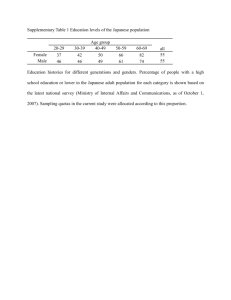
Review A Comprehensive Review of the Pharmacokinetics of Approved Therapeutic Monoclonal Antibodies in Japan: Are Japanese Phase I Studies Still Needed? The Journal of Clinical Pharmacology 54(5) 483–494 © 2014, The American College of Clinical Pharmacology DOI: 10.1002/jcph.231 Koji Chiba, PhD1,2, Hiroyuki Yoshitsugu, PhD3, Yuto Kyosaka, BSc2, Satofumi Iida, PhD4, Koichiro Yoneyama, MSc4, Takahiko Tanigawa, PhD5, Takashi Fukushima, BSc2†, and Masaki Hiraoka, PhD6 Abstract Ethnic evaluation of the pharmacokinetics and safety of new drugs is required in Japan before implementing bridging or joining global studies. As therapeutic monoclonal antibodies (mAbs) show limited ethnic differences, their pharmacokinetics and safety in Japanese individuals could be estimated from prior non‐Japanese studies. Therefore, there is potential to re‐evaluate the development program for mAbs in Japan. We reviewed the pharmacokinetics of mAbs approved in Japan. Although some differences had been observed in pharmacokinetics of mAbs between Japanese and non‐ Japanese populations (mainly Caucasians), these differences were attributed to differences of body weight and/or antigen levels. Moreover, the influential factors can be estimated without conducting regional pharmacokinetic/safety studies. The pharmacokinetics of some mAbs is presumably non‐linear and show differences between healthy volunteers and patients because of differences in antigen levels. However, for 10/24 mAbs approved in Japan, Japanese healthy volunteer studies were conducted before the patient studies. Additionally, for the mAbs that showed ethnic differences in pharmacokinetics, the doses selected in subsequent patient studies were the same as the doses approved in the United States. In this review, we discuss new drug development strategies in various regions, and assess the need for regional pharmacokinetics/safety studies before joining global studies. Keywords monoclonal antibody preparations, Japan, regulatory affairs The clinical trial environment in Japan has matured over the last decade, at least in part following the introduction of the International Conference on Harmonization Guidelines for Ethnic Factors in the Acceptability of Foreign Clinical Data (ICH‐E5, R1),1 and its adoption by the Pharmaceutical and Medical Devices Agency (PMDA).2 This guideline proposed that the similarity of pharmacokinetics between Japanese and non‐Japanese individuals should be evaluated before proceeding to bridging studies, which could be performed in a new region to extrapolate foreign clinical data to the population in the new region. The objective of this bridging approach is to minimize duplication of large clinical trials. The clinical trial environment in Japan was further revolutionized in 2007 by the recommendations of the Ministry of Health, Labour and Welfare (MHLW) for Japanese centers to participate in global clinical trials.3 As a consequence of these recommendations, the number of global clinical trials that have included Japanese clinical sites has markedly increased.4 To assess the feasibility of joining global clinical trials, possible ethnic differences between Japanese and non‐ Japanese subjects must be evaluated, as these may adversely influence the safety and efficacy of the new drug. Therefore, it is advocated that pharmacokinetic studies must be conducted in Japanese subjects before implementing bridging studies or joining global clinical trials. 1 Laboratory of Clinical Pharmacology, Yokohama College of Pharmacy, Yokohama, Japan 2 Department of Drug Development and Regulatory Science, Keio University Graduate School of Pharmaceutical Science, Tokyo, Japan 3 Discovery Medicine & Clinical Pharmacology, Research & Development, Bristol‐Myers Squibb, Princeton, NJ, USA 4 Clinical Research Planning Department, Chugai Pharmaceutical Co., Ltd., Tokyo, Japan 5 Clinical Sciences, Bayer Pharma AG, Berlin, Germany 6 DMCP, Clinical Research, Bristol‐Myers K.K., Tokyo, Japan *Present address: Clinical Pharmacology & PPDM, Japan Development, MSD K.K., Tokyo, Japan. y Present address: Site Management Department, Janssen Pharmaceutical K.K., Tokyo, Japan. Submitted for publication 26 September 2013; accepted 7 November 2013. Corresponding Author: Masaki Hiraoka, PhD, DMCP, Clinical Research, Bristol‐Myers K.K., Tokyo, Japan, Shinjuku i‐Land Tower 5‐1, Nishi‐Shinjuku 6‐chome, Shinjuku‐ku, Tokyo 163‐1328, Japan E‐mail: masaki.hiraoka@bms.com Ethnic Differences in the Pharmacokinetics of Monoclonal Antibodies Because of the large size, charge, polarity, and hydrophilicity of mAbs and the morphology of the paracellular pores in the vascular endothelium, the distribution of mAbs to peripheral tissue is limited and slow.5 Paracellular movement is thought to be the main route by which mAbs transfer from the vascular space to the interstitial space.6 Transcellular movement of mAbs by receptor‐mediated endocytosis, phagocytosis, and fluid‐phase pinocytosis mainly occurs in the vascular or interstitial space. Once the mAbs are incorporated into the cells, some of them enter the FcRn salvage pathway and are returned to the interstitial or vascular space. They may also return to the circulation via lymphatic drainage.7 Consequently, mAbs are mainly distributed in blood and interstitial spaces. From this biochemical perspective, mAbs are less likely to be sensitive to extrinsic or intrinsic ethnic factors compared with small chemical compounds.8,9 So far, there have been no reports describing ethnic differences, at least, in the paracellular movement of mAbs. Figure 1 shows the differences in clearance routes between large and small molecule drugs, including mAbs, Patients Internalization CDC ADCC Efficacy Toxicity Membrane associated target antigens Soluble target antigensa Catabolism Target mediated clearance Healthy volunteers Phagocytic cells FcRn Blood Enzyme Receptor Efficacy Toxicity Blood Kidney Toxicity Other organs Toxicity Liver Toxicity Hepatic clearance Monoclonal antibodies (Large molecule drugs) It is also important to consider whether ethnic differences in pharmacokinetics may translate into clinically meaningful differences in efficacy or safety. This issue raised the question of whether pharmacokinetic studies are necessary in the early phase of development for all drugs, or whether the need for such studies should be considered on a case‐by‐case basis, considering the characteristics of the target population (e.g., genetic mutational status and relative expression in different ethnic groups), as well as the expected absorption, distribution, metabolism, and excretion of the drug. Antibody drugs show several desirable characteristics, including good solubility and stability, long presence in the body, high selectivity and specificity, and low risk for bioconversion to toxic metabolites. Consequently, numerous monoclonal antibodies (mAbs) have been approved as therapeutic drugs and many mAbs are currently under clinical evaluation. Therefore, it is predicted that many mAbs will be introduced into the market. The primary objective of this review was to examine whether the characteristics of mAbs in non‐Japanese subjects, mainly Caucasians, could predict their pharmacokinetic characteristics in Japanese subjects, and whether a specific and abbreviated development strategy for mAbs in Japan could be considered. We expect that this regional investigation could be expanded and applied to Asian regulatory science. We included mAbs and mAb‐like therapeutic proteins, such as fusion proteins containing the Fc domain of IgG, in this review. The Journal of Clinical Pharmacology / Vol 54 No 5 (2014) Small molecule drugs 484 Renal clearance Figure 1. Clearance of small and large molecule drugs. The light blue‐ squared region represents the metabolism and disposition in healthy volunteers and patients. The yellow region indicates patient‐specific metabolism and disposition. The sections below and above the dotted line represent small molecule drugs and large molecule drugs (mAbs), respectively. Small molecule drugs are ubiquitously distributed and are mainly metabolized in the liver or eliminated by the kidney. The efficacy and toxicity of small molecule drugs are mediated by their interactions with enzymes, receptors, and other proteins in target tissues and in other organs. Large molecule drugs, including mAbs, are only distributed by the blood and are eliminated by target‐mediated clearance or phagocytosis. Because the target is highly expressed in patients, target‐mediated clearance is the predominant clearance route in patients. ADCC, antibody‐dependent cellular cytotoxicity; CDC, complement‐dependent cytotoxicity; PK, pharmacokinetics. aSome antibody drugs bind to endogenous substances. in healthy volunteers and patients. In terms of the metabolism of mAbs, the majority of the mAb dose is cleared by intracellular catabolism, through Fc‐receptor‐ mediated clearance and target‐mediated clearance.6 mAbs against soluble antigens are primarily eliminated by Fc receptor‐mediated clearance, which involves a non‐ specific common pathway for endogenous IgG and mAbs via FcRn and FcgR, a process that shows linear pharmacokinetics. Several reports have described ethnic differences in these pathways.10–13 For FcRn, genetic polymorphisms of FCGRT were reported to show ethnic differences, as the mean allelic frequency of the variable number of tandem repeats was 0.032 in Japanese individuals versus 0.075 in Caucasians.10 However, the impact of these genetic variations on the function of FcRn is yet to be established. For FcgR, although ethnic differences were reported in the frequencies of variants of FcgRIIa, FcgRIIb, FcgRIIIa, and FcgRIIIb,11–13 their effects on the clearance of mAbs remain unknown. The absence of ethnic differences of endogenous IgG in Fc receptor‐mediated clearance indicates the absence of ethnic differences in the elimination and clearance of mAbs because of the involvement of non‐specific common pathways. mAbs against antigens expressed on cell surfaces are eliminated by Fc receptor‐mediated and target‐mediated clearance pathways.14 Target‐mediated Chiba et al clearance primarily results from internalization of antigen–antibody immune complexes, which accelerates clearance in a saturable manner with non‐linear pharmacokinetics.9 However, this may not be observed in healthy volunteers because the expression or activation of the target may be lower in healthy volunteers than in patients. Consequently, the pharmacokinetic characteristics of efficacy‐ and toxicity‐related antigen–antibody interactions cannot be evaluated in healthy volunteers. Unlike mAbs, small molecule drugs are predominantly cleared via hepatic metabolism with biliary and renal excretion. Small molecule drugs are also capable of penetrating tissues more effectively than mAbs, which reflects physiological factors and the physicochemical properties of such drugs. However, the broad distribution of small molecule drugs contributes to their adverse reactions in non‐target tissues (Figure 1). Thus, ethnic differences in metabolic and physiological factors may result in ethnic differences in the pharmacokinetics and safety of small molecule drugs.15,16 However, this is not necessarily true for mAbs. From a pharmacokinetic perspective, Phase I studies in healthy volunteers in a new region might be meaningless for mAbs because of the absence of ethnic differences in their distribution and elimination, similar to that of endogenous IgG. These issues have therefore raised the question of whether or not clinical pharmacokinetic bridging studies are necessary for mAbs. Zhou et al5 compared the approved doses of 12 mAbs that were approved in both Japan and the US, and discussed the pharmacokinetic properties of mAbs in general. They reached the conclusion that, although there is a marked difference in body size between the two populations, this did not necessitate different dosing regimens in the two countries. They also highlighted the potential safety and ethical implications of clinically unnecessary administration of mAbs to healthy subjects, a major concern because of the large number of subjects that would be needed in such studies. They finally recommended that it “may be more prudent to first evaluate the available data sets looking for potential ethnic differences in the pharmacokinetic characteristics before considering the need to formerly conduct a clinical pharmacokinetic study.” Phase I Studies of Monoclonal Antibodies in Japan The PMDA answered a question regarding the necessity of Japanese Phase I studies before global clinical trials in a document published by the MHLW.3 The question was “Is it mandatory to have a Phase I trial or pharmacokinetic information in Japanese population prior to conduct of a global clinical trial for patients?” The PMDA’s answer to this question was: “The dosage regimen to be used in the global trial should be confirmed beforehand to whether it 485 does not have any particular safety problem for the Japanese. For this purpose, before the start of the global clinical trial, at least it is required to examine single‐dose safety and pharmacokinetics of investigational drugs in Japanese healthy volunteers or patients, compare the results with non‐Japanese, and confirm that risks in the Japanese are equivalent with non‐Japanese.” However, they also acknowledged the possibility of a waiver for conducting Japanese safety and pharmacokinetic studies “If safety in the Japanese can be determined with appropriate reasons, a Phase I trial in the Japanese is not necessarily required prior to the global trial.” To investigate whether or not Japanese Phase I studies had been conducted in Japan in addition to non‐Japanese Phase I studies, we searched the PMDA database (http:// www.info.pmda.go.jp/info/syounin_index.html) for mAbs that had been approved in Japan, and recorded the study population (healthy volunteers or patients) and the sampling type (intensive or sparse sampling). The 24 mAbs (including mAb‐like therapeutic proteins) that had been approved in Japan as of December 2012 are listed in Table 1. The pharmacokinetic properties in Japanese subjects were determined using intensive blood sampling in Japanese Phase I or Phase I/II studies for all mAbs, except for eculizumab, which was approved for an orphan indication with limited study data in Japanese subjects because of an extremely small patient population in Japan (approximately 400 patients in 1998). Most of the mAbs were approved for use in oncology (9/24, Table 1) or to treat inflammatory diseases, particularly rheumatoid arthritis (6/24). Phase I studies were conducted in healthy volunteers for 1/9 mAbs used to treat cancer and for 4/6 mAbs to treat rheumatoid arthritis. Thus, the subject types were probably chosen according to the target disease. Additionally, the same subject type had been selected in non‐Japanese studies for almost all mAbs used to treat cancer and rheumatoid arthritis. In other words, if a study of non‐Japanese healthy volunteers had not been conducted for a mAb, then one was not done in Japanese healthy volunteers. Almost all of the products were developed with either one of the following three strategies; bridging strategies, application of results in foreign clinical studies or using results from global studies including Japanese patients. Only tocilizumab and mogamulizumab underwent a full clinical development strategy in Japan as the NDAs for these mAbs were filed in Japan before other countries. There were no relationships between the clinical development strategies and subjects (i.e., inclusion of healthy volunteers or patients). Thus, according to current guidelines, almost all of the mAbs approved in Japan were evaluated in Japanese pharmacokinetic studies, even though pharmacokinetic data were available in non‐Japanese subjects. Moreover, for 10/24 mAbs, a Phase I study was performed in The Journal of Clinical Pharmacology / Vol 54 No 5 (2014) 486 Table 1. Therapeutic Target, Filing Strategy, and Type of Pharmacokinetic Studies Used to Support the New Drug Applications of Monoclonal Antibodies in Japan, as of December 2012 mAb Abatacept Adalimumab Basiliximab Therapeutic target Filing strategya 2010 2008 2010 2010 2010 2011 2012 2002 Rheumatoid arthritis Rheumatoid arthritis Plaque psoriasis, psoriatic arthritis Ankylosing spondylitis Crohn’s disease Polyarticular juvenile idiopathic arthritis Rheumatoid arthritis (first line) Prophylaxis of acute organ rejection in adult patients receiving renal transplantation Prophylaxis of acute organ rejection in pediatric patients receiving renal transplantation Advanced or recurrent colorectal cancer Advanced or recurrent colorectal cancer (additional dosing regimen) Advanced or recurrent non‐squamous non‐small cell lung cancer Breast cancer Cryopyrin‐associated periodic syndrome Rheumatoid arthritis (for patients with an inadequate response to conventional therapy) EGFR‐expressing advanced or recurrent colorectal cancer Bone metastases from solid tumors and multiple myeloma Paroxysmal nocturnal hemoglobinuria Rheumatoid arthritis (for patients who have an inadequate response to conventional therapy) Polyarticular juvenile idiopathic arthritis Rheumatoid arthritis (the prevention of structural joint damage) CD33 positive acute myeloid leukemia Rheumatoid arthritis Low‐grade B‐cell non‐Hodgkin’s lymphoma, mantle cell lymphoma Crohn’s disease Rheumatoid arthritis Intractable uveoretinitis Crohn’s disease (remission maintenance) Plaque asoriasis, psoriatic arthritis, pustular psoriasis, erythrodermic psoriasis Ankylosing spondylitis Ulcerative colitis CCR4‐positive adult T‐cell leukemia‐lymphoma Bronchial asthma Prevention of serious lower respiratory tract disease caused by RSV in children KRAS mutation‐positive colorectal cancer Neovascular (wet) age‐related macular degeneration Low‐grade or follicular, CD20‐positive, B‐cell non‐Hodgkin’s lymphoma, mantle cell lymphoma (375 mg/m2 weekly for 4 doses) CD20‐positive B‐cell non‐Hodgkin’s lymphoma new dosing regimen (375 mg/m2 weekly for 8 doses) Infusion prior to the administration of ibritumomab tiuxetan Chronic idiopathic thrombocytopenic purpura Castleman disease Rheumatoid arthritis Bridging study Bridging study Domestic study Intensive Intensive (HVe) Bridging study Intensive 2008 Bevacizumab 2007 2009 2009 Canakinumab Certolizumab pegol 2011 2011 2012 Cetuximab Denosumab Eculizumab Etanercept 2008 2012 2010 2005 2009 2012 Gemtuzumab ozogamicin Golimumab Ibritumomab tiuxetan 2005 2011 2008 Infliximab 2002 2003 2007 2007 2010 Mogamulizumab Omalizumab Palivizumab 2010 2010 2012 2009 2002 Panitumumab Ranibizumab Rituximab 2010 2009 2001 2003 Romiplostim Tocilizumab Pharmacokinetic blood sampling Approved 2008 2011 2005 2008 Bridging study Bridging study Bridging study Intensive Bridging study Bridging study Domestic study Domestic study Intensive (HV) Intensive (HV) Bridging study Global study Bridging study Bridging study Intensive Intensive (HV) Sparsef Intensive (HV) Bridging study Domestic study Bridging study Domestic study Bridging study Intensive Intensive (HV) Intensive Bridging study Bridging study Domestic study Intensive Domestic studyb Domestic study Bridging study Intensive Intensive (HV) Intensive (HV) Global study Bridging study —c Intensive Intensive Intensive Domestic study Domestic study Domestic study Domestic studyb Intensive (HV) Intensive (HV) (Continued) Chiba et al 487 Table 1. Continued mAb Trastuzumab Approved Therapeutic target 2008 Polyarticular juvenile idiopathic arthritis, systemic juvenile idiopathic arthritis Metastatic breast cancer whose tumors overexpress the HER2 protein (4mg/kg initially, followed by 2 mg every week) Breast cancer whose tumors overexpress the HER2 protein (adjuvant) Breast cancer whose tumors overexpress the HER2 protein (neoadjuvant) New dosing regimen for metastatic breast cancer whose tumors overexpress the HER2 protein (8 mg/kg initially, followed by 6 mg every 3 weeks) Gastric cancer whose tumors overexpress the HER2 protein Psoriatic arthritis, plaque psoriasis 2001 2008 2011 2011 Ustekinumab 2011 Filing strategya Bridging study Pharmacokinetic blood sampling Intensive Global study Special approvald Global study Domestic study Intensive CCR4, chemokine CC motif receptor 4; EGFR, endothelial growth factor receptor; HER2, human epidermal growth factor receptor 2; HV, healthy volunteers; RSV, respiratory syncytial virus. Including supplemental new drug applications. a Underlined “bridging” indicates no Japanese Phase III studies without description of extrapolation or bridging in the review report and non‐Japanese Phase III data are referred to as “essential data”; non‐underlined “bridging” represents mAbs for which review reports include “bridging” or “extrapolation.” b An independent Phase I study was conducted as a first‐in‐human study. c Unknown whether foreign data were essential or reference. d Public knowledge‐based application. e A Phase I study in healthy Japanese volunteers was discontinued at the lowest dosage because of the emergence of adverse events (infusion site reactions). f Orphan drug (only 400 patients in Japan). Japanese healthy volunteers even though data from Phase I studies in non‐Japanese subjects were available. From an ethical point of view, some guidelines might be necessary to help determine whether Japanese studies in healthy volunteers or patients with intensive sampling are necessary before Japanese patients are enrolled in global studies, if data from Phase I studies in non‐Japanese subjects are available. Evaluation of the Ethnic Differences of Pharmacokinetics in Japanese Subjects For some mAbs that show non‐linear PK due to target‐ mediated drug disposition, their clearance depends on the relative expression of the target antigen. Therefore, PK studies in healthy volunteers may not be appropriate. Exposure information was available for 7/10 mAbs, allowing comparison of the exposure between Japanese and non‐Japanese healthy volunteers. Figure 2 shows the differences in exposure and the PMDA’s assessment of the similarity of the mAbs in healthy volunteers and patients. Exposure (i.e., maximum plasma concentration [Cmax] and area under the concentration–time curve [AUC]) ratios (Japanese/non‐Japanese) in healthy volunteers ranged from 0.6 to 1.2, which might be numerically similar. Regarding studies in patients, data were available to compare the exposure between Japanese and non‐ Japanese subjects for 11/14 mAbs. The PMDA concluded that the pharmacokinetic profiles were similar for 8/11 mAbs. We calculated the Cmax and AUC (Figure 2A and B) ratios (Japanese/non‐Japanese subjects) for these 11 mAbs, and found that the ranges of the Cmax and AUC ratios for PMDA‐assessed “similarity” were 0.6–1.4 and 0.6–1.3, respectively. For cetuximab, although ethnic similarity of Cmax was suspected by the regulator for the 400 mg dose (1.35‐fold), the regulator carefully commented on the similarity in the expanded indication for head and neck cancer. Therefore, a 1.35‐fold difference might represent the regulator’s upper limit for assuming similarity. Only three mAbs had values beyond these ranges: ustekinumab (90 mg) (Cmax ratio: 1.56), rituximab (Cmax: 0.38, AUC: 0.42) and ibritumomab tiuxetan (AUC: 1.84). However, there were some exceptions, even within the range (basiliximab [20 mg] and ustekinumab [45 mg]). Table 2 lists the mAbs that the PMDA judged to be non‐similar in healthy volunteers and patients, along with the reason written in the common technical document (CTD) or PMDA review reports why the sponsors and the PMDA considered the pharmacokinetics to be “non‐ similar” (details in Supplemental Table S1). Despite the “non‐similar” evaluations of omalizumab, basiliximab (20 mg), ibritumomab tiuxetan, rituximab, and ustekinumab, their doses used in the subsequent The Journal of Clinical Pharmacology / Vol 54 No 5 (2014) 488 0.4 0.6 0.8 1 1.2 1.4 1.6 1.8 2 0.2 Palivizumab (3 mg/kg) Certolizumab pegol (400 mg) Etanercept (50 mg) Etanercept (25 mg) Denosumab (3 mg/kg) Etanercept (10 mg) Omalizumab (150 mg) Golimumab (100 mg) Denosumab (1 mg/kg) Rituximab (375 mg/m2) Abatacept (2 mg/kg) Infliximab (5 mg/kg, 10 mg/kg) Bevacizumab (10 mg/kg) Bevacizumab (15 mg/kg) Adalimumab (80 mg) Panitumumab (6 mg/kg) Abatacept (10 mg/kg) Adalimumab (40 mg) Ustekinumab (90 mg) Ustekinumab (45 mg) Cetuximab (250 mg/m2) Gemtuzumab ozogamicin (9 mg/m2) Cetuximab (400 mg/m2) Ibritumomab tiuxetan (14.8 MBq/Kg) Ibritumomab tiuxetan (11.1 MBq/Kg) Rituximab (375 mg/m2) Abatacept (2 mg/kg) 0.6 0.8 1 1.2 1.4 1.6 䕕Similar 䕔Non-similar Canakinumab (150 mg) Golimumab (50 mg) Adalimumab (80 mg) Panitumumab (6 mg/kg) Abatacept (10 mg/kg) Adalimumab (40 mg) Ustekinumab (90 mg) Ustekinumab (45 mg) Cetuximab (250 mg/m2) Gemtuzumab ozogamicin (9 mg/m2) Cetuximab (400 mg/m2) Patients Healthy volunteers Palivizumab (3 mg/kg) Certolizumab pegol (400 mg) Etanercept (50 mg) Etanercept (25 mg) Denosumab (3 mg/kg) Etanercept (10 mg) Omalizumab (150 mg) Golimumab (100 mg) Denosumab (1 mg/kg) Palivizumab (15 mg/kg) Canakinumab (150 mg) Golimumab (50 mg) 0.4 Basiliximab (20 mg) 0.4 0.6 0.8 1 1.2 1.4 1.6 1.8 2 AUC ratio 0.2 0.4 0.6 0.8 1 1.2 1.4 1.6 Cmax ratio Figure 2. Area under the concentration–time curve (AUC) ratios (left panel) and maximum plasma concentration (Cmax) ratios (right panel) for monoclonal antibodies (mAbs) between Japanese and non‐Japanese subjects. Upper and lower figures expressed for healthy volunteers and patients, respectively. Underlined mAbs target cell surface antigens; mAbs without underlining target soluble antigens. The data were extracted from the studies in which the pharmacokinetic properties were compared between Japanese and non‐Japanese subjects as of December 2012. If multiple mean values were reported for the same dose, the overall weighted geometric mean was calculated. If the PMDA clearly concluded that there was an ethnic difference in the pharmacokinetics profiles or if the PMDA agreed or did not deny an apparent/statistically significant ethnic difference in pharmacokinetic properties reported in the common technical documents (CTDs), the pharmacokinetics characteristics were reported as “non‐similar” (black columns), otherwise they were reported as “similar” (white columns). The dashed lines represent the upper and lower bounds of similarity. Eculizumab is not listed because the Cmax and AUC values were not reported for pharmacokinetic comparisons in the review report or CTD but the ratio of CL was 1.17. Ranibizumab, trastuzumab, tocilizumab, romiplostim, and mogamulizumab are not listed because no pharmacokinetic data were available for the comparison or the pharmacokinetics were non‐linear. clinical studies in Japan were the same as those stated on the approved US labels, and the dose regimens stated on the US and Japan labels are essentially similar (Table 2). The regulatory assessment for omalizumab, basiliximab, and usutekinumab was “non‐similar,” even though there were small numerical differences in pharmacokinetic parameters (Figure 2). For omalizumab, we could not find any pharmacokinetic factors that could account for the “non‐similar” evaluation. For basiliximab, there were no ethnic differences in Cmax, while differences in Vss and CL were explained by body weight. For ustekinumab (45 mg), the regulatory assessment was possibly influenced by the results reported for ustekinumab (90 mg), for which there was an apparent ethnic difference in Cmax. For the three mAbs that had values beyond the ranges of “similarity” (Cmax 0.6–1.4, AUC 0.6–1.3), ibritumomab tiuxetan and rituximab both target cell‐surface antigens, which influences mAb clearance. By contrast, ustekinumab targets a soluble antigen, which hardly affects mAb clearance. The ethnic differences in the pharmacokinetics of ibritumomab tiuxetan and rituximab were explained by CD20 levels. Ethnic differences in cell surface expression of the molecular targets of rituximab and ibritumomab tiuxetan could affect their exposure because the pharmacokinetics of mAbs are associated with the immune complex concentration. For ustekinumab, the NDA review report described that the difference in its pharmacokinetics could be explained by body weight. In fact, the Cmax, which was affected by distribution volume, showed ethnic differences whereas AUC did not. In summary, the observed differences in pharmacokinetics between Japanese and non‐Japanese were either due to differences in body weight or differences in receptor expression between the populations. The body weight difference between Japanese and Caucasian individuals is only about 20%,16 but the difference in receptor expression level depends on the target disease. If the difference is covered by the safety margin, dose adjustment might not be necessary, as was observed for clinical dose shown in Table 2. Safety of Monoclonal Antibodies in Healthy Volunteers As the pharmacokinetics of mAbs are similar between Japanese and non‐Japanese subjects, and because the target is usually less detectable in healthy volunteers than in patients, the safety profiles of mAbs in healthy volunteers should also be similar between Japanese and non‐Japanese subjects. Table 3 summarizes the adverse 45 mg initially and 4 weeks later, followed by 45 mg every 12 weeks (body weight 100 kg) 90 mg initially and 4 weeks later, followed by 90 mg every 12 weeks (body weight >100 kg) 150–375 mg every 2 or 4 weeks (adjustment by IgE and body weight) First 20 mg within 2 h before transplantation, followed by 20 mg at 4 days after transplantation 14.8 MBq/kg for patients with normal platelet count 11.1 MBq/kg for patients with platelet count of 100,000–149,000 cells/ mm3 375 mg/m2 weekly for 4 or 8 doses Non‐Japanese 20 mg 14.8 MBq/kg 11.1 MBq/kg 375 mg/m2 20 mg (patients) 14.8 MBq/kg (patients) 11.1 MBq/kg (patients) 375 mg/m2 (patients) 45 mg (patients) 90 mg (patients) No difference No difference 45 mg initially and 4 weeks later, followed by 45 mg every 12 weeks For patients who have an incomplete response, 90 mg every 12 weeks (similar regimen)g 90 mg 45 mg 150–375 mg every 2 or 4 weeks Subsequent phases in patientse 150 mg (healthy volunteers) Pharmacokinetic study phasesd 75–375 mg every 2 or 4 weeks (adjustment by IgE and body weight)f No difference Japanese Dose 1.84 —h 1.56 1.2 1.05 1.12 0.42 1.48 —h 0.38 —h 0.94 AUC 1.09 1.17 Cmax Ratiob Sponsor Non‐similar: it is probably caused by differences in CD20 expression Non‐similar: caused by differences in body weight Non‐similar: caused by differences in CD20 expression Non‐similar: the reason proposed by the sponsor was accepted Non‐similar: the cause of the difference was not determined Non‐similar: the cause of the difference was not determined Non‐similar: the cause of the difference was not determined Non‐similar: it is difficult to confirm similarity Regulator Assessment of similarityc Non‐similar: caused by IgE concentration difference Non‐similar: caused by differences in body weight AUC, area under the concentration–time curve; Cmax, maximum plasma concentration; mAb, monoclonal antibody. The mAbs included in this table are evaluated as “non‐similar” in PMDA review reports as of December 2012 (see legends in Figure 2). a Dose regimens stated on the US and Japanese labels. b Cmax ratios and AUC ratios between Japanese and non‐Japanese subjects described in Figure 2. c The assessments of similarity are described based on the CTD (sponsor evaluation) and the PMDA review report (PMDA evaluation). d Dose in the pharmacokinetic studies used to compare pharmacokinetic properties. e Doses used in subsequent clinical studies, which were conducted after the pharmacokinetic studies. f Dose adjustments based on the patient’s bodyweight and IgE concentration were recommended by the PMDA. g Body weight‐tiered dose regimens were not recommended by the PMDA because of the small number of patients with a body weight >100 kg in Japanese clinical trials. h Not reported. Ustekinumab Rituximab Ibritumomab tiuxetan Basiliximab Omalizumab mAb Recommended dosea Table 2. Relationship Between the Dose Used in Pharmacokinetic Studies and Doses Used in Subsequent Clinical Studies for mAbs Evaluated as being “Non‐Similar,” as of December 2012 Chiba et al 489 The Journal of Clinical Pharmacology / Vol 54 No 5 (2014) 490 Table 3. Summary of Adverse Reactions Associated With Monoclonal Antibodies in Healthy Japanese Volunteers, as of December 2012 mAb Adalimumab Canakinumab Dose 0.1 mg/kg 1 mg/kg i.v. 3 mg/kg i.v. 600 mg i.v. 150 mg s.c. 300 mg s.c. 600 mg i.v. þ 300 mg s.c. Placebo Certolizumab pegol 100 mg 400 mg 800 mg Placebo Denosmab 0.03 mg/kg 0.1 mg/kg 0.3 mg/kg 1.0 mg/kg 3.0 mg/kg Placebo Etanercept 10 mg 25 mg Golimumab 50 mg placebo 50 mg 100 mg All adverse event (number of patients) Rash (7/15), leukopenia (1/15) Laboratory test abnormal (2/6), injury, poisoning and procedural complications (1/6) Gastrointestinal disorders (2/6), infections and infestations (1/6) None Gastrointestinal disorders (2/6), infections and infestations (1/6) Laboratory test abnormal (4/6) Laboratory test abnormal (2/6), eye disorders (1/6) Laboratory test abnormal (7/12), infections and infestations (2/12), gastrointestinal disorders (2/12) Queasy (1/6), nasopharyngitis (1/6) Nasopharyngitis (1/6), chickenpox (2/6), headache NOS (2/6) Queasy (2/6), sore throat NOS (2/6), influenza like illness (1/6), nasopharyngitis (2/6), back pain (2/6), headache NOS (3/6) Sore throat NOS (1/6), Injection site pain (2/6), nasopharyngitis (1/6), headache NOS (2/6) Nasopharyngitis (1/6), chest discomfort (1/6) Nasopharyngitis (2/6), back pain (1/6), atrial fibrillation (1/6), dizziness (1/6), gastritis (1/6) Rhinorrhea (1/6), abdominal pain (1/6), arthralgia (1/6), chest discomfort (1/6), headache (1/6), malaise (1/6), stomatitis (1/6), cheilitis (1/6), conjunctival hemorrhage (1/6), contusion (1/6), dermatitis contact (1/6), herpes zoster (1/6), hypoesthesia (1/6), seasonal allergy (1/6), sensation of block in ear (1/6), tinnitus (1/6) Nasopharyngitis (5/6), rhinorrhea (2/6), injection site pain (1/6), abdominal pain (1/6), arthralgia (1/6), back pain (1/6), eczema (1/6), headache (1/6), malaise (1/6), stomatitis (1/6), thermal burn (1/6), bronchitis acute (1/6), diarrhea (1/6), fatigue (1/6), muscle fatigue (1/6), rash (1/6) Injection site pain (2/6), nasopharyngitis (1/6), eczema (1/6), thermal burn (1/6), blepharospasm (1/6), blister (1/6), conjunctivitis (1/6), hemorrhage subcutaneous (1/6), injection site erythema (1/6), periarthritis (1/6), periodontal infection (1/6), spondylosis (1/6) Arthralgia (1/10), contusion (1/10), muscle fatigue (1/10), tinnitus (1/10), chest pain (1/10), dermatitis (1/10), gingival bleeding (1/10), hepatic enzyme increased (1/10), injection site hemorrhage (1/10), lip blister (1/10), myalgia (1/10), pruritus (1/10), rhinitis allergic (1/10), stomach discomfort (1/10) Nasal discharge (2/8), pain pharynx (1/8), general malaise (1/8), twilight state (1/8), CRP increased (1/8), cough (1/8), pharynx redness (1/8), chills (1/8), dull headache (1/8), Abdominal distension (1/8), headaches (1/8), cough (1/8), white blood cell decreased (1/8), white blood cell increased (1/8) Nasal discharge (2/8), triglyceride increase (2/8), pain pharynx (1/8), general malaise (1/8), twilight state (1/8), CRP increased (1/8), fever (1/8), hot feeling generalized (1/8), wooziness), (1/8), paroxysmal sneeze (1/8), tachycardia (1/8), hot flush (1/8), monocyte count increased (1/8), lymphocyte count decreased (1/8) Triglyceride increase (3/8), nasal discharge (1/8), low back ache (1/8) Pain pharynx (1/6), cough (1/6) Gastrointestinal disorders respiratory (2/12), thoracic and mediastinal disorders (2/12), infections and infestations (2/12), injury, poisoning and procedural complications (1/12), nervous system disorders (1/12) Gastrointestinal disorders respiratory (4/12), thoracic and mediastinal disorders (2/12), infections and infestations (2/12) Severity of adverse event Slight or moderate Slight or moderate No severe AEa Slight or moderate Slight (Continued) Chiba et al 491 Table 3. Continued mAb Dose Omalizumab 150 mg Omalizumab 75 mg 150 mg 300 mg 375 mg Placebo Palivizumab 3 mg/kg 10 mg/kg 15 mg/kg Romiplostim 0.3 mg/kg 1 mg/kg 2 mg/kg Placebo Tocilizumab 0.15 mg/kg 0.5 mg/kg 1 mg/kg All adverse event (number of patients) Laboratory test abnormal (1/20), skin and subcutaneous tissue disorders (1/20) Respiratory, thoracic and mediastinal disorders (5/12), general disorders and administration site conditions (2/12), gastrointestinal disorders (1/12), skin and subcutaneous tissue disorders (1/12) Respiratory, thoracic and mediastinal disorders (1/12), skin and subcutaneous tissue disorders (1/12) Respiratory, thoracic and mediastinal disorders (4/12), gastrointestinal disorders (2/12), general disorders and administration site conditions (1/12), nervous system disorders (1/ 12) Respiratory, thoracic and mediastinal disorders (5/12), general disorders and administration site conditions (1/12), gastrointestinal disorders (1/12), nervous system disorders (1/12), skin and subcutaneous tissue disorders (1/12), musculoskeletal and connective tissue and bone disorders (1/12) Respiratory, thoracic and mediastinal disorders (7/24), general disorders and administration site conditions (4/24), nervous system disorders (3/24), musculoskeletal and connective tissue and bone disorders (2/24), gastrointestinal disorders (2/24), cardiac disorders (1/24), infections and infestations (1/24), renal and urinary disorders (1/24), skin and subcutaneous tissue disorders (1/24) Respiratory system disorder (4/12), urogenital diseases (3/12), general disorders and administration site conditions (2/12), enterogastric disorder (1/12), blood and lymphatic system disorders (1/12) Urogenital diseases (1/6) Respiratory system disorder (3/6), general disorders and administration site conditions (2/6), enterogastric disorder (2/6) Laboratory test abnormal (4/6), gastrointestinal disorders (1/6), general disorders and administration site conditions (1/6), musculoskeletal and connective tissue disorders (1/6), nervous system disorders (1/6) Gastrointestinal disorders (3/6), general disorders and administration site conditions (2/6), nervous system disorders (2/6), laboratory test abnormal (1/6), metabolism and nutrition disorders (1/6), musculoskeletal and connective tissue disorders (1/6) Infections and infestations (3/6), gastrointestinal disorders (2/6), laboratory test abnormal (2/6), musculoskeletal and connective tissue disorders (2/6), nervous system disorders (1/6) Gastrointestinal disorders (2/6), general disorders and administration site conditions (1/6), immune system disorders (1/6), infections and infestations (1/6), laboratory test abnormal (1/6) Eye disorders (1/5), gastrointestinal disorders (1/5), laboratory test abnormal (1/5) Laboratory test abnormal (3/5), gastrointestinal disorders (2/5), infections and infestations (1/5), eye disorders (1/5), respiratory, thoracic and mediastinal disorders (1/5), musculoskeletal and connective tissue disorders (1/5), general disorders and administration site conditions (1/5) Respiratory, thoracic and mediastinal disorders (3/5), gastrointestinal disorders (3/5), musculoskeletal and connective tissue disorders (3/5), laboratory test abnormal (3/5), general disorders and administration site conditions (2/5) Severity of adverse event No severe AEb Slight or moderate Slight or moderate Slight or moderate Slight Moderate Moderate (Continued) The Journal of Clinical Pharmacology / Vol 54 No 5 (2014) 492 Table 3. Continued mAb Dose 2 mg/kg Placebo All adverse event (number of patients) Immune system disorders (4/5), general disorders and administration site conditions (2/5), laboratory test abnormal (2/5), respiratory, thoracic, and mediastinal disorders (1/5) Immune system disorders (3/8), respiratory, thoracic, and mediastinal disorders (3/8), gastrointestinal disorders (3/8), general disorders and administration site conditions (2/8), psychiatric disorders (1/8), eye disorders (1/8), musculoskeletal and connective tissue disorders (1/8), laboratory test abnormal (1/ 8), injury, poisoning, and procedural complications (1/8) Severity of adverse event Slight Slight AE, adverse event; CRP, C‐reactive protein; i.v., intravenous; mAb, monoclonal antibody; NOS, not otherwise stated; s.c., subcutaneous. The common technical document (CTD) is unavailable. b There is no description about severity in the CTD. a reactions observed in Phase I studies involving healthy Japanese volunteers. As indicated in this table, the majority of adverse reactions were classified as slight, with only a few moderate events. No severe adverse reactions were reported in any of the studies. Discussion The PMDA has accumulated much data through evaluation of drugs developed by bridging strategies that can allow for comparisons of ethnic differences or similarities, and may allow us to predict the impact of ethnicity for new compounds. In this review, we first examined the study type and sampling methods used in the Japanese clinical pharmacokinetic studies of mAbs, as reported in the PMDA’s publically available database of NDAs. The sampling methods of all mAbs, except for eculizumab, involved intensive blood sampling, suggesting that the studies were classified as pharmacokinetic/safety studies. Although the “Basic Principles on Global Clinical Trials” acknowledges the possibility of a waiver for pharmacokinetic/ safety studies, Japanese pharmacokinetic/safety studies are still required before Japanese patients can be enrolled in global clinical trials. Simultaneous filing of a NDA with global clinical trials is becoming increasingly common in Japan and Asia. Drug development programs generally start in the US/EU, and Asian populations are ideally incorporated after establishing the proof of concept to reduce the risk of attrition. However, if regional pharmacokinetic/safety studies are essential, it may be difficult for the sponsor to include time for such studies between the first‐in‐human and proof of concept studies. Additionally, from ethical and efficiency perspectives, it might be difficult to expect clinically meaningful results from Japanese pharmacokinetic/safety studies for mAbs in particular, because the pharmacokinetics of mAbs are dependent on the target levels, which could be measured in diagnostic practice. In the present review, we retrieved the PMDA’s evaluation of each mAb from the CTD and review reports. Through this review, we found that the scientific discussion regarding the apparent ethnic differences for omalizumab, ibritumomab tiuxetan, and rituximab focused on the possible differences in antigen levels between Japanese and non‐Japanese subjects. Of course, it is difficult to exclude possible ethnic differences in genetic factors, and differences in antigen levels might contribute to the different pharmacokinetic/pharmacodynamic results. We also found that the pharmacokinetics of mAbs targeting soluble antigens were similar between Japanese and non‐Japanese subjects, except for omalizumab and ustekinumab, which were comparable either numerically or after considering body weight. The effects of body size on the pharmacokinetics of mAbs were discussed in the context of adjusting the doses of mAbs, and it was suggested that body weight had little or only moderate effects on the doses of most mAbs.17,18 Of note, studies in healthy Japanese volunteers may not provide any additional insight into the pharmacokinetic properties of a mAb beyond that obtained in prior Phase I studies of non‐Japanese subjects. Actually, the doses selected in subsequent Japanese patient phases were the same as those stated on the approved US labels, even if there were differences in pharmacokinetics in the healthy volunteer studies (omalizumab, Table 2). In this review, we confirmed that there are essentially no differences in exposure between Japanese and non‐Japanese subjects, and that there are no safety concerns specific to healthy Japanese volunteers for the mAbs approved in Japan. Keizer et al8 suggested that Phase I studies in healthy volunteers may provide only limited information regarding the pharmacokinetics characteristics of mAbs. Additionally, the need for fractionated doses of many mAbs means that the pharmacokinetic characteristics determined in Phase I studies may not truly represent the pharmacokinetics in patients. Although the incidence of severe adverse reactions may be low for many mAbs, Chiba et al 493 mAb Are PK characteristics linear? Yes No Considering the safety, is an ethnic difference of the antigen level predictable? Yes Predict the antigen level and pharmacokinetics Is there any exposureindependent toxicity?b No Safety (PK) study in patientsa (intensive sampling) No yes Skip Japanese phase I studies Safety studyc Sparse PK sampling can be performed in Phase II studies Figure 3. Proposed algorithm for assessing whether Phase I studies in Japanese patients could be waived for monoclonal antibodies if data from prior non‐Japanese studies are available. aIntensive blood sampling may be performed in Phase IIa studies instead of Phase I studies. bThe need for safety studies to detect exposure‐independent toxicity in Japanese patients should be discussed with the Pharmaceutical and Medical Devices Agency. cConsidering Japanese‐specific antigen‐independent serious adverse events, studies (possibly Phase II) should be conducted with careful monitoring of safety. Studies in other Asian countries might be useful to predict safety profiles in Japanese patients. reducing the exposure of healthy volunteers to clinically relevant doses of mAbs is important from a safety perspective. Based on these issues, we suggest that Phase I studies in Japanese healthy volunteers could be waived. Moreover, Phase I‐type studies in Japanese patients could be waived for some mAbs if suitable studies have already been performed in other countries. Figure 3 presents an algorithm that could help determine whether or not such studies could be waived. First, from a pharmacokinetic perspective, if the mAb shows linear pharmacokinetics within the anticipated therapeutic dose range in prior non‐Japanese Phase I studies, almost all antigens must form a complex with excessive mAbs. Hence, low antigen levels do not affect the pharmacokinetics of the mAbs. If the mAb shows a non‐linear profile, its pharmacokinetic properties are most likely affected by the target levels. In this case, if the target level can be measured or predicted, the pharmacokinetic properties of the mAb can be predicted in Japanese subjects. If the target level cannot be measured or predicted, then it is necessary to perform appropriate pharmacokinetic/safety studies in Japanese subjects. Next, from a safety perspective, if the pharmacokinetics of a mAb are linear or can be predicted from prior studies in non‐Japanese subjects, then the sponsor must consider the risk of exposure‐independent toxicity due to off‐target toxicity. If this is the case, the toxicity will not be predictable and safety studies might be necessary in Japanese subjects. However, it might be necessary to conduct such studies in the target patients considering the benefit/risk balance. By contrast, if exposure‐independent toxicity is not apparent, pharmacokinetic/safety studies involving intensive sampling in healthy volunteers and patients may be unnecessary. In conclusion, the present analyses revealed no essential differences between Japanese and non‐Japanese subjects, particularly in healthy volunteers, in the exposure of mAbs that have been approved in Japan. The PMDA assessment of similarity was reasonable, as the ranges of Cmax and AUC ratios were 0.6–1.4 and 0.6– 1.3, respectively, although there were a few exceptions. Moreover, most of the observed differences in PK were accounted for by differences in body weight or in target expression levels between Japanese and non‐Japanese subjects. The studies entailed intensive blood sampling, except for one mAb in which sparse sampling methods were used. Studies in healthy volunteers were conducted for approximately half of the mAbs. Based on these data, we think that a waiver for Japanese pharmacokinetic/ safety studies following non‐Japanese Phase I studies will become more commonplace. Our review should help in the evaluation of mAbs currently under development, and to determine the necessity for Japanese Phase I pharmacokinetic and safety studies. Acknowledgments We wish to thank Shinichi Tsuchiwata, MSc, for scientific advice and Nicholas D. Smith, PhD, for providing editorial support. Declaration of Conflicting Interests Hiroyuki Yoshitsugu was an employee of Bristol‐Myers Squibb Co., Ltd. at the time of this research. Masaki Hiraoka is an employee of Bristol‐Myers K.K. Satofumi Iida and Koichiro Yoneyama are employees of Chugai Pharmaceutical Co., Ltd. Takahiko Tanigawa is an employee of Bayer Pharma AG. The authors have no stock options or other incentives in addition to research support and consulting agreements. Author Contributions Koji Chiba and Hiroyuki Yoshitsugu designed research method; all of the authors performed analyzed the research and results; Koji Chiba Takahiko Tanigawa wrote the manuscript; all of authors read and reviewed the manuscript. the and and the References 1. International Conferrence on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH Harmonised Tripartite Guideline: Ethnic Factors in the Acceptability of Foreign Clinical Data: E5(R1) 1998. 2. Pharmaceutical and Medical Safety Bureau, Ministry of Health, Labour and Welfare, Japan. Notification No. 739 (kyokuchou‐tsuuchi). August 11. Tokyo: Ministry of Health, Labour and Welfare; 1998. 3. Evaluation and Licensing Division, Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare, Japan. Basic Principles on Global Clinical Trials. Notification no. 0928010; 2007. 494 4. 5. 6. 7. 8. 9. 10. 11. http://www.pmda.go.jp/regulatory/file/guideline/new_drug/GlobalClinicalTrials_en.pdf. Ichimaru K, Toyoshima S, Uyama Y. Effective global drug development strategy for obtaining regulatory approval in Japan in the context of ethnicity‐related drug response factors. Clin Pharmacol Ther. 2010;87:362–366. Zhou H, Tsukamoto Y, Davis HM. Should clinical pharmacokinetic bridging studies between Caucasian and Asian populations be required for approval of monoclonal antibodies? J Clin Pharmacol. 2012;52:1273–1276. Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84: 548–558. Brambell FW. The transmission of immunity from mother to young and the catabolism of immunoglobulins. Lancet. 1966;2:1087–1093. Keizer RJ, Huitema AD, Schellens JH, Beijnen JH. Clinical pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:493–507. Mould DR, Green B. Pharmacokinetics and pharmacodynamics of monoclonal antibodies: concepts and lessons for drug development. BioDrugs. 2010;24:23–39. Ishii‐Watabe A, Saito Y, Suzuki T, et al. Genetic polymorphisms of FCGRT encoding FcRn in a Japanese population and their functional analysis. Drug Metab Pharmacokinet. 2010;25:578–587. Smith KG, Clatworthy MR. FcgammaRIIB in autoimmunity and infection: evolutionary and therapeutic implications. Nat Rev Immunol. 2010;10:328–343. The Journal of Clinical Pharmacology / Vol 54 No 5 (2014) 12. Takai T. Roles of Fc receptors in autoimmunity. Nat Rev Immunol. 2002;2:580–592. 13. Torkildsen O, Utsi E, Mellgren SI, Harbo HF, Vedeler CA, Myhr KM. Ethnic variation of Fc gamma receptor polymorphism in Sami and Norwegian populations. Immunology. 2005;115:416–421. 14. Tabrizi MA, Tseng CM, Roskos LK. Elimination mechanisms of therapeutic monoclonal antibodies. Drug Discov Today. 2006;11:81–88. 15. Arnold FL, Kusama M, Ono S. Exploring differences in drug doses between Japan and Western countries. Clin Pharmacol Ther. 2010;87:714–720. 16. Myrand SP, Sekiguchi K, Man MZ, et al. Pharmacokinetics/ genotype associations for major cytochrome P450 enzymes in native and first‐ and third‐generation Japanese populations: comparison with Korean, Chinese, and Caucasian populations. Clin Pharmacol Ther. 2008;84:347–361. 17. Bai S, Jorga K, Xin Y, et al. A guide to rational dosing of monoclonal antibodies. Clin Pharmacokinet. 2012;51:119–135. 18. Wang DD, Zhang S, Zhao H, Men AY, Parivar K. Fixed dosing versus body size‐based dosing of monoclonal antibodies in adult clinical trials. J Clin Pharmacol. 2009;49:1012–1024. Supporting Information Additional supporting information may be found in the online version of this article at the publisher’s web‐site.