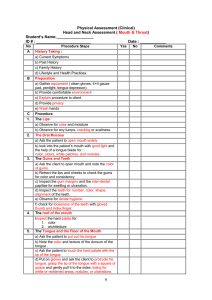
Assessing the Nose, Mouth, and Throat Supplies Tongue blades Pen light Nasal speculum Sterile gauze Clean gloves 1. Examine the external nose in four steps. (I will exam your nose) a. Inspect the nose. - Note its size, shape, color (straight, skin is smooth and unswollen, match color w/ face b. Observe the nares for discharge and flaring or narrowing. - Nares are oval shapes and columella is midline c. Palpate the bridge and soft tissues of the nose. - The nasal is firm and stable without tenderness, masses or bone d. Evaluate nasal patency. (When I block this nostril, try to breath in and out through the other). - Check the open naris, the breathing should be noiseless and easy Children under 7 age, fontal sinuses not develop yet, so focus on maxillary sinuses 2. Assess the nasal cavity. Observe three aspects. (Use 1 hand to move patient head, insert nasal speculum to inspect a. Inspect the nasal mucosa. – deep pink and glistening without discharge, masses b. Inspect the nasal septum. – have same color, firm and unswollen, septum have no perforation, bleeding, or crusting c. Test the sense of smell and CN I. 3. Examine the sinuses. a. Inspect the front and maxillary sinus areas – No swelling b. Palpate the frontal sinuses (press thumb against brow bone). Palpate the maxillary sinuses (zygomatic progresses). NO TENDERESS/SWELLING Examine the mouth, oral cavity, and oropharynx. 4. Inspect and palpate the lips – Pink, smooth, symmetric, without swelling, lesions, surface abnormalities 5. Have the patient clench the teeth and give a big smile. 6. Examine the buccal mucosa, gums, and teeth using four key assessments. (the upper molars should be interdigitate w. lower molar) Can you open your mouth, please a. Observe the mucous membrane. Inspect oral structure, using tongue blade and bright light b. Inspect the gums – appear slightly stipple and pink with clearly define tight margin at each tooth c. Palpate the gums – free of lesions, induration, thickening, masses, and tenderness d. Inspect and count the teeth. – using tongue blade to probe each tooth, which should be firmly anchored. NOTE ANY WEAR,NOTHCHES,CARIES,MISSING OR LOOSE TEETH Can you stick out your tongue and hold it please 7. Examine the oral cavity in seven ways. a. Inspect the dorsum of the tongue. – dull red, moist, and glistening, without coating or ulcerations, tongue should protrude fully, remain midline and show no deviation or tremor. b. Test CN XII. Now I need to look under your tongue. Can you touch the tip of your tongue to the top of your front teeth? c. Have the patient touch the tip of the tongue to the palate behind the upper incisors while you inspect the floor of the mouth and the ventral surface of the tongue – is pink and smooth with large veins between the frenulum and fimbriated folds, with no swelling or varicosities. OLDER PATIENT: varicose vein under the tongue are expected variation d. Inspect the lateral borders of the tongue (grab gauze around the tongue and pull the tongue to each side) – No red or white margins or ulcerations Now I going inside to feel your mouth e. Palpate the tongue and the floor of the mouth. – tongue feels smooth and even in texture, no nodules, ulcerations, or areas of induration Now I need to you tilt your head back and open wide so I can look at the roof of your mouth f. Inspect the palate and uvula. Now I need you to open line and say A g. Evaluate soft palate movement, (as patient vocalizes) – palate rise symmetrically and uvula should remain midline 8. Assess the oropharynx in three ways. a. Inspect the oropharynx and tonsillar pillars. b. Observe the posterior wall of pharynx (retropharyngeal wall). The tonsil should be pink as pharynx and should not project pass tonsillar pillar. retropharyngeal wall should pink, smooth with small vessels and spot of lymphatic tissue c. Touch the posterior wall of the pharynx on each side to elicit the gag reflex. The gag reflex should be present on both sides. Testing with a tongue blade on each side of the oropharynx is part of assessing the gag reflex. There should be a bilateral response to the gag reflex Assisting with Meals 1. 2. 3. 4. 5. Assess the patient for signs and symptoms of malnutrition, and identify if the patient is malnourished or at risk for malnutrition. Identify if the patient is at risk for dysphagia, and collaborate with other members of the health care team to minimize complications, such as aspiration pneumonia. Verify the health care provider's diet order, and ensure that the patient is receiving the correct therapeutic diet. Assess the patient's level of consciousness before feeding. If you suspect that the patient is aspirating, stop feeding the patient immediately, and suction the patient's airway. If the patient's intake falls below 75% for any length of time, refer the patient to a RD (registered dietitian) for medical nutrition therapy. Gather the necessary equipment and supplies. Perform hand hygiene before entering patients room Provide for the patient's privacy. Before feeding, Verify the health care provider's orders. Introduce yourself to the patient and family if present. (I’m Ngan, I will your nurse today, can check your wrist band) 6. Identify the patient using two identifiers. (Can you tell me your name and DOB) 7. Assess the patient for nausea, the ability to pass gas, and an intact gag reflex. (Ask patient have you feeling sick stomach, are you passing gas?) – should no nausea, can pass gas and gag reflex. the nurse want to determine if the patient is passing flatus before giving a meal to determine whether the GI tract is functioning. 8. Check the condition of the patient's teeth, or that dentures (if present) fit properly. (I need you to sip a small of water) 9. Check for bowel sounds in all four quadrants. 10. Assess the patient for the ability to feed himself/herself and what his/her appetite has been like. (Are you hungry? Are you able to feed yourself) - The nurse would ask the patient to try to self-feed in order to determine what specific assistance or assistive devices the patient needs during meals 11. Prepare the patient's room for mealtime: a. Clear the overbed table to make room for the meal tray. b. Help the patient into a comfortable sitting position in a chair, or place the patient's bed in the high-Fowler's position. If the patient is unable to sit, turn the patient onto his or her side, with the head of the bed elevated. 12. Prepare the patient for the meal: a. Help the patient with elimination needs, if necessary. b. Help the patient put in dentures and put on eyeglasses or insert contact lenses if used. c. Help the patient with hand hygiene. 13. Verify the meal is the patient's. 14. Ask the patient in what order he or she would like to eat the meal. Ask the patient about desired seasonings. Help the patient cut food into bite-size pieces if he or she is unable to do so independently. Patients with dementia may manage better with finger foods that may be easily picked up and put in their mouths as they may have difficulty using silverware.2 15. Use adaptive eating and drinking aids for the patient as needed, according to your assessment, such as a two-handled cup with lid, a plate with plate guard, utensils with splints, or utensils with oversized handles. 16. If the patient is disoriented, visually impaired, or easily fatigued, identify food placement by locating the food items as if the plate were a clock face. 17. If the patient needs assistance, feed the patient in a way that facilitates chewing and swallowing. a. For the older adult, provide small amounts of food at a time. Watch the patient bite, chew, and swallow, and be aware of his or her level of fatigue. Be sure the patient swallows the food between bites. b. For the neurologically impaired patient, provide small amounts of food at a time. Assess the patient's ability to chew, manipulate the tongue to form a bolus, and swallow. Check the patient's mouth for food left inside the cheeks, known as "pocketing." 18. Provide fluids as requested. Encourage the patient not to drink all of the liquid at the beginning of the meal. 19. Talk with the patient during the meal. Use the meal as an opportunity to educate the patient about topics such as those related to nutrition, postoperative exercises, and discharge planning. 20. Assist the patient with hand hygiene and mouth care after the meal has ended. 21. Ask the seated patient their preference for staying in the chair or being assisted into bed. 22. If the patient is still in bed, help the patient into a resting position, leaving the head of the bed elevated at 30 to 45 degrees for 30 to 60 minutes after the meal. To ensure the patient's safety, raise the appropriate number of side rails and lower the bed to the lowest position. 23. Place the call light within easy reach, and make sure the patient knows how to use it to summon assistance. 24. Return the patient's tray to the appropriate place, and perform hand hygiene. 25. Document the procedure in the patient’s record. If necessary, record the calorie count. If monitoring intake and output (I&O), record the fluid intake. Document any swallowing difficulties or refusal to eat. Cleaning Dentures 1. 2. 3. 4. 5. Verify the health care provider’s orders. Gather the necessary equipment and supplies. Provide for the patient’s privacy and perform hand hygiene. Introduce yourself to the patient and family, if present. Identify the patient using two identifiers, Compare these identifiers with the information on the patient’s identification bracelet. 6. Explain the procedure to the patient and ensure that he or she agrees to treatment. 7. Before cleaning a patient’s dentures, determine if the patient can clean the dentures independently, or if he or she requires assistance. Ask the patient about denture care product preference. 8. Apply gloves. 9. Remove the dentures from the patient’s mouth. If the patient is unable to do this independently, grasp the upper plate at the front with your thumb and index finger wrapped in gauze, and pull downward. Gently lift the lower denture from the jaw, and rotate one side of the bottom denture downward to remove it from the patient’s mouth. 10. Place the dentures in a denture cup or an emesis basin. Place a washcloth at the bottom of the sink, and fill the sink with approximately 1 inch (2.5 cm) of water. 11. Apply a cleaning agent to a toothbrush, and brush the surfaces of the dentures. 12. Hold the dentures close to the water. Hold the brush horizontally, and use a back-and-forth motion to cleanse the biting surfaces. To clean the outer tooth surfaces, use short strokes, moving from the top of the denture to the biting surfaces. To clean the inner tooth surfaces, hold the brush vertically and use short strokes. To clean the undersurface of the denture, hold the brush horizontally and use a back-and-forth motion. 13. Rinse the denture thoroughly in tepid water. If the water is too cold, the denture can crack. If the water is too hot, the denture can warp and will no longer fit properly in the patient’s mouth. 14. Repeat the cleaning and rinsing process with the other denture if the patient has one. 15. Offer mouthwash for the patient to rinse his or her mouth to clean the oral cavity prior to inserting clean dentures. A 50/50 solution of mouthwash and water or other antimicrobial solution may be used. The gums may be cleaned with a small amount of toothpaste applied to a soft-bristled toothbrush. 16. If the patient needs help inserting the dentures, moisten the upper denture and press it firmly to the gums to seal it in place. Use the same process to insert the moistened lower denture. 17. Some patients use an adhesive to seal the dentures in place. If the patient uses an adhesive, apply a thin layer to the undersurface of the denture before insertion. 18. Ask the patient if the denture(s) feel(s) comfortable. Assist the patient with drying his or her face. 19. Dispose of all used supplies and equipment. 20. Remove and dispose of gloves. Perform hand hygiene. 21. Some patients prefer to store their dentures, to give their gums a rest and to reduce the risk of infection. Store the dentures in tepid water in a denture cup. An effervescent cleaning tablet may be added to the cup at the patient’s request. Label the cup with the patient’s name, and put it in a secure place to keep the dentures from getting lost or being accidentally thrown away. 22. Help the patient into a comfortable position, and place toiletries and personal items within reach. 23. Place the call light within easy reach, and make sure the patient knows how to use it to summon assistance. 24. To ensure the patient’s safety, raise the appropriate number of side rails and lower the bed to the lowest position. 25. Document and report the patient’s response and expected or unexpected outcomes. Performing Oral Hygiene for an Unconscious Patient If the patient has an impaired gag reflex, determine the type of suction apparatus needed at the bedside to protect the airway from aspiration. Use Standard Precautions when providing oral care, including wearing clean gloves. Additional precautions requiring other personal protective equipment (PPE) may be necessary, depending on the patient’s condition. Do not use your fingers to inspect the mouth of an unconscious or unresponsive patient. Always use a tongue blade to avoid the patient’s reflex to bite down. 1. Introduce yourself to the patient and family, if present, and explain the procedure. If patient is conscious, ensure he or she agrees to treatment. 2. Identify the patient using two identifiers 3. Perform hand hygiene. 4. Provide for patient privacy. 5. Place a towel on the overbed table, and arrange your equipment. 6. Raise the bed to a comfortable working height, and position the patient close to the side of the bed from which you will be working. Lower the side rails. 7. Apply clean gloves. Assessment 8. Test for the presence of a gag reflex by placing a tongue blade on the back half of the tongue. Use a tongue blade and penlight to inspect the condition of the oral cavity. 9. Inspect the patient’s mouth for signs of tartar, swollen or bleeding gums, ulcerations, debris, and severe halitosis. Remove the patient’s dentures or partial plates if present, and safely store them for proper cleaning in an appropriate container labeled with the patient’s name. 10. Remove and dispose of gloves. 11. If needed, turn on the suction machine, and test the suction catheter. 12. Position the patient close to the side of the bed from which you will be working. Unless contraindicated, as in patients with head injury or neck trauma, position the patient in the Sims’ or side-lying position (reducing the risk of aspiration). Turn the patient’s head toward the mattress in a dependent position, with the head of the bed elevated to at least 30 degrees. 13. Turn the patient’s head toward the mattress in a dependent position, and place a towel under the patient’s head. Verify the head of the bed elevated to at least 30 degrees. 14. Apply a clean pair of gloves. 15. Place an emesis basin under the patient’s chin. 16. If the patient is unconscious or has a bite reflex, put an oral airway in place. Insert the airway upside down, and then turn it sideways and over the tongue to keep the teeth apart. Do not use force. 17. If possible, use floss or another interdental device (soft pick) at least once a day before brushing the teeth.4 18. Next, suction any accumulated secretions, and clean the mouth using a toothbrush moistened with water. Apply toothpaste or an antimicrobial or chlorhexidine solution to the toothbrush, and use it to loosen any crusts. 19. Apply toothpaste to the toothbrush, and cleanse the tooth surfaces using a gentle up-and-down motion. A toothette sponge can be used for patients in whom toothbrushing is contraindicated. A tongue blade may be used to move the lips and cheek mucosa away from the teeth as you brush or clean. 20. Clean the chewing and inner surfaces of the teeth first. Then clean the outer surfaces by holding the toothbrush so that its bristles are at a 45-degree angle to the gum line.2 Be sure that the tips of the bristles rest against and penetrate beneath the gum line.2 21. Brush the inner and outer surfaces of the upper and lower teeth from the gum line to the crown of each tooth. Clean the biting surfaces of the teeth by holding the toothbrush bristles perpendicular to the teeth and brushing gently back and forth. Brush the sides of the teeth by gently moving the bristles back and forth. 22. Use a bulb syringe filled with water to rinse the mouth and repeat as needed. Moisten the toothbrush with antimicrobial mouth rinse and cleanse the oral cavity, ensuring contact of the antimicrobial rinse with all oral cavity structures. Use the brush or a toothette to clean the roof of the mouth, the gums, and inside the cheeks. 23. Gently brush the tongue, taking care to avoid stimulating the gag reflex if one is present.2 Repeat this rinsing action several times, and use suction to remove any secretions. 24. If a toothbrush cannot be used, rinse the roof of the mouth, gums, and inside of the cheeks with a toothette sponge. 25. Use a gloved finger or toothette sponge to apply a thin layer of water-soluble moisturizer to the patient’s lips. 26. Inform the patient that the procedure has been completed. Return the patient to a comfortable and safe position. 27. Raise the side rails as appropriate, and return the bed to the locked and lowest position. 28. Dispose of all soiled linen in an appropriate receptacle. 29. Remove and discard your gloves, and perform hand hygiene. (hand washing) 30. Document the patient’s oral care. Performing Oropharyngeal Suctioning Be prepared to quickly reapply supplemental oxygen if the SpO2 level falls below the patient’s usual baseline or if respiratory distress develops during or at the end of suctioning. Keep the catheter in a nonairtight container, such as a brown paper bag or a plastic bag attached to a bed rail or in the suction canister area. Do not store the catheter where it will come into contact with secretions or excretions, which promote bacterial growth. Do not use a rigid suction device to reach beyond the oropharynx into the laryngopharynx; doing so will cause the patient to gag and possibly vomit, increasing the risk of aspiration, or it may cause the negative effects of vagal stimulation. 1. Apply a pulse oximeter and obtain the SpO2 reading. 2. Help the patient into a semi-Fowler's or sitting position. Raise the bed up and lower the nearest side rail to facilitate access to the patient. 3. Assess for signs that the patient may require suctioning such as restlessness, gurgling, drooling, ineffective coughing, gastric secretions, or vomit in the mouth. 4. Drape the patient’s neck and chest. 5. Apply clean gloves. Put on a mask, gown, or face shield if splashing is likely. 6. Fill a cup or basin with approximately 100 mL of sterile water or 0.9% sodium chloride solution. 7. Connect one end of the connecting tubing to the suction machine and turn on the suction. Set the vacuum regulator to the lowest setting appropriate for the thickness of the secretions.1 Then connect the other end of the tubing to the Yankauer suction catheter. 8. Check to ensure that the suction machine is functioning properly by placing the tip of the catheter in sterile water or sterile saline and suctioning a small amount from the cup or the basin. 9. Remove the patient’s oxygen mask, if present. Keep the oxygen mask near the patient’s face in case he or she desaturates. A nasal cannula may remain in place. 10. Insert the catheter into the patient’s mouth moving along the gum line to the pharynx. Move the catheter around the mouth until all secretions have cleared. Encourage the patient to cough. Do not at any time apply suction to the buccal mucosa. Clear the device by suctioning a small amount of sterile water or sterile normal saline in between passes. Replace the patient’s oxygen mask. 11. Rinse the catheter with water in a cup or basin until the connecting tubing has been cleared of secretions. Turn off the suction. Disinfect the external catheter surface per manufacturer’s directions. Wash the patient’s face if secretions are present on the patient’s skin. 12. Observe/assess the patient’s respiratory status. Repeat the procedure, if indicated. You may need to use a flexible suction catheter to reach into the pharynx if the patient’s respiratory status has not improved. 13. Remove the towel, cloth, or disposable drape from the patient, and place it in the trash or in the laundry if it is soiled. Raise the bedside rail and place the bed in the lowest position to the floor. Reposition the patient. The left lateral recumbent position encourages drainage and should be used if the patient has a decreased LOC. 14. Place the dry catheter in a clean, dry area, such as in a bag attached to the bedrail. 15. Position the recovered patient for comfort, and provide oral hygiene if needed. 16. Discard the remainder of the sterile water or sterile normal saline into the appropriate receptacle. Discard the disposable cup into the appropriate receptacle. 17. Remove your gloves and mask or face shield, and dispose of them in the appropriate receptacles. 18. Perform hand hygiene. 19. Help the patient into a comfortable position, and place toiletries and personal items within reach. 20. Place the call light within easy reach, and make sure the patient knows how to use it to summon assistance. 21. To ensure the patient’s safety, raise the appropriate number of side rails and lower the bed to the lowest position. 22. Perform hand hygiene. 23. Document and report the patient’s response and expected or unexpected outcomes. Document the procedure including how the patient tolerated the suctioning. Document the amount, consistency, color, and odor of any secretions. action is most useful in evaluating the effectiveness of oropharyngeal suctioning : Comparing presuctioning and postsuctioning assessment data allows the nurse to compare the patient’s postintervention respiratory status against his or her baseline to see if it has improved. After oropharyngeal suctioning, Placing the Yankauer catheter in a clean, dry area will protect it until it is needed again. Supplies are not disposed of in the trash, and the Yankauer tube can be used again. The supplies need not be placed in a biohazard bag. Taking Aspiration Precautions Assess the patient’s level of consciousness before feeding him or her. Identify obstructions and medication side effects that cause difficulty swallowing. Suspect dysphagia or aspiration if the patient complains of having the sensation of food sticking in the throat and makes repeated attempts to swallow. Place any patient at risk of dysphagia or aspiration on NPO status until a swallowing evaluation determines that the dysphagia poses no substantial risk to the patient. Comply with the mandate of The Joint Commission that any patient admitted with a stroke diagnosis be screened for aspiration before he or she ingests an oral diet. To evaluate for silent aspiration, use pulse oximetry when administering oral fluids. A drop in oxygen saturation of greater than or equal to 2% from the patient’s baseline is diagnostic of aspiration. The inability to coordinate the complex, sequential swallowing mechanism results in food being left in the mouth and may lead to failure to protect the airway. Aspiration pneumonia is a fatal complication of dysphagia, especially in older adults. Steps to start the procedure (hand hygiene, Introduce yourself, provide privacy, identify the patients, and explain the procedure) 1. Determine if the patient is at risk for aspiration: a. Assess nutritional status and ability to chew or swallow. b. Assess for mental status by seeing if the patient can follow simple commands. c. Apply gloves and inspect mouth and cheeks with penlight and tongue blade. Pocketing of food suggests patient has difficulty swallowing. d. Ask the patient to tuck chin at a 45-degree angle. Ask him or her to swallow twice or several times, and monitor the patient’s swallowing and any associated respiratory difficulty. 2. Position the patient at a 90-degree angle, or place at the most upright position the patient’s medical condition allows. 3. Apply the pulse oximeter to the patient’s finger (or other appropriate site) to monitor oxygenation during the feeding. 4. Watch the patient eat of various consistencies. Add a thickener to thin liquids to achieve the desired consistency, as determined by the health care provider or SLP’s evaluation. Always read the label when modifying liquids to prepare the proper thickness. 5. Encourage the patient to feed himself or herself. 6. Remind the patient not to tilt his or her head backward while eating or drinking. 7. If the patient is unable to feed himself or herself, direct ½ to 1 teaspoon of food into the unaffected side of the patient’s mouth, allowing the utensil to touch the mouth or tongue. 8. Offer verbal cues as you feed the patient. Remind him or her to focus on chewing and to think about swallowing. 9. If necessary, use sauces, condiments, and gravies to form a cohesive food bolus. 10. Avoid mixing foods that have different textures in the same mouthful. Alternate between offering liquids and giving bites of food. 11. Minimize distractions, and do not rush the patient. Allow plenty of time for him or her to adequately chew and swallow the food. 12. Monitor for any signs and symptoms of fatigue, dysphagia, or aspiration. 13. If needed, suction patient’s orapharyngeal airway and check mouth periodically with penlight to make sure patient is not pocketing food. 14. If coughing, choking, or other signs of aspiration occur, remove the tray until the patient is evaluated by the practitioner or speech therapist. 15. Ask the patient to remain sitting in the upright position for at least 30 to 60 minutes after the meal. 16. Remove pulse oximeter and help the patient with hand hygiene and oral hygiene after meals. 17. Perform hand hygiene. 18. Place toiletries and personal items within reach. 19. Place the call light within easy reach, and make sure the patient knows how to use it to summon assistance. 20. To ensure the patient’s safety, raise the appropriate number of side rails and lower the bed to the lowest position. 21. Report any signs or symptoms of dysphagia or aspiration to the health care provider. 22. Weigh the patient daily or weekly. Document intake and output (I&O), calorie intake, food intake, and pulse oximeter readings during meals. 23. Consult the health care provider about any modification of the patient’s diet. the nurse instruct nursing assistive personnel (NAP) to report while feeding any patient on aspiration precautions when the onset of coughing in any patient on aspiration precautions the most effective way of preventing aspiration is put any at-risk patient on NPO status until a dysphagia evaluation can be conducted by a SLP. Monitoring the patient’s oxygenation is useful in detecting silent aspiration; nevertheless, but not the most important precaution to prevent aspiration. Bedside observation, however, is insufficient. The most important precaution to prevent aspiration is to put any at-risk patient on NPO status until a dysphagia evaluation can be conducted by a SLP. food item would not be given to a patient on a dysphagia diet is chicken noodle soup. The liquid portion of the soup is not viscous enough to form a soft bolus in the mouth