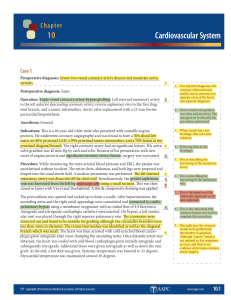
Case 1 Anesthesiologist: Deborah Doc, MD Dr. D placed a CVP in the internal jugular and a Swan-Ganz in the left internal jugular. Time: 15:37 to 17:51 Physical Status Modifier: P5 Preoperative Diagnosis: Severe coronary artery occlusive disease with failed stent insertion requiring emergency bypass grafting. Postoperative Diagnosis: Severe coronary artery occlusive disease with failed stent insertion requiring emergency bypass grafting. Name of Procedure: Emergency coronary artery bypass graft x2, (saphenous vein graft to proximal obtuse marginal circumflex, saphenous vein graft to distal right coronary artery). Anesthesia: General endotracheal anesthesia. Cardiopulmonary bypass was institutional. History: The patient is a 58-year old female with known peripheral vascular disease, who recently was found to have high-grade two vessel occlusive disease with an ostial 70 to 75 percent lesion of right coronary artery and a 90 percent mid body lesion of the proximal obtuse marginal branch of the circumflex. She came in and underwent attempted percutaneous transluminal coronary angioplasty with stent placement earlier today. Apparently, the lesion could not be crossed with a stent and she developed chest pain. The lesion was maintained with a wire across it. We were called to see the patient to perform emergency bypass grafting. After assessing the situation, we agreed to proceed. What ae the CPT and ICD-10-CM codes for this service?