used if drug therapy is ineffective. ● Polymorphic VT with a prolonged baseline QT interval: IV magnesium, isoproterenol, phenytoin, lidocaine, or antitachycardia pacing ○ Drugs that prolong the QT interval should be discontinued. ○ If the rhythm is not converted, cardioversion may be needed ● VT without a pulse is a life-threatening situation. ○ Cardiopulmonary resuscitation (CPR) and rapid defibrillation ○ Epinephrine if defibrillation is unsuccessful Ventricular Fibrillation Clinical associations for Ventricular Fibrillation ● ● ● ● ● Acute MI, CAD, cardiomyopathy May occur during cardiac pacing or cardiac catheterization May occur with coronary reperfusion after fibrinolytic therapy ○ Accidental electric shock ○ Hyperkalemia ○ Hypoxia ○ Acidosis ○ Drug toxicity Unresponsive, pulseless, and apneic state (unconscious) If not treated rapidly, death will result (TEST: VF:more narrow and smaller, vfib is not as wide QRS as vtach) Treatment ● Immediate CPR and ACLS measures with use of defibrillation and definitive drug therapy Asystole ● ● ● ● Represents total absence of ventricular electrical activity No ventricular contraction (CO) occurs because depolarization does not occur. Most lethal dysrhythmia, no electrical activities in heart Can have occasional P but still asystole even if it has one P Clinical Associations Asystole ● Advanced cardiac disease ● Severe cardiac conduction system disturbance ● End-stage HF Clinical Si gnificance of Asystole ● Unresponsive, pulseless, and apneic state ● Prognosis for asystole is poor Treatment for Asystole ● CPR ● ACLS ○ Intubation ○ Transcutaneous pacing ○ IV therapy with epinephrine and atropine Pulseless Electrical Activity ● Electrical activity can be observed on the ECG, but no mechanical activity of the ventricles is evident, and the patient has no pulse. Pulseless Electrical Activity Clinical Associations ● Hypovolemia ● Hypoxia ● ● ● Metabolic acidosis Hyperkalemia or hypokalemia Hypothermia ○ Drug overdose ○ Cardiac tamponade ○ MI ○ Tension ○ Pneumothorax ○ Pulmonary embolus Treatment for Pulseless Electrical Activity ● CPR followed by intubation and IV epinephrine ● Atropine is used if the ventricular rate is slow. ● Treatment is directed toward correction of the underlying cause. Question #1: If you saw the rhythm below after defibrillation, how would you determine if it is pulseless electrical activity? Answer: Feel for the pulse. You can palpate the carotid for easiest access to pulse. Sudden Cardiac Death (SCD) ● ● Death from a cardiac cause Majority of SCDs result from ventricular dysrhythmias ○ V Tach ○ V Fib Defibrillation ● ● ● ● ● Most effective method of terminating VF and pulseless VT Passage of DC electrical shock through the heart to depolarize the cells of myocardium to allow the SA node to resume the role of pacemaker Deliver energy using a monophasic or biphasic waveform ○ Monophasic defibrillators deliver energy in one direction. ○ Biphasic defibrillators deliver energy in two directions. ■ Deliver successful shocks at lower energies and with fewer post shock ECG abnormalities Output is measured in joules or watts per second Recommended energy for initial shocks in defibrillators ○ Biphasic defibrillators: First and successive shocks: 150 to 200 joules ○ Monophasic defibrillators: Initial shock at 360 joules ● After the initial shock, chest compressions (CPR) should be started LifePak contains monitor, defibrillator, and transcutaneous pacemaker Synchronized Cardioversion ● ● Cardioversion Synchronized with QRS complex Choice of therapy for hemodynamically unstable ventricular or supraventricular tachydysrhythmias ○ Synchronized circuit delivers a countershock on the R wave of the QRS complex on the ECG The procedure for synchronized cardioversion is the same as for defibrillation with some exceptions. Synchronized cardioversion is shock delivery that is timed with the QRS complex. This synchronization avoids shock delivery during the relative refractory portion of the cardiac cycle, when a shock could produce ventricular fibrillation. The shock dose used for a synchronized shock is lower than that used for defibrillation. Cardioversion may be a necessary procedure when drugs alone have not been able to convert an arrhythmia to a normal heart rhythm. Cardioversion restores the normal heart rate and rhythm, allowing the heart to pump more effectively. The most common use of cardioversion is to treat atrial fibrillation or atrial flutter. But cardioversion may also be used to treat unstable supraventricular tachycardia, which could lead to ventricular fibrillation This is what will show on the monitor when cardioversion occurs Implantable Cardioverter-Defibrillator (ICD) ● ● ● ● ● Appropriate for patients who ○ Have survived SCA: sudden cardiac arrest ○ Have spontaneous sustained VT ○ Have syncope with inducible ventricular tachycardia/fibrillation ○ Are at high risk for future life-threatening dysrhythmias Consists of a lead system placed via subclavian vein to the endocardium Battery-powered pulse generator is implanted subcutaneously ICD sensing system monitors the HR and Rhythm and identifies VT or VF ○ Approxiamtely 25 seconds after detecting VT, or VF ICD <25 joules ○ If unsuccessful ICD recycles and delivers successive shocks ICD’s are equipped with antitachycardia and antibradycardia pacemakers ○ Initiate overdrive pacing of supraventricular and ventricular tachycardias ○ Provide backup pacing for bradydysrhythmias that may occur after defibrillation discharges ICD Education ● Variety of emotions are possible ○ Cardiac problems have high rate of depression ○ Fear of body image change ○ Fear of recurrent dysrhythmias ○ Expectation of pain with ICD discharge ○ Anxiety about going home ■ Participation in ICD support group should be encouraged Pacemakers ● Used to pace the heart when the normal conduction pathway is damaged or diseased ○ Pacing circuit consist of power source, one or more conduction leading, and the myocardium Pacemakers ● Only used if patient is symptomatic or if provider believes that they are at risk for lethal dysrhythmia ● Antibradycardia pacing ● Antitachycardia pacing: Delivery of a stimulus to the ventricle to terminate tachydysrhythmias ● Overdrive pacing: Pacing the atrium at rates of 200 to 500 impulses per minute to terminate atrial tachycardias ● Permanent pacemaker: Implanted totally within the body ● Cardiac resynchronization therapy (CRT): Pacing technique that resynchronizes the cardiac cycle by pacing both ventricles Pacemakers Power Source ● Temporary pacemaker: power source outside the body ○ Transvenous ○ Epicardial ○ Transcutaneous Temporary external, dual-chamber demand pacemaker ● Pacemaker Malfunction ● Failure to sense: Failure to recognize spontaneous atrial or ventricular activity and pacemaker fires inappropriately ○ Lead damage, battery failure, dislodgement of the electrode Failure to capture: Electrical charge to myocardium is insufficient to produce atrial or ventricular contraction ○ Lead damage, battery failure, dislodgement of the electrode, fibrosis at the electrode tip ○ Patient Education: need to check the pacemaker every 6 months or when they feel it is malfunctioning. Radiofrequency Catheter Ablation Therapy ● Electrode-tipped ablation catheter “burns” accessory pathways or ectopic sites in the atria, AV node, and ventricles. ○ Nonpharmacologic treatment for ■ AV nodal reentrant tachycardia ■ Reentrant tachycardia related to accessory bypass tracts ■ Control of ventricular response of certain tachydysrhythmias •Ablation therapy is done after EPS has identified the source of the dysrhythmia. ECG Changes Associated with Acute Coronary Syndrome (ACS) ● Ischemia ○ Changes occur in response to the electrical disturbance in myocardial cells due to inadequate supply of oxygen. ○ Once treated (adequate blood flow is restored), ECG changes resolve, and ECG returns to baseline. ○ This can be caused from a partial block or a complete block. ● Infarction ○ Physiologic Q wave is the first negative deflection following the P wave. ■ Small and narrow (<0.04 second in duration) ○ Pathologic Q wave is deep and >0.03 second in duration. Changes Associated With Injury ST segment, T wave, and Q wave changes associated with Myocardial injury (B). ECG Changes Associated With Acute Coronary Syndrome (ACS) ● Ischemia ○ ST segment depression and/or T wave inversion ○ ST segment depression is significant if it is at least 1 mm (one small box) below the isoelectric line. Fig. 36-29. ST segment, T wave, and Q wave changes associated with myocardial ischemia (A). ECG Changes Associated With Acute Coronary Syndrome (ACS) Injury ST segment elevation is significant if >1 mm above the isoelectric line. If treatment is prompt and effective, may avoid infarction o If serum cardiac markers are present, an ST-segment-elevation myocardial infarction (STEMI) has occurred. ECG Finding With Anterolateral Wall MI Fig. 36-30. ECG findings with anterolateral wall myocardial infarction. Normally, leads I, aVL, and V 1 to V3 have a positive R wave. Note the pathologic Q waves in these leads and the ST-segment-elevation in leads V2 to V5 (arrows). Non-Stemi Vs. Stemi - Stemi: we see ST elevation and troponin going up. Partial occlusion causing tissue death. Send straight to the cath lab. - Non-stemi: no ST elevation but troponin still going up. Send home with aspirin. They have to make lifestyle changes because they are at risk for stemi. Syncope ● ● Brief lapse in consciousness accompanied by a loss in postural tone (fainting) temporary loss of consciousness caused by a fall in blood pressure. Cardiovascular causes ○ Cardioneurogenic syncope or “vasovagal” syncope (e.g., carotid sinus sensitivity) ○ Primary cardiac dysrhythmias (e.g., tachycardias, bradycardias) ○ Going to the bathroom because of vagal pressure Syncope:Noncardiovascular causes ● Hypoglycemia ● Hysteria ● Unwitnessed seizure ● Stroke ● Vertebrobasilar transient ischemic attack Diagnostic Studies for syncope ● Echocardiography ● EPS ● Head-upright tilt table testing ● Holter monitor ● Event monitor/loop recorder Practice Questions 1. A patient in the coronary care unit develops ventricular fibrillation. The first action the nurse should take is to: a. Perform defibrillation. b. Initiate cardiopulmonary resuscitation. c. Prepare for synchronized cardioversion. d. Administer IV antidysrhythmic drugs per protocol 2. A patient has a diagnosis of acute myocardial infarction, and his cardiac rhythm is sinus bradycardia with six to eight premature ventricular contractions (PVCs) per minute. The pattern that the nurse recognizes as the most characteristic of PVCs is: a. An irregular rhythm. b. An inverted T wave. c. A wide, distorted QRS complex. d. An increasingly long PR interval. 3. A patient’s cardiac rhythm is sinus bradycardia with a heart rate of 34 beats/minute. If the bradycardia is symptomatic, the nurse would expect the patient to exhibit: a. Palpitations. b. Hypertension. c. Warm, flushed skin. d. Shortness of breath. Case Study A 45-year-old woman enters the ED complaining of sudden onset of palpitations and shortness of breath. ECG reveals atrial fibrillation with a rapid ventricular response (HR = 168). She has no previous history of cardiac problems. An emergent cardioversion is planned. 1. What are some teaching points before the procedure? a. It’s going to hurt b. Sedation will be given 2. What treatments are available if the procedure is unsuccessful? a. Beta blockers or calcium channel blockers b. Digoxin 3. What risks does sustained Afib pose and how can this information be helpful in ensuring compliance? a. Stroke





