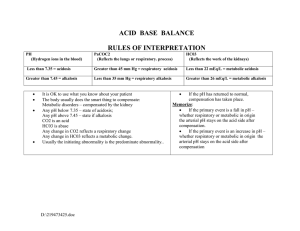
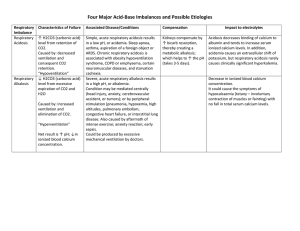
Acid-Base Disorders Worksheet Joshua Steinberg MD for Wilson Family Practice Residency Na+ Step #1: Gather the necessary data (Na+, Cl-, HCO3-, pH, pCO2). 1 Preferably, all obtained from the same blood sample. At Wilson, ordering an Cl HCO3ABG and a BMP (Chem 7) will give you all of the information you need. pH pCO2 Step #2: Look at the pH. If it is > 7.4, then pt has primary alkalosis, proceed to Step 3a. If pH < 7.4, then pt has primary acidosis, proceed to step 3b. Patient has primary: acidosis | alkalosis Step #3: Look at the pCO2. 3a: If PCO2 is > 40, then pt’s alkalosis is metabolic; if < 40 then respiratory. 3b: If PCO2 is > 40, then pt’s acidosis is respiratory; if < 40, then metabolic. Primary process is: respiratory | metabolic Step #4: Look for disorders revealed by failure of compensation. 2 - If 1° process is metabolic alkalosis, pCO2 should be > 40, < 55 (there are several Additional disorder: resp. resp. acidosis | alkalosis metabolic alkalosis pCO2 prediction formulas, but fraught with clinical inaccuracy/unreliability). - If 1° process is metabolic acidosis, predicted pCO2 = (1.5 x HCO3) + 8 +/- 2. In either case above, if actual pCO2 too high, then additional respiratory acidosis; if actual pCO2 too low, then additional respiratory alkalosis. - If 1° process is resp., then skip to steps 5&6 (where further metabolic disorders revealed). -or- no additional disorder Step #5: Check if patient has a significant anion gap (> 12-18). (AG = Na – Cl – HCO3.) If significantly elevated, then patient has an anion gap metabolic acidosis in addition to (or in confirmation of) whatever Steps 2 thru 4 yielded. Patient has | does not have anion gap metabolic acidosis. Step #6: Calculate the corrected bicarb. (Pt’s gap – 12 + pt’s serum bicarb) In addition to whatever disorders Steps 1 through 5 yielded, ... - if corrected bicarb > 30, then pt has an underlying metabolic alkalosis; - if corrected bicarb < 23, then pt has an underlying non-gap metabolic acidosis. Patient has underlying metabolic: non gap | alkalosis !!!!acidosis Step #7: Figure out what’s causing the problem(s) using differentials below & knowledge of the patient Anion Gap Metabolic Acidosis Non-Gap Metabolic Acidosis Acute Respiratory Acidosis Metabolic Alkalosis Respiratory Alkalosis “MUDPILERS” “HARDUPS” “CLEVER PD” “CHAMPS” • Methanol • Uremia • DKA/Alcoholic KA • Paraldehyde • Isoniazid • Lactic Acidosis • EtOH/Ethylene Glycol • Rhabdo/Renal Failure • Salicylates • Hyperalimentation • Acetazolamide • Renal Tubular Acidosis •Diarrhea •Uretero-Pelvic Shunt • Post-Hypocapnia • Spironolactone anything that causes hypoventilation, i.e.: • CNS Depression (drugs/CVA) • Airway Obstruction • Pneumonia • Pulmonary Edema • Hemo/Pneumothorax • Myopathy Contraction Licorice* Endo: (Conn’s/ anything that causes hyperventilation, i.e.: Cushing’s/Bartter’s)* • CNS disease • Hypoxia • Anxiety • Mech Ventilators • Progesterone • Salicylates/Sepsis (Chronic respiratory acidosis is caused by COPD and restrictive lung disease) Vomiting, NG suction Excess Alkali* Refeeding Alkalosis* Post-hypercapnia Diuretics* *assoc with high urine CL levels Step #8: Fix it! references: all steps but #4 nearly verbatim from Dr. Erik Rupard's worksheet adaptation of Haber, A practical approach to acid-base disorders. West J Med 1991. Aug; 155:146-151; step #4 from Narins and Emmett, Simple and Mixed Acid-Base Disorders. Medicine, vol. 59, no. 3, 1980, and multiple other sources agreeing on metabolic acidosis compensation while conflicting on metabolic alkalosis compensation! revised last: by Dr. Steinberg at Wilson/JCFCC January 11, 2009.