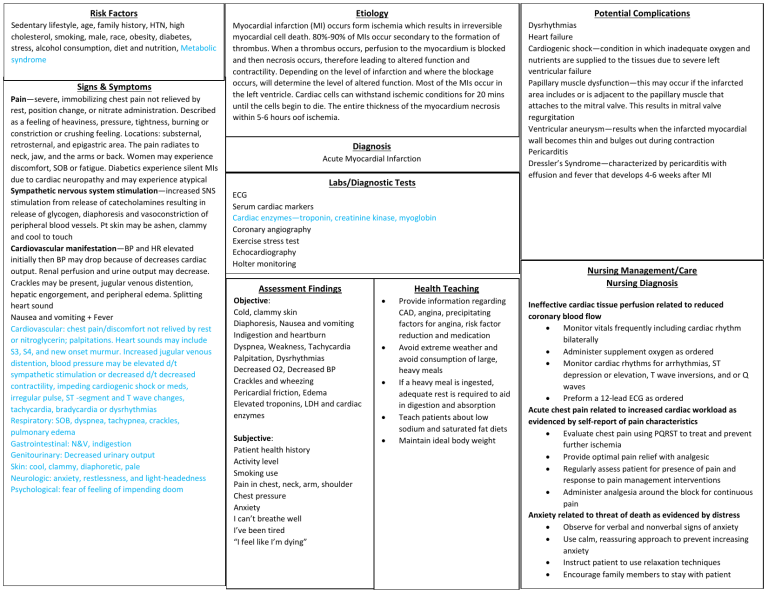
Risk Factors Sedentary lifestyle, age, family history, HTN, high cholesterol, smoking, male, race, obesity, diabetes, stress, alcohol consumption, diet and nutrition, Metabolic syndrome Signs & Symptoms Pain—severe, immobilizing chest pain not relieved by rest, position change, or nitrate administration. Described as a feeling of heaviness, pressure, tightness, burning or constriction or crushing feeling. Locations: substernal, retrosternal, and epigastric area. The pain radiates to neck, jaw, and the arms or back. Women may experience discomfort, SOB or fatigue. Diabetics experience silent MIs due to cardiac neuropathy and may experience atypical Sympathetic nervous system stimulation—increased SNS stimulation from release of catecholamines resulting in release of glycogen, diaphoresis and vasoconstriction of peripheral blood vessels. Pt skin may be ashen, clammy and cool to touch Cardiovascular manifestation—BP and HR elevated initially then BP may drop because of decreases cardiac output. Renal perfusion and urine output may decrease. Crackles may be present, jugular venous distention, hepatic engorgement, and peripheral edema. Splitting heart sound Nausea and vomiting + Fever Cardiovascular: chest pain/discomfort not relived by rest or nitroglycerin; palpitations. Heart sounds may include S3, S4, and new onset murmur. Increased jugular venous distention, blood pressure may be elevated d/t sympathetic stimulation or decreased d/t decreased contractility, impeding cardiogenic shock or meds, irregular pulse, ST -segment and T wave changes, tachycardia, bradycardia or dysrhythmias Respiratory: SOB, dyspnea, tachypnea, crackles, pulmonary edema Gastrointestinal: N&V, indigestion Genitourinary: Decreased urinary output Skin: cool, clammy, diaphoretic, pale Neurologic: anxiety, restlessness, and light-headedness Psychological: fear of feeling of impending doom Potential Complications Etiology Myocardial infarction (MI) occurs form ischemia which results in irreversible myocardial cell death. 80%-90% of MIs occur secondary to the formation of thrombus. When a thrombus occurs, perfusion to the myocardium is blocked and then necrosis occurs, therefore leading to altered function and contractility. Depending on the level of infarction and where the blockage occurs, will determine the level of altered function. Most of the MIs occur in the left ventricle. Cardiac cells can withstand ischemic conditions for 20 mins until the cells begin to die. The entire thickness of the myocardium necrosis within 5-6 hours oof ischemia. Diagnosis Acute Myocardial Infarction Labs/Diagnostic Tests ECG Serum cardiac markers Cardiac enzymes—troponin, creatinine kinase, myoglobin Coronary angiography Exercise stress test Echocardiography Holter monitoring Assessment Findings Health Teaching Objective: Cold, clammy skin Diaphoresis, Nausea and vomiting Indigestion and heartburn Dyspnea, Weakness, Tachycardia Palpitation, Dysrhythmias Decreased O2, Decreased BP Crackles and wheezing Pericardial friction, Edema Elevated troponins, LDH and cardiac enzymes Subjective: Patient health history Activity level Smoking use Pain in chest, neck, arm, shoulder Chest pressure Anxiety I can’t breathe well I’ve been tired “I feel like I’m dying” Provide information regarding CAD, angina, precipitating factors for angina, risk factor reduction and medication Avoid extreme weather and avoid consumption of large, heavy meals If a heavy meal is ingested, adequate rest is required to aid in digestion and absorption Teach patients about low sodium and saturated fat diets Maintain ideal body weight Dysrhythmias Heart failure Cardiogenic shock—condition in which inadequate oxygen and nutrients are supplied to the tissues due to severe left ventricular failure Papillary muscle dysfunction—this may occur if the infarcted area includes or is adjacent to the papillary muscle that attaches to the mitral valve. This results in mitral valve regurgitation Ventricular aneurysm—results when the infarcted myocardial wall becomes thin and bulges out during contraction Pericarditis Dressler’s Syndrome—characterized by pericarditis with effusion and fever that develops 4-6 weeks after MI Nursing Management/Care Nursing Diagnosis Ineffective cardiac tissue perfusion related to reduced coronary blood flow Monitor vitals frequently including cardiac rhythm bilaterally Administer supplement oxygen as ordered Monitor cardiac rhythms for arrhythmias, ST depression or elevation, T wave inversions, and or Q waves Preform a 12-lead ECG as ordered Acute chest pain related to increased cardiac workload as evidenced by self-report of pain characteristics Evaluate chest pain using PQRST to treat and prevent further ischemia Provide optimal pain relief with analgesic Regularly assess patient for presence of pain and response to pain management interventions Administer analgesia around the block for continuous pain Anxiety related to threat of death as evidenced by distress Observe for verbal and nonverbal signs of anxiety Use calm, reassuring approach to prevent increasing anxiety Instruct patient to use relaxation techniques Encourage family members to stay with patient Medical Management (Pharmacological/Surgical) Nitroglycerin—reduce angina pain and improve coronary blood flow Monitor BP Anticoagulants such as ASA Morphine—Given for chest pain unrelieved by nitro Vasodilator, it can decrease cardiac workload by lowering myocardial oxygen consumption, reducing contractility, and decreasing BP and HR Monitor for bradypnea and hypoxia Oxygen given usually between 2L to 4L via nasal cannula ACE inhibitors—recommended after anterior wall MIs or MIs that result in decrease left ventricular function. Can help prevent ventricular remodelling and prevent or slow progression of HF Surgical procedure CABG—placement of conduits to transport blood between aorta or other major arteries. Involves use of grafts Coronary artery bypass---minimally invasive and uses thoracoscope Percutaneous coronary intervention—procedure to open the occluded coronary artery and promote reperfusion to the area that has been deprived of oxygen References Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier. Hinkle, J. L., & Cheever, K. H. (2018). Brunner & Suddarths textbook of medical-surgical nursing. Philadelphia: Wolters Kluwer. Lewis, S. L., Bucher, L., MacLean Heitkemper, M., Harding, M. M., Barry, M., Lok, J., Tyerman, J., & Goldsworthy, S. (Eds.). (2019). MedicalSurgical Nursing in Canada: Assessment and Management of Clinical Problems (4th ed.). Elsevier Canada Skidmore-Roth, L. (2015). Mosbys Drug Guide for Nursing Students. Mosby.




