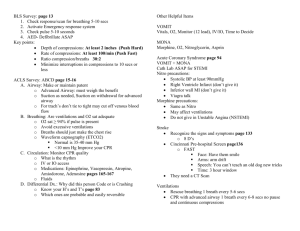
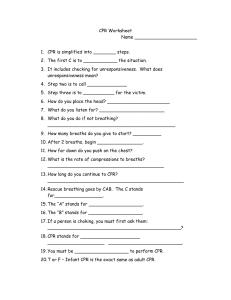
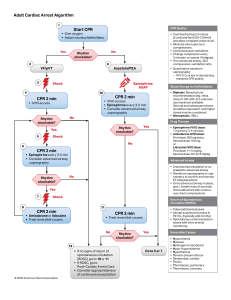
CODE BLUE QUICK SHEET: ACLS algorithm CPR 2 min → check pulse & rhythm Q2 min of CPR ⇣ SHOCK→ wait to see rhythm; NO MEDS yet ⇣ CPR 2 min → check pulse & rhythm Q2 min of CPR ⇣ SHOCK ⇣ GIve EPI = 1 mg Q 3-5 min IV push @ beginning of compressions (NOT with breaths) ⇣ SHOCK→ wait to see rhythm; NO MEDS yet ⇣ CPR 2 min ⇣ SHOCK ⇣ CPR ⇣ Amiodarone = 300 bolus 1st dose IV push, 150 2nd dose, NO 3rd dose. (Dilute in 20-30 ml D5W) (Should wait 15 min between doses) ⇣ **Hang whatever fixes pt heart** NOTE: You can only do all this for so long→ intubate pt CPR 30 compressions - 2 breaths - 30 compressions - 2 breaths Breathing/Circulation: ○ 1 breath/sec ○ Tight seal around mouth/nose -- stand at HOB, tilt head back, hold mask & chin w “C”-shaped hand ○ Give 15L of O2 (Ambu bag fully inflated) Compressions: ○ Hands middle @ nipple line ○ 2 inches deep; 100-120 per minute ○ Place backboard under pt Defibrillation/Cardioversion Pads can 1) cardiovert, 2) pace, 3) defibrillate **defibrillate IF pt is dead→ VTach/ VFib **cardiovert IF pt alive → Aflutter or symptomatic AFib ⇓ Then think: What needs fixed to keep this pt alive? Cardioverting→ converts to sinus rhythm from FAST rhythms OUTSIDE the ventricles. SHOCKS are delivered with R waves→ energy used to control RATE. SE: physically exhausting → give meds to relax (versed) ROSC: Return of Spontaneous Circulation 1. Maintain O2 saturation ≥94% via face mask HOB 30 deg Advanced Airway? 2. Treat HoTN (SBP <90mmHg) → IV bolus (1-2 L NS or LR) and vasopressor infusion (Epi, Dopamine, Norepi) - then focus on treatable causes that may have precipitated the cardiac arrest 3. 12-lead ECG - To identify pt’s w STEMI or high suspicion of AMI 4. Assess coronary reperfusion Initiate Temperature management (mild hypothermia is optimal for good neurological outcome) Neuro checks Airway ● NO oral airway if AWAKE→ gagging/aspiration risk ● Nasal trumpet CI for deviated septum or trauma pt ● PRIORITY: adjust head/neck position 1st ETT/Vents: used for 1. inability to maintain airway (LOC issue) and 2. oxygenation issues (lungs) →Sedate first (need order to sedate- restraint) → 10 cc syringe w air to inflate balloon (to keep air IN) → measure tube in cm @ gums or teeth → oral care to prevent VAP and infxn; bite block (tubing) *CHECK placement: (1) Auscultate stomach (2) base of L/R lungs (3) higher on lungs (4) physical rise of chest even? (5) check CO2 detector NO XRAY to verify (this is a DR thing) Code Blue Drugs ● Amiodarone→ use FILTER; no 3rd dose ● Adenosine→ FLUSH FAST; 12 lead EKG, used for chemical cardioversion ● Epi→ All pressors are compatible ● Atropine→ symptomatic brady (NOT CPR/code blue!) ● Lidocaine→ antiarrhythmic Pt may need LR to expand vasculature; (don’t have to flush line during med administration if giving fluids) During code → DOCUMENT (when did code start? Meds given? When? Dose? etc) ☆ Treat the PATIENT, not the monitor ☆