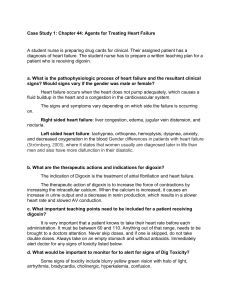
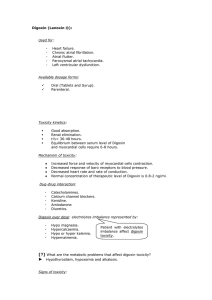
NR118 Care of the Adult Cardiac Drugs Information from Harding, et al (2020) or from Deonne Johnson, RN, MSN Class/Examples Indication Patient Teaching/Nursing Implications Short Acting Nitrates First line therapy for 1. Teach patient to keep from direct the treatment of sunlight. Nitrostat (Sublingual angina. Act to dilate 2. Place tablet or direct spray under NTG) peripheral blood tongue. May cause a tingling Nitrolingual vessels to decrease SVR sensation. If no tingling sensation (Translingual spray) which reduces cardiac occurs the drug may be ineffective. workload. 3. Call EMS if pain persists after 5 minutes. May take an additional 2 tablets while waiting on EMS to arrive. 4. NTG may cause increased HR, headache and dizziness. Patient can take acetaminophen for headache. 5. Caution patient not to stand up too quickly because hypotension may occur after NTG administration. 6. NTG may be taken prophylactically before activity known to precipitate chest pain. 7. Patient should report any changes in normal pattern or response of pain. 8. Replace the NTG tablets every 6 months because they lose potency once opened. Long-Acting Nitrates Used to reduce the 1. Predominant side effect is headache. incidence of chest pain. Headaches may diminish over time Isordil (Isosorbide even though the anti-angina effect dinitrate) remains. Imdur (isosorbide 2. Orthostatic hypotension is a mononitrate) problem with all nitrates. Nitroglycerin 3. Tolerance to NTG-induced Ointment vasodilation can develop, so patients Transdermal should schedule an 8 hour nitrateControlled-Release free period every day (preferably at Nitrates (patch) night). 4. Nurse should avoid getting the ointment or the medication from the patch on skin. 5. See implications for short acting nitrates. β-Adrenergic Blockers Inderal (propranolol) Lopressor (metoprolol) Corgard (nadolol) Tenormin (atenolol) Coreg (carvedilol) Bystolic (nebivolol) Calcium Channel Blockers Procardia (nifedipine) Calan (verapamil) Cardizem (diltiazem) Cardene (nicardipine) Preferred drugs for the management of chronic stable angina. Decrease myocardial contractility, HR, SVR and BP to reduce the myocardial oxygen demand. Also, have been shown to decrease morbidity and mortality in patients with CAD, especially following MI. May be used if βblockers are poorly tolerated, contraindicated or ineffective against angina pain. Also used to manage Prinzmetal’s angina pain. ACE Inhibitors Capoten (captopril) Vasotec (enalapril) Lotensin (benazepril) Prinvil, Zestril (lisinopril) ARBs (Angiotensin II Receptor Blockers) Cozaar (losartan) Diovan (valsartan) Benicar (olmesartan) PDE5 Inhibitors Cause systemic vasodilation (decreased SVR), decreased myocardial contractility, and coronary vasodilation. May be added to the drug regimen for certain high-risk patients with chronic stable angina. Used to treat high blood pressure (HTN) and Chronic Kidney Disease. Blocks the angiotensin 2 receptor sites so that sodium retention and vasoconstriction do not occur. Originally discovered during the search for 1. Sometimes are poorly tolerated d/t the side effects of bradycardia, hypotension, wheezing and GI complaints. 2. Should be avoided in patients with asthma, cautious use in patients with diabetes (mask signs of hypoglycemia. Should NOT BE DISCONTINUED ABRUPTLY without medical supervision. 1. Potentiate the action of digoxin. Digoxin levels should be closely monitored after starting this therapy. 2. Teach patient signs and symptoms of digoxin toxicity. (Bradycardia & dizziness or syncope, nausea & vomiting, visual disturbance) 3. Should be used with caution in patients with heart failure. 4. Avoid grapefruit while on nifedipine. 1. Can cause orthostatic hypotension. 2. Cough can be very bothersome and cause people to stop the medication. 3. Should not be used with potassiumsparing diuretics as hyperkalemia may result. 1. May cause dizziness, hyperkalemia, angioedema. 2. Problems such as severe diarrhea or weight loss should be reported to the PCP. 1. Because these medications are given for erectile dysfunction and act by Viagra (sildenafil) Cialis (tadalafil) Levitra (vardenafil) new anti-anginal medications. 2. Diruetics Loop Diuretic Lasix (furosemide) Thiazide Diuretic HCTZ(hydrochlorothiazide) Potassium-sparing Aldactone (spironolactone) Given to reduce or prevent fluid overload associated with cardiac failure. Anti-platelet Aggregation/Anticoagulant Aspirin Plavix (clopidogrel) Heparin Coumadin Given to prevent thrombus formation in at-risk clients. 1. 2. 3. 1. 2. 3. Anti-dysrhythmics Digoxin (lanoxin) Lidocaine Atropine Amiodarone Digoxin is given to slow and strengthen cardiac contractions. Given to control atrialfibrillation Lidocaine is given to control PVCs and prevent conversion to Ventricular Tachycardia or Ventricular Fibrillation. Acts to decrease ventricular irritability and excitability. Atropine is given to correct bradycardia or asystole. Amiodarone is used to 1. vasodilating the vessels of the penis, patients taking these drugs should not take nitrates. These drugs are being studied for the treatment of pulmonary hypertension. Watch for hypokalemia with the loop diuretics and thiazide diuretics. Patient may be on a potassium supplement if on the above medications. Watch patients for digoxin toxicity if on Lasix. Hypokalemia predisposes the patient to digoxin toxicity. Patients taking digoxin and Lasix should be on a potassium supplement. Daily ASA 81 mg often prescribed for post MI or in patients who are at risk. Heparin is administered following fibrinolytic (thrombolytic) therapy to prevent new clot formation. Coumadin prescribed long-term for uncontrolled atrial fibrillation to prevent clots caused by increased turbulence in blood flow. Digoxin: A) Teach patients to check pulse daily. Call provider if pulse falls below 60 bpm. B) Teach patient to recognize S/S of digoxin toxicity. C)Hospitalized clients on digoxin will have apical pulse daily prior to administration. 2. Lidocaine is administered via IV. It has been associated with malignant hyperthermia. 3. Atropine is administered via IV. It is a potent anticholinergic drug and a belladonna alkaloid. Used after epinephrine for asystole or pulseless electrical activity to restore NSR. (Anticholinergics cause increased heart rate, dry mouth, urinary retention, constipation and dilated pupils with blurred vision) treat life-threatening dysrhythmias of the ventricles (ventricular tachycardia or fibrillation). 4. The first dose of Amiodarone should be given in the hospital, and only used for people who have tried other anti-dysrhythmia medication.