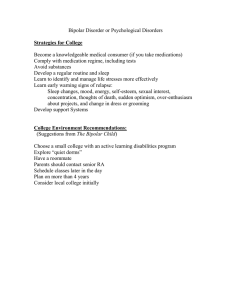
Bipolar, or manic-depressive, disorder is a frequent, severe, mostly recurrent mood disorder associated with great morbidity. The lifetime prevalence of bipolar disorder is 1.3 to 1.6%. The mortality rate of the disease is two to three times higher than that of the general population. About 10–20% of individuals with bipolar disorder take their own life, and nearly one third of patients admit to at least one suicide attempt. They range from mild hypomania or mild depression to severe forms of mania or depression accompanied by psychosis. Bipolar disorder is equally prevalent across genders, with the exception of rapid cycling, a severe and difficult to treat variant of the disorder, which arises mostly in women. Features of Mania: Features of Depression: Euphoria or irritable mood • Reduced interest in activities Decreased need for sleep • Behavior and demeanor different from usual Talkativeness • Reduced appetite and weight Racing thoughts • Insomnia ad fatigue Increased aggressive activity; • Suicidal thoughts If symptoms become too severe the person may need to be hospitalized About 50 percent of patients with bipolar illness have a family history of the disorder. The lifetime risk of bipolar disorder in first-degree relatives of a bipolar patient is 40–70% for a monozygotic twin and 5–10% for all other first-degree relatives. Many genes with small effect sizes are considered to contribute to the group of disorders. For example, a study in 2019 identified 30 significant loci, of which 20 had not previously been recognized (polygenic inheritance). Research is still ongoing on the exact genes that affect and cause bipolar disorder as well as how the brain is affected by these genetic variations. Bipolar disorder could be triggered by: Having a first-degree relative with bipolar disorder Periods of high stress Drugs or alcohol Although bipolar disorder may seem like a psychological disorder, it is believed to be caused by chemical imbalances in the brain that do not occur in the normal human. A series of many chemical process usually caused genetically may cause the person do have manic episodes, which can become severe and the patient diagnosed with bipolar disorder. Total: 123000 Research studies have shown that lithium, valproate, and carbamazepine have established efficiency in the treatment of acute mania and are effective in clinical practice as monotherapy for occasional episodes of mild mania. Bipolar depression (depressive episodes in a patient with bipolar illness) generally responds to tricyclic antidepressants. However, treatment for bipolar depression must be carried out in the knowledge that antidepressant drugs may induce a switch from depression to mania. Lithium is the classic mood stabilizer. It has been used for over 50 years as a treatment for bipolar disorder. However, the blood levels in patients taking lithium must be monitored as too much lithium can cause severe toxic effects and sometimes death. Bipolar, or manic-depressive, disorder is a frequent, severe, mostly recurrent mood disorder associated with great morbidity. The lifetime prevalence of bipolar disorder is 1.3 to 1.6%. The mortality rate of the disease is two to three times higher than that of the general population. About 10–20% of individuals with bipolar disorder take their own life, and nearly one third of patients admit to at least one suicide attempt. The clinical manifestations of the disease are exceptionally diverse. They range from mild hypomania or mild depression to severe forms of mania or depression. Lithium salts are the first choice long-term preventive treatment for bipolar disorder. They also possess well documented ant suicidal effects. Second choice prophylactic treatments are carbamazepine and valproate, although evidence of their effectiveness is weaker. Müller-Oerlinghausen, B., Berghöfer, A., & Bauer, M. (2002). Bipolar disorder. The Lancet, 359(9302), 241–247. https://www.sciencedirect.com/science/article/abs/pii/S0140673602074500 Belmaker, R. H. (2020). Bipolar Disorder. New England Journal of Medicine, 351(5), 476–486. https://www.nejm.org/doi/full/10.1056/NEJMra035354 Thank You