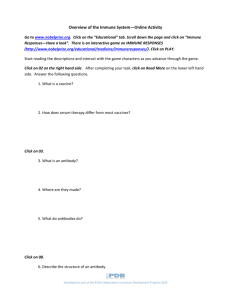
Pharmacology Exam 2 Study Guide The Body’s Defenses: Barrier Defenses Skin o first line of defense o protects the internal tissues and organs of the body o the normal bacterial flora of the skin help to destroy many disease-causing pathogens Mucous Membranes o line the areas of the body that are exposed to external influences, but do not have skin protection o include the respiratory, gastrointestinal (GI), genitourinary (GU) tracts Gastric Acid o secreted by the stomach in response to many stimuli o destroys many would-be pathogens Major Histocompatibility Complex o distinguishes between self-cells and foreign cells Mononuclear Phagocyte System (MPS) o composed of: Lymphatic tissue Leukocytes (white blood cells - WBCs) Lymphocytes - T cells, B cells, and natural killer cells Myelocytes - neutrophils, basophils, eosinophils, and monocytes or macrophages numerous chemical mediators The Body’s Defense: The Inflammatory Response Injury to a cell membrane causes a locally mediated response – release of histamine Vasodilation occurs and brings more blood and blood components to the area Alters capillary permeability and brings neutrophils to the injured area Stimulates pain perception Inflammatory Response Clinical Presentation: (sequence/order of events) o Rubor (redness/erythema) occurs first and is caused by the increase in blood flow due to vasodilation o Tumor (swelling/edema) occurs second and is caused by fluid that leaks into the tissues as a result of increased capillary permeability o Calor (heat) occurs third and is caused by increased blood flow to the area o Dolor (pain) occurs last and is caused by the activation of pain fibers by histamine and the kinin system The Body’s Defense : Immune Response More specific invasion can stimulate a more specific response through the immune system o Lymphocytes produced in the bone marrow can develop into T lymphocytes (suppressor, cytotoxic, and helper T cells) or B lymphocytes when a B cell reacts with an antigen, it transforms into a plasma cell and produces antibodies or immunoglobulins (takes several days): IgM (first exposure to the antigen) IgG (most prevalent; contains antibodies made by memory cells that circulate and enter the tissues) IgE (allergic response) IgA (found in tears, saliva, sweat, mucus, and bile; secreted by plasma cells in the GI tract, respiratory tract, and in epithelial cells) IgD (role has not yet been determined) B cells form memory cells that will produce antibodies for immediate release in the future if the antigen is encountered o Other identified lymphocytes include natural killer cells and lymphokineactivated killer cells these cells are aggressive against neoplastic or cancer cells and promote rapid cellular death Other Mediators of the Immune Response Interferons o chemicals that are secreted by cells that have been invaded by viruses o prevent viral replication and suppress malignant cell replication and tumor growth Interleukins o chemicals secreted by active leukocytes to influence other leukocytes o also cause fever, arthralgia, myalgia, and slow-wave sleep induction Tumor necrosis factor (TNF) o chemical released by macrophages o inhibit tumor growth and can cause tumor regression o Anti-inflammatory, Antiartheritis, and Related Agents Block or alter the chemical reactions associated with the inflammatory response to stop one or more of the signs and symptoms of inflammation o Corticosteroids (chapter 36) block or alter the chemical reactions associated with the inflammatory response o Antihistamines (chapter 54) block the release of histamine in the initiation of the inflammatory response o Immune-modulating agents (chapter 17) block or decrease the effects of inflammation in chronic disorders such as rheumatoid arthritis (RA) and Crohn disease Over-the-counter (OTC) anti-inflammatory agents All can cause adverse effects Salicylates Salicylates: aspirin, mesalamine, salsalate, balsalazide o can block the inflammatory response o have antipyretic properties (fever-blocking) o have analgesic (pain-blocking) properties Actions/Indications: o inhibit the synthesis of prostaglandin o used to treat mild to moderate pain and fever Contraindications: o known allergy to salicylates or NSAIDs o bleeding abnormalities o impaired renal function o use in children with viral infections such as chickenpox or influenza due to risk of Reye syndrome (manifests with vomiting, confusion, seizures, and loss of consciousness -> can cause liver damage and even death) o pregnancy or lactation Adverse Effects: o GI effects - nausea, dyspepsia, heartburn, epigastric discomfort o Bleeding o Salicylate toxicity (at doses of 20-25 grams in adults or 4 grams in children) the first sign of salicylate toxicity Is decreased hearing and tinnitus (ringing in the ears) headache and dizziness can also occur other signs and symptoms include nausea, vomiting, diarrhea, and diaphoresis (excessive sweating) with continued ingestion of salicylates, fever, confusion, seizures, and respiratory and/or renal failure can develop Drug-Drug Interactions: o increased risk of bleeding when taken with NSAIDs, anticoagulants, corticosteroids, and alcohol Nonsteroidal Anti-inflammatory Drugs (NSAIDs) Actions/Indications: o inhibit prostaglandin synthesis o block two enzymes known as COX-1 and COX-2 COX-1 is present in all tissues and is involved in platelet aggregation, protecting the stomach lining, and maintaining sodium and water balance in the kidney/blood flow to the kidney COX-2 is active at sites of trauma or injury when more prostaglandins are needed, but it does not seem to be involved in the other tissue functions (decreases inflammation, pain, and body temperature) Nonsteroidal Anti-inflammatory Drugs (NSAIDs)- continued Contraindications/Cautions: o allergy to any NSAIDs or salicylates o celecoxib is also contraindicated in the presence of allergy to sulfonamides o cardiovascular dysfunction or hypertension • linked to an increased risk of CV events and death (increased risk for thromboembolic events – MI, CVA) – recommendations are for combining NSAID with aspirin 81 mg daily to decrease risk o peptic ulcer disease (PUD) and GI bleeding o pregnancy (celecoxib is teratogenic in the third trimester) and lactation (crosses the placenta and passes into breast milk) o renal dysfunction o hepatic dysfunction Adverse Effects: o GI effects: nausea, dyspepsia, GI pain, constipation, diarrhea, or flatulence o GI bleed (monitor complete blood count [CBC]), ulceration, perforation (Black Box Warning) o CNS effects: headache, dizziness, somnolence, & fatigue o platelet inhibition o hypertension o cardiovascular thrombotic event (Black Box Warning) o bone marrow depression o rash and mouth sores Drug-Drug Interactions: o decreased diuretic effect when these drugs are taken with loop diuretics o potential for decreased antihypertensive effect of beta-blockers if these drugs are combined o lithium toxicity, especially when combined with ibuprofen Acetaminophen (Tylenol) Actions: o acts directly on the thermoregulatory cells of the hypothalamus to cause sweating and vasodilation which causes the release of heat and lowers fever o mechanism of action unknown but related to analgesic effects o used to treat pain and fever o treat pain and fever associated with a variety of conditions, including influenza o prophylaxis of children receiving diphtheria–pertussis–tetanus (DPT) immunizations o relief of musculoskeletal pain associated with arthritis Contraindications: o known allergy o caution in pregnancy and lactation o hepatic dysfunction (toxic doses can cause liver damage/failure -> antidote is acetylcysteine [Mucomyst] – available oral or IV) o chronic alcoholism Limit daily use to < 4 grams from all sources Anti-Rheumatic Agents: Disease Modifying Antirheumatic Drugs (DMARDs) Aggressively affect the process of inflammation Adverse effects of DMARDs can be severe to life-threatening because they alter the ability of the body to initiate or carry on an inflammatory reaction Since they alter the course of the inflammatory process, many rheumatologists are selecting to utilize DMARDs early in the diagnosis, before damage to the joints has occurred Two Types of DMARDs: adalimumab (Humira), etanercept (Enbrel), infliximab (Remicade) o Tumor Necrosis Factor (TNF) blockers cannot be used in anyone with an acute infection, cancer, sepsis, tuberculosis, hepatitis, myelosuppression or demyelinating disorders (because they block the body’s immune/inflammatory response – serious reactions may occur) Black Box Warnings: risk of serious to fatal infections and the development of lymphomas and other cancers live vaccines should not be administered while on TNF blockers o Other DMARDs Immune Modulators: Immune Stimulants Immune modulators modify the actions of the immune system: Immune Stimulants: o Interferons: naturally released from human cells in response to viral invasion prevent virus particles from replicating inside other cells stimulate interferon receptor sites on noninvaded cells to produce antiviral proteins which prevent viruses from entering the cell inhibit tumor growth and replication Adverse Effects: lethargy, myalgias, arthralgias, anorexia, nausea, headache, dizziness, depression and suicidal ideation, bone marrow depression, hepatic impairment, and photosensitivity o Interleukins: chemicals produced by T cells to communicate between lymphocytes, stimulate cellular immunity, and inhibit tumor growth Adverse Effects: flu-like effects such as lethargy, myalgias, arthralgias, fatigue, and fever respiratory difficulties CNS changes cardiac arrythmias o Colony-stimulating factors: stimulate bone marrow to produce more WBCs (neutrophils) Immune Modulators: Immune Suppressants Immune suppressants are often used in conjunction with corticosteroids which block the inflammatory reaction and decrease initial damage to cells Especially beneficial in organ transplantation (client will require immunosuppressant therapy for life to prevent transplanted organ rejection) and in the treatment of autoimmune diseases o Immune Modulators: block the release of various cytokines involved in the inflammatory response and activation of lymphocytes, decreasing immune activity o T and B Cell Suppressors: block antibody production by B cells; inhibit suppressor and helper T cells; modify the release of interleukins and of T cell growth factor o Interleukin Receptor Antagonist: work to block the activity of the interleukins that are released in an inflammatory or immune response (used to treat moderate-tosevere rheumatoid arthritis in patients >=18 years of age and older who have not responded to the traditional antirheumatic drug) o Monoclonal Antibodies: antibodies that attach to specific receptor sites that are developed to respond to very specific situations (must match to specific target cell receptor sites – if there is not a match, treatment will not be successful) Immunity A state of relative resistance to a disease that develops after exposure to the specific disease-causing agent People are not born with immunity to diseases, so they must acquire immunity by stimulating B-cell clones to form plasma cells and then antibodies Types of Immunity: o Active Immunity the body recognizes a foreign protein and begins producing antibodies to react with it (i.e., direction infection with a microorganism or vaccination) o Passive Immunity occurs when preformed antibodies are injected into the system and react with a specific antigen (i.e., from mother to infant through breast milk or through the placenta) Immunization: the process of artificially stimulating active immunity by exposing the body to weakened or less toxic proteins associated with specific disease-causing organisms o the goal is to cause an immune response without having the patient suffer the full course of a disease Vaccines (see table 18.1) Vaccines are immunizations containing weakened or altered protein antigens that stimulate the formation of antibodies against a specific disease o Made from chemically inactivated microorganisms or from live or weakened viruses or bacteria Stimulate active immunity in people who are at risk The vaccines that are needed depends on the exposure the person will have to pathogens Some vaccines require booster doses Vaccines are thought to provide life-long immunity to the disease against which the patient is being immunized Vaccines are contraindicated in the presence of immune deficiency, pregnancy, known allergy to the components of the vaccine, acute infection/high fever, and patients receiving immunoglobulins or blood products within the past 3 months (a serious immune reaction can occur) Drug-Drug Interactions: vaccines should not be given with any immunosuppressant drugs, including corticosteroids, which could alter the body’s response to the vaccine Immune Sera Antibodies are found in immune sera, which may contain antibodies to toxins, venins, bacteria, viruses, or even red blood cell antigenic factors Immune sera refers to sera that contain antibodies to specific bacteria or viruses These drugs are used to provide early treatment following exposure to known antigens Types: o Antitoxin - immune sera that have antibodies to very specific toxins that might be released by invading pathogens (i.e., botulism) o Antivenom - immune sera that have antibodies to venom that might be injected though spider or snake bites Action: o provide passive immunity to a specific antigen or disease o used as prophylaxis against specific disease after exposure o may lessen the severity of a disease Adverse Effects: allergic reaction (chest tightness, hypotension, and dyspnea (difficulty breathing) Drug-Drug Interactions: immunosuppressant drugs, including corticosteroids (can alter the body’s response to the biologicals) Clotting Process A complex process that involves vasoconstriction, platelet clumping or aggregation, and a cascade of clotting factors produced in the liver that eventually react to break down fibrinogen (a protein also produced in the liver) into insoluble fibrin threads When a clot is formed, plasmin (another blood protein) acts to break it down Blood coagulation can be affected at any step in this complicated process to alter the way that blood clotting occurs Blood Vessel Injury Local transient vasoconstriction seals off small injury Platelet aggregation forms a platelet plug o once they stick, the platelets release adenosine diphosphate (ADP), serotonin, and other chemicals that attract other platelets, causing them to gather or aggregate and to stick as well o ADP is also a precursor of the prostaglandins, from which thromboxane A2 is formed and causes local vasoconstriction and further platelet aggregation Hageman factor (Factor XII) is activated which then activates Factor XI and the intrinsic pathway is stimulated Intrinsic pathway ends with the conversion of prothrombin to thrombin to seal system (calcium is the catalyst) -> thrombus Extrinsic pathway causes the blood that has leaked out of the vascular system into the surrounding tissues to clot The extrinsic and intrinsic clotting pathways converge into the common clotting pathway starting at the activation of Factor X Clot Resolution Blood plasma also contains anticlotting substances that inhibit clotting reactions that might otherwise lead to an obstruction of blood vessels by blood clots o antithrombin III prevents the formation of thrombin, thus stopping the breakdown of the fibrin threads o plasmin, or fibrinolysin, dissolves clots to ensure free movement of blood through the system • plasmin is a protein-dissolving substance that breaks down the fibrin framework of blood clots and opens up vessels • its precursor, plasminogen, is made in the liver and the conversion of plasminogen to plasmin begins with the activation of Hageman factor