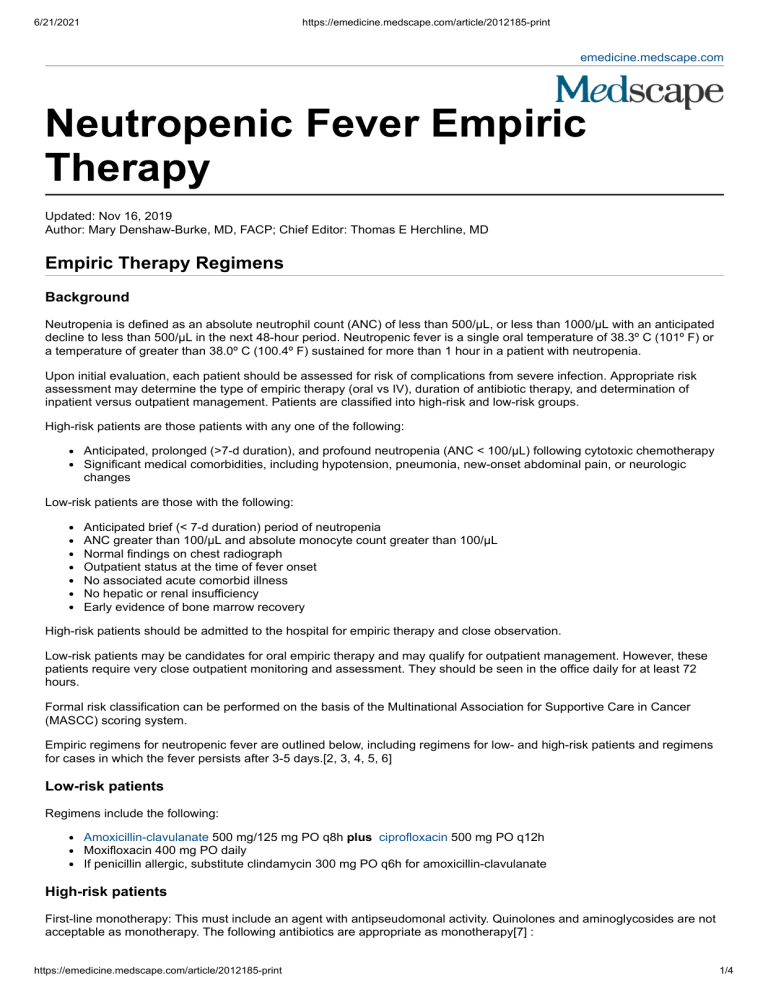
6/21/2021 https://emedicine.medscape.com/article/2012185-print emedicine.medscape.com Neutropenic Fever Empiric Therapy Updated: Nov 16, 2019 Author: Mary Denshaw-Burke, MD, FACP; Chief Editor: Thomas E Herchline, MD Empiric Therapy Regimens Background Neutropenia is defined as an absolute neutrophil count (ANC) of less than 500/µL, or less than 1000/µL with an anticipated decline to less than 500/µL in the next 48-hour period. Neutropenic fever is a single oral temperature of 38.3º C (101º F) or a temperature of greater than 38.0º C (100.4º F) sustained for more than 1 hour in a patient with neutropenia. Upon initial evaluation, each patient should be assessed for risk of complications from severe infection. Appropriate risk assessment may determine the type of empiric therapy (oral vs IV), duration of antibiotic therapy, and determination of inpatient versus outpatient management. Patients are classified into high-risk and low-risk groups. High-risk patients are those patients with any one of the following: Anticipated, prolonged (>7-d duration), and profound neutropenia (ANC < 100/µL) following cytotoxic chemotherapy Significant medical comorbidities, including hypotension, pneumonia, new-onset abdominal pain, or neurologic changes Low-risk patients are those with the following: Anticipated brief (< 7-d duration) period of neutropenia ANC greater than 100/µL and absolute monocyte count greater than 100/µL Normal findings on chest radiograph Outpatient status at the time of fever onset No associated acute comorbid illness No hepatic or renal insufficiency Early evidence of bone marrow recovery High-risk patients should be admitted to the hospital for empiric therapy and close observation. Low-risk patients may be candidates for oral empiric therapy and may qualify for outpatient management. However, these patients require very close outpatient monitoring and assessment. They should be seen in the office daily for at least 72 hours. Formal risk classification can be performed on the basis of the Multinational Association for Supportive Care in Cancer (MASCC) scoring system. Empiric regimens for neutropenic fever are outlined below, including regimens for low- and high-risk patients and regimens for cases in which the fever persists after 3-5 days.[2, 3, 4, 5, 6] Low-risk patients Regimens include the following: Amoxicillin-clavulanate 500 mg/125 mg PO q8h plus ciprofloxacin 500 mg PO q12h Moxifloxacin 400 mg PO daily If penicillin allergic, substitute clindamycin 300 mg PO q6h for amoxicillin-clavulanate High-risk patients First-line monotherapy: This must include an agent with antipseudomonal activity. Quinolones and aminoglycosides are not acceptable as monotherapy. The following antibiotics are appropriate as monotherapy[7] : https://emedicine.medscape.com/article/2012185-print 1/4 6/21/2021 https://emedicine.medscape.com/article/2012185-print Piperacillin-tazobactam 4.5 g IV q6h or Cefepime 2 g IV q8h or Meropenem 1 g IV q8h or Imipenem-cilastatin 500 mg IV q6h No single agent has shown superiority in the empiric treatment of febrile neutropenia. Second-line dual therapy: The use of dual therapy in high-risk patients is indicated for complicated cases (hypotension or pneumonia) or suspected or proven antimicrobial resistance. Appropriate antibiotic regimens in this setting include the following: Piperacillin-tazobactam 4.5 g IV q6h plus an aminoglycoside (see below) or Cefepime 2 g IV q8h plus an aminoglycoside (see below) or Meropenem 1 g IV q8h plus an aminoglycoside (see below) or Imipenem-cilastatin 500 mg IV q6h plus an aminoglycoside (see below) Aminoglycoside options: Gentamicin 2 mg/kg IV q8h or 5 mg/kg q24h or Amikacin 15 mg/kg/day or Tobramycin 2 mg/kg q8h Indications for the empiric addition of vancomycin (15 mg/kg IV q12h) to drug regimens listed above: Clinically suspected serious catheter-related infections (eg, bacteremia, cellulitis) Known colonization with penicillin- and cephalosporin-resistant pneumococci or methicillin-resistant Staphylococcus aureus (MRSA) Blood culture positive for gram-positive bacteria Hypotension Severe mucositis, if prior fluoroquinolone prophylaxis provided Additions to initial empiric therapy that may be considered for patients at risk for infection with antibiotic-resistant organisms: MRSA – Vancomycin, linezolid, or daptomycin Vancomycin-resistant enterococcus (VRE) – Linezolid or daptomycin Extended-spectrum beta-lactamase (ESBL)–producing gram-negative bacteria – A carbepenem (eg, meropenem) Carbapenemase-producing organisms (eg, Klebsiella pneumoniae carbapenemase) – polymyxin-colistin or tigecycline Recommendations if fever resolves in 3-5 days Organism identified: Adjust antibiotics based on specific organism and site of infection. Continue therapy for at least 7 days until cultures are negative and clinical recovery is noted. No organism identified and ANC greater than 500/µL for 2 consecutive days (see the Absolute Neutrophil Count calculator): Change therapy to amoxicillin-clavulanate 500 mg/125 mg PO q8h plus ciprofloxacin 500-750 mg PO q12h. Antibiotic therapy may be discontinued after 5-7 days once patient is afebrile for 2 consecutive days. No organism identified and ANC less than 500/µL: Continue current antibiotic regimen until day 7. If patient is initially low risk and clinically stable by day 7, then antibiotics can be discontinued. If patient is initially high risk then continue antibiotic therapy for 2 weeks or until resolution of neutropenia. Change to a prophylactic antibiotic regimen may be considered. If fever persists after 3-5 days: ANC greater than 500/µL: Continue current empiric antibiotic regimen. Stop regimen 4-5 days after ANC has reached >500/µL. Reassess for undiagnosed fungal infection. ANC less than 500/µL: If patient is not on vancomycin, add vancomycin if criteria are met. If patient is already on vancomycin, consider discontinuation if cultures are negative for MRSA. Consider adding empiric antifungal therapy (see below) https://emedicine.medscape.com/article/2012185-print 2/4 6/21/2021 https://emedicine.medscape.com/article/2012185-print Antifungal agents can be withheld in a specific subset of high-risk febrile neutropenic patients. These patients include those who remain febrile after 4-7 days of broad-spectrum antibiotics but are clinically stable and without clinical or radiographic signs of fungal infection. In low-risk patients, the risk of fungal infection is low; therefore, empiric antifungal agents should not be used routinely. Empiric antifungal therapy: Amphotericin B liposomal complex 3 mg/kg q24h or Voriconazole 6 mg/kg q12h X 2 doses, then 4 mg/kg q12 h or Posaconazole 200 mg PO q6h for 7d, then 400 mg PO q12h or Itraconazole 200 mg IV q12h for 2d, then 200 mg IV or PO q24h for 7d, then 400 mg PO q24h thereafter or Caspofungin 70 mg IV for 1 dose, then 50 mg IV q24h or Micafungin 100-150 mg IV q24h or Anidulafungin 200 mg IV for 1 dose, then 100 mg IV q24h Patients already on antifungal prophylaxis should be switched to a different class if fever persists. Continue therapy for 2 weeks if patient has stabilized and no infectious nidus is identified. Special considerations The prophylactic use of colony-stimulating factors has been shown to reduce the incidence of neutropenic fever and should be considered for patients in whom the anticipated risk of fever and neutropenia with a specific chemotherapy regimen is greater than 20%. If the intent of the chemotherapy treatment is palliative in nature, then chemotherapy dose reduction is usually a more appropriate approach. At present, the use of myeloid colony-stimulating factors is not recommended in the setting of an established fever and neutropenia. Several randomized studies have shown a decrease in the days of neutropenia, duration of fever, and length of hospital stay. However, none of those studies has shown a survival benefit.[8, 9] Contributor Information and Disclosures Author Mary Denshaw-Burke, MD, FACP Clinical Assistant Professor of Medicine, Jefferson Medical College of Thomas Jefferson University; Clinical Assistant Professor, Affiliated Clinical Faculty of the Lankenau Institute for Medical Research; Program Director of Hematology/Oncology Fellowship, Education Coordinator for Oncology, Lankenau Medical Center Mary Denshaw-Burke, MD, FACP is a member of the following medical societies: American College of Physicians Disclosure: Nothing to disclose. Coauthor(s) Aarti Shevade, MD Fellow in Hematology and Oncology, Lankenau Medical Center Aarti Shevade, MD is a member of the following medical societies: American Society of Hematology, American Society of Clinical Oncology Disclosure: Nothing to disclose. Specialty Editor Board Jasmeet Anand, PharmD, RPh Adjunct Instructor, University of Nebraska Medical Center College of Pharmacy; Editor-inChief, Medscape Drug Reference Disclosure: Nothing to disclose. Chief Editor Thomas E Herchline, MD Professor of Medicine, Wright State University, Boonshoft School of Medicine; Medical Consultant, Public Health, Dayton and Montgomery County (Ohio) Tuberculosis Clinic Thomas E Herchline, MD is a member of the following medical societies: Alpha Omega Alpha, Infectious Diseases Society of America, Infectious Diseases Society of Ohio Disclosure: Serve(d) as a speaker or a member of a speakers bureau for: Med Learning Group<br/>Received research grant from: Regeneron. Acknowledgements Kelley Struble, DO Fellow, Department of Infectious Diseases, University of Oklahoma College of Medicine https://emedicine.medscape.com/article/2012185-print 3/4 6/21/2021 https://emedicine.medscape.com/article/2012185-print Kelley Struble, DO is a member of the following medical societies: American College of Physicians and Infectious Diseases Society of America Disclosure: Nothing to disclose. References 1. Bow EJ, Rotstein C, Noskin GA, Laverdiere M, Schwarer AP, Segal BH. A randomized, open-label, multicenter comparative study of the efficacy and safety of piperacillin-tazobactam and cefepime for the empirical treatment of febrile neutropenic episodes in patients with hematologic malignancies. Clin Infect Dis. 2006 Aug 15. 43(4):447-59. [Medline]. 2. [Guideline] Taplitz RA, Kennedy EB, Bow EJ, Crews J, Gleason C, Hawley DK, et al. Outpatient Management of Fever and Neutropenia in Adults Treated for Malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America Clinical Practice Guideline Update. J Clin Oncol. 2018 May 10. 36 (14):1443-1453. [Medline]. [Full Text]. 3. Kern WV, Marchetti O, Drgona L, et al. Oral antibiotics for fever in low-risk neutropenic patients with cancer: a double-blind, randomized, multicenter trial comparing single daily moxifloxacin with twice daily ciprofloxacin plus amoxicillin/clavulanic acid combination therapy--EORTC infectious diseases group trial XV. J Clin Oncol. 2013 Mar 20. 31(9):1149-56. [Medline]. 4. Schuler U, Bammer S, Aulitzky WE, Binder C, Böhme A, Egerer G. Safety and efficacy of itraconazole compared to amphotericin B as empirical antifungal therapy for neutropenic fever in patients with haematological malignancy. Onkologie. 2007 Apr. 30(4):185-91. [Medline]. 5. Vedi A, Pennington V, O'Meara M, Stark K, Senner A, Hunstead P, et al. Management of fever and neutropenia in children with cancer. Support Care Cancer. 2015 Jul. 23 (7):2079-87. [Medline]. 6. Kroll AL, Corrigan PA, Patel S, Hawks KG. Evaluation of empiric antibiotic de-escalation in febrile neutropenia. J Oncol Pharm Pract. 2015 Jul 30. [Medline]. 7. [Guideline] Smith TJ, Bohlke K, Lyman GH, Carson KR, Crawford J, Cross SJ, et al. Recommendations for the Use of WBC Growth Factors: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2015 Oct 1. 33 (28):3199-212. [Medline]. [Full Text]. 8. Thursky KA, Worth LJ. Can mortality of cancer patients with fever and neutropenia be improved?. Curr Opin Infect Dis. 2015 Dec. 28 (6):505-13. [Medline]. https://emedicine.medscape.com/article/2012185-print 4/4