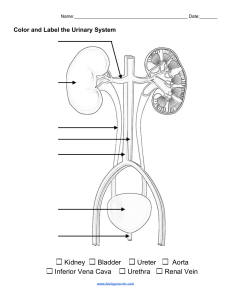
Immunizations Immunity: the ability to destroy and remove a specific antigen from the body Active immunity: acquired when a person’s OWN immune system generates the immune response Passive immunity: produced from immunoglobulins transferred from one person to another passive immunity lasts for months Contraindications for receiving vaccines o Severe febrile illness o Immunocompromised child should not receive MMR, MMRV, or Varicella o Known allergy to vaccine or its content (MMR, influenza, yellow fever all contains egg) o Pregnant patients should not receive MMR Barriers to receiving Vaccines: o Associated costs o Concern about safety o Misconceptions about vaccine link to autism and learning problems o Multiple children in household VIS—Vaccine Information Sheet: o Must be given to parent/caregiver and then consent PRIOR to vaccine administration o NO VIS or CONSENT= NO VACCINE!!! o VIS associate with each type of vaccine Skin Disorders Causes of skin disorders: o Exposure to infectious microorganisms o Hypersensitivity reactions; poison ivy o Hormonal influences o Injuries; burns and bites Bacterial infections o Cause: staphylococci and streptococci o At risk: children with congenital or acquired conditions o Prevention: HANDWASHING o TX: oral, topical, IV antibiotics o Types of Bacterial Infections Impetigo (staph) Presents: red maculesbecome vesicular Rupture easily, Dries and crusts over CONTAGIOUS TX: TAO, Mupiricin, oral antibiotics Pyoderma (staph, Strep) Presents: infection to dermis Lymphangitis; lymph nodes near site become inflamed Sepsis, heart disease Skin to skin TX: soap and water cleanse, mupirocin, or antibiotics o TX early to keep from invading lymph Cellulitis (step, Staph, Haemophiles, Influenzae) Inflammation of skin and subcutaneous tissues Presents: intense redness, swelling, firm infiltration, fever, malaise, may involve lymph nodes, may progress to abscess TX: antibiotics and rest o May require hospitalization o ** Keep on bedrest so area can heal** Viral infections o Virus that causes epidermal cells to become inflamed and to vesiculate as in HSV o to form growths like wartz o TX: antivirals and treating the cause Verruca or Wartz Cause: HPV Present: well-circumcised, grey or brown, firm and elevated Usually on hands, fingers, face, soles on exposed areas Tx: surgery, cryotherapy, causative solutions Tend to leave scars Fungal infections o Caused by fungi and are superficial, live on skin (not in skin), invades the stratum, corneum, hair and nails o Tx: ketoconazole, Nystatinapply topically, orally, or IV Tinea Cruris (Jock Itch) Yeast in peri area Prevention: use own equipment, towels, fresh underwear, etc. Tx: clotrimazole Transmitted person to person Acne o Classifications: Mild: primarily inflammatory lesions (comedones) Moderate: Comedones plus inflammatory lesions such as papules or pustules (localized to face and back) Severe: lesions similar to moderate acne, but more widespread, and/or presence of cysts or nodules --> scarring Burns o Classification: Superficial ( 1st degree)epidermal injury, heals without scarring Partial thickness (2nd degree)epidermal and dermal involvement, heals with minimal scarring Deep partial thickness (3rd degree) causes changes in sebaceous gland function and appearance of hair and nails; takes longer to heal, may scar, may require surgery Full thickness (4th degree) significant tissue damage, scarring through to the hypodermis; may cause contracture and limited functions; extensive scarring, significant healing time, requires surgery and grafting Cold Injury or Frostbite o Classification: 1st degree: superficial white layers with surrounding erythema 2nd degree: demonstrates blistering with erythemia and edema 3rd degree: Hemorrhagic blisters 4th degree: progresses to tissue necrosis and sloughing Genitourinary Disorders Differences in Anatomy o Kidney: large in relation to the abdomen prone to injury o Urethra: shorterR/F infection due to bacterin in bladder (UTI); especially in women o Glomerular Filtration Rate: slower in infants; R/F Dehydration Types of genitourinary disorders: o Congenital: where there is an obstruction as in glomerulonephritis o Structural: as in bladder exstrophy (bladder develops outside of body), hypospadias (opening of penis is on the underside and not the tip), or vesicoureteral reflux (abnormal flow of urine back up the ureters) o Acquired: as in nephrotic syndrome (kidney disorder where the body excretes too much protein), acute glomerulonephritis, or hemolytic-uremic syndrome Urinary Tract Infections: o Lower UTI: urethra and bladder o Upper: ureters, renal pelvis, renal cortex and renal medulla o E.coli is the most common causative pathogen for genitourinary disorders o Labs: renal function tests, BUN, Uremic Acid, Creatinine, MRI, Cystoscopy Enuresis o s/s: common inappropriate voiding must occur at least 2 times per week for at least 3 months in a child who is at least 5 years old *common in males* o Types: Nocturnal: (at night, ages 6-8) Primary: bedwetting in child that has never been dry for extended periods Secondary: bedwetting in children after a period of established continence o tx: antidiuretic, antispasmatics, tricyclic antidepressants, limiting fluids Phimosis: o s/s: narrowing of the preputial opening of the foreskin, prevents retracting of the foreskin over the glans penis which results in a dribbling stream of urine or a ballooning of the foreskin with urine during voiding o tx: proper hygiene of foreskin and not forcibly trying to retract the foreskin Hydrocele: peritoneal fluid in the scrotum o s/s: painless swelling, nonincarcerated inguinal hernia usually resolves by age 1 o tx: surgical repair Cryptochidism: o s/s: Failure of one or both of the testes to descend o TX: surgical repositioning of the testes, hormone therapy is no longer recommended Hypospadias: o S/S: *Congenital* male urethral opening is on the underside of penis and not on the tip o TX: surgical correction between 6 and 12 months Bladder Extrophy: o S/S: Open, inside out bladder caused by failure of abdominal wall to fuse in utero o TX: treat to preserve renal function, attain urinary control, acceptable appearance, prevent UTI, and preserve external genitalia 2 diapers (one on bladder and one to cover baby bottom) Vesicoureteral Reflux VUR: backward flow of urine from the bladder into the kidneys (reflux with infection is most common cause oof pyelonephritis in children) o S/S: fever, vomiting, and chills o TX: antibiotic therapy and surgery in cases not likely to self-resolve Nephrotic syndrome: o S/S: proteinuria, hypoalbuminemia, edema, and hyperlipidemia (occurs ages 2-7 and common in males) o TX: dietary restriction (low salt), corticosteroid TX, antibiotic TX in children with peritonitis, cellulitis, and pneumonia. TX aimed to reduce protein excretion, reduce fluid retention, prevent infection, and minimize complications Acute Glomerulonephritis: glomeruli become edematous o S/S: oliguria, edema, HTN, circulatory congestion, hematuria, and proteinuria o TX: dietary restriction (sodium and fluid restriction), VS and weight assessments, I/O, antihypertensive meds Hemolytic Uremic Syndrome (HUS): uncommon acute renal disease in ages 6mo-5 yrs glomerular arterioles become swollen and occluded damaging RBCs o S/S: acquired hemolytic anemia, thrombocytopenia, or renal injury o TX: infusing fresh frozen plasma, plasmapheresis, hemodialysis, or peritoneal dialysis in the anuric child (>24hrs), who presents with HTN and seizures. Acute Kidney Injury: kidneys become unable to regulate urine volume, caused by HUS and glomerulonephritis poor perfusion, obstructions, and irreversible renal disease o S/S: HTN, anemia, seizures, cardiac failure, metabolic acidosis, hyperkalemia and uremia, high mortality rate in children, severe GFR reduction, Increased BUN, decreased renal blood flow o TX: strict I/O, limiting fluids, observing behavioral changes, fluid and electrolyte imbalances Chronic Kidney Disease: kidneys cannot maintain normal chemical structure of body fluids, progressive deterioration= uremic shock. caused by congenital malformations, chronic pyelonephritis, chronic glomerulonephritis, systemic Lupus erythematous SLE o S/S: increased BUN, increased creatinine, edema, vascular congestion (water and sodium retention), hyperkalemia, metabolic acidosis, anemia, calcium and phosphorus disturbance, growth disturbance o TX: maintain F&E balance, tx systemic complications, promote active and normal life, diet regulation, Vit D, dialysis, and kidney transplant Renal Failure: kidneys cannot concentrate urine, conserve electrolytes, or excrete waste products o S/S: can progress to end stage renal disease o TX: dialysis and kidney transplant Female Reproductive Organ Disorders o Vulvovaginitis- bacteria or yeast overgrowth o PID: caused by STI o Menstrual disorders Male Reproductive Organ Disorders o Hydrocele: fluid around 1 or both testicles o Testicular torsion: twisted testicles o Epididymitis: infection with bacteria Cardiac Disorders Two Groups: o Congenital: anatomic abnormalities present at birth HF Hypoxemia o Acquired: occurs after birth can be associated with congenital heart defect but also seen in a normal heart can be caused by infection or environmental tendencies Congenital Heart Disease (CHD): o Cause: VSD (most common), alcohol consumption, exposure to environmental toxins, and infection lead to heart issues for fetus Defects with Increased Blood Flow Arterial Septal Defect (ASD): abnormal opening between the atria, pts may be asymptomatic; hole may close spontaneously by 18 months o Characteristic systolic murmur o Pulmonary HTN or vascular obstructive disease and emboli due to increased pulmonary blood flow o Cyanotic baby Ventricular Septal Defect (VSD): abnormal opening between right and left ventricles o Frequently associated with other conditions such as COA, PDA, and pulmonary stenosis related to increased blood flow o Increased risk for infective endocarditis Patent Ductus Arteriosus (PDA): failure of the ductus arteriosus to close within the first weeks of life may or may not have symptoms of HF o Machine-like murmur o Pulmonary vascular congestion occurs causing increased pulmonary pressure Obstructive Heart Defects Coarctation of the Aorta: Narrowing near the ductus arteriosus o Pressure proximal to the defect is increased (upper extremities) o Pressure distal to defect is decreased (lower extremities) o Older child may experience headaches, dizziness, fainting, epistaxis from HTN o Risk for ruptured aorta, aortic aneurysm and stroke Aortic Stenosis: narrowing of aortic valve = resistance to blood flow in left ventricle, decreased CO, left ventricle hypertrophy and pulmonary vascular congestion. o In infant: Decreased CO, hypotension and faint pulses, tachycardia, poor feeding o In Children: Exercise intolerance, chest pain, dizziness, R/F coronary insufficiency Pulmonic Stenosis: narrowing at the entrance to the pulmonary artery= resistance to blood flow, right ventricular hypertrophy and decreased pulmonary blood flow o Mild cyanosis o Loud systolic ejection murmur may be present Defects with Decreased Pulmonary Blood Flow Tetralogy of Fallot: comprised of four conditions including: (1)VSD, (2)pulmonary stenosis, (3)overriding aorta, (4)right ventricular hypertrophy o Blue spells (tet spells) o R/F seizures o R/F LOC o R/F sudden death o TX: three surgeries open heart surgery right away Tricuspid Atresia: tricuspid valve fails to develop leads to systemic desaturation and decreased pulmonary blood flow o Older children have CHRONIC HYPOXEMIA with CLUBBING o TX: valve replacement Mixed Cardiovascular Defects Fully saturated blood flow mixes with desaturated pulmonary blood flow leads to desaturation of systemic blood flow, pulmonary congestion, decreased CO, HF, desaturation Transposition of the Great Valves: pulmonary artery leaves the left ventricle and aorta exits from the right ventricle with no communication between the systemic and pulmonary circulation; poorly oxygenated blood returns to the right atrium and right ventricle is then pumped out to the aorta and back to the body o Newborn presents with sever cyanosis and worsens as ductus arteriosus closes o Deoxygenated blood is filtering through the body Total Anomalous Pulmonary Venous Return (TAPVR): rare defect characterized by failure of the pulmonary veins to connect to the left atrium, instead they are connected to the right atrium so right atrium received blood load o Cyanotic infants Truncus Arteriosus: Failure of the normal separation and division of embryonic bulbar trunk into pulmonary artery and aorta o Most infants are asymptomatic but may have cyanosis at rest, poor growth, activity intolerance, poor feeding o Pressure is less in the pulmonary and higher in the systemic system leading to increased blood flow to lungs and decreased blood flow through system o May lead to pulmonary vascular disease over time Hypoplastic Left Heart Syndrome (HLHS): underdeveloped left side of the heart, hypoplastic left ventricle, and aortic atresia o Signs of HF until PDA closes , the heart cannot pump blood into systemic circulation causing poor perfusion of vital organs and shock o Progressive deterioration o Decrease CO o Fatal in first months of life without intervention o TX: surgery for multistage repairs and eventually a HEART TRANSPLANT Risk Factors of Cardiovascular Disorders o Family hx of heart disease or CHD (first degree relative) o Hyperlipidemia o DM o Obesity o Inactivity o Stress o High-cholesterol diet Nursing Assessments o VS o O2 o RR o Cyanosis o Mottling o Adventitious lung sounds o Activity intolerance o Lethargy o Vomiting and FTT o Edema o Abdominal distention o I/O