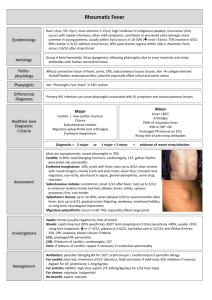
RHEUMATIC FEVER Definotion: Rheumatic fever is an inflammatory disease involving mainly the joints and the heart and less frequently then the central nervous system, skin, and subcutaneous tissues. It has a marked tendency to recur, and both initial and recurrent attacks are non suppurative complications of group A streptococcal upper respiratory infection. Pathogenesis: Not definitely known. 1. Hypothesis of allergy to streptococcus of group A: There is much evidence that the initial and subsequent of rheumatic fever follow scarlet fever or upper respiratory infection due to β-hemolytic streptococci group A. The attack of streptococcal pharyngitis may be extremely mild or moderately severe [phase I]. In most instances, the symptoms of upper respiratory infection subside quickly and are followed by a latent or "silent" period [phase II] usually lasting one to three weeks. During which the patient is symptom-free. Phase II is followed by the onset of -acute rheumatic fever [ phase III ]. If penicillin is given early within the first 9 days and in sufficient quantity over an adequate period of time, the patient escapes rheumatic fever. With such therapy, the hemolytic streptocococci are eradicated from the throat in most instances. The concept that rheumatic fever is an allergic process is based in part upon the following points: a) The fibrinoid degeneration of collagen is considered to be the characteristic of allergic disease. b) A peroid of 1 - 3 weeks commonly intervenes between the streptococcal. infection and the onset of rheumatic fever. Such an interval is characteristic of known allergic diseases. c) The acute phase of rheumatic fever has clinical signs and symptoms which are frequently indistinguishable from allergic diseases(e.g. serum sickness). d) Recurrent attacks indicate absence of immunity. 2. Hypothesis of autoimmunity: A more widely held theory is that rheumatic fever is an autoimmune disease. Several strepcococcal antigens cross-react with human tissue antigens, and cross-reactive ["anti-heart"] antibodies have been found in rheumatic fever patients. According to this hypothesis, streptococcal antigens immunologically similar to tissue antigens may elicit antibodies capable or reacting, not only with microbial products but also with the host's antigens, Thus autoimmunization may be the underlying basis for the cardiac lesion. Susceptibility: Besides infection, an important factor in the etiology of rheumatic fever is individual susceptibility. The susceptibility in child population in general Лб between 0.2 – 1 %. The child, who gets rheumatic fever may be susceptible due to familial predisposition: if one child in a family has rheumatic fever approximately 10% of the children will develop it. Age of onset: Usually between 5 - 10 years. but in some cases it does begin at the age of 2 , 3 , or 4 years, however, it is not common. , Sex Rheumatic fever may occur: in children, males and females are affected equally. Pathology: 2 stages. There are 2 stages in the development of the disease. 1. Acute (Exudative) stagey: is characterizes by an exudative inflammatory reaction in the connective tissues of: a) The heart: -Within the myocardium the cellular infiltrate [lymphocytes and plasma celis ] form in tne interstitial tissue аs well as due to damage of the muscle cells. - Edema of the valvular fibrous ring and valve leaflets. - Fibrinous or serofibrinous pericarditis. b) Joints: Swelling of the articular and periarticular structures with infiltration of synovial membranes and serous effusion. This stage lasts for 2-3 weeks and is followed by: 2. Proliferative stage: The characterized by the appearance of Aschoff’s nodules and a diffuse infiltration which end the fibrous. This phase is limited to the myocardium and endocardium. The Clinical picture and Diagnosis: Rheumatic fever may affect a number –of isolated organs and tissues, or in combination. No single clinical manifestation or laboratory test is characteristic enough to be a diagnostic. The need to bring some uniformity to the diagnosis led T.D. Jones to formulate diagnostic criteria based on combination of clinical manifestations and laboratory findinds. These criteria include: 1. Major manifestations. 2. Minor manifestations. 3. Evidence of recent group A beta- hemolytic streptococcal infection of the upper respiratory tract. I. I. Major manifestations: Arthritis: Rheumatic arthritis is characterized by the following criteria: a) It affects the big joints mainly e.g. knees, wrists, ankles, elbows. b) The affected joint shows signs of acute inflammation i.e. swollen, tender, red , hot , limitation of movements associated with severe pain. c) Several joints are commonly involved, sometimes together and sometimes one after another (migrating arthritis). d) As a rule, there is prompt improvement by salicylates; but whether salicylates are given or not, it is rare for symptoms and signs of arthritis to persist more than one week. e) No residual deformity occurs in the affected joints. II. Carditis : All layers of the heart are involved i.e. pancarditis develops. A. Pericarditis: - Pericarditis is recognized by hearing friction rub as superficial scratchy sound which is heard over the precordium especially near the sternum, and which has to and fro character. - It is accompanied by slight pain, fever, leukocytosis and usually raised S-T segment with inverted T wave in the ECG. - When pericardial effusion is formed, it produces an area of enlargedcardiac dullness and distant heart sounds. Echocardiography is very helpful in diagnosis. B. Myocarditis: Clinical manifestations of myocarditis include: - Heart failure with its manifestations as gallop rhythm, congested neck veins, edema of lower limbs,. etc. - Cardiomegaly - Arrhythmias C. Endocarditis: This leads to Mitral valve with or without Aortic valve. 1. Mitral valve: valve leads to mitral valve incompetence which is manifested by a pansystolic murmur, heard on the apex at maximum, selectively propagated to the axilla. Harsh blowing in character and does not change with respiration or change of position. The mitral valve incompetence is due to dilatation of the fibrous ring of the valve. The first heart sound is usually muffle and of decreased intensity which is caused by prolonged conduction time of AV bundle which delays ventricular contraction so that the atrioventricular valves are already more or less closed when the ventricles contract. In mitral valve another murmur may be heard: Carey Coomb's murmur. It is a soft short mid-diastolic murmur, heard on the apex. It is produced by the inflammatory thickening of the mitral cusps. This murmur occurs early in the course of rheumatic carditis, and disappears as activity subsides ( i.e. a sign of activity). 2. Aortic valve: Inflammation of the aortic valve may lead to aortic incompetence which manifests by early diastolic murmur, heard of maximum on the aortic area. It is soft blowing in character and is associated with peripheral signs of aortic incompetence: Water-hammer pulse, increased pulse pressure, pistol-shot, Corrigan's sign, and Durozier's sign. III.Chorea: Rheumatic chorea (or Sydenham's Chorea) often appears to occur alone rather than in the company of other rheumatic manifestations and the E S R is usually normal . About 20% of patients with chorea alone develop rheumatic heart disease. Chorea generally affects girls more than boys. Clinical Features: 1. Involuntary movements: purposeless, irregular, non-repetitive, jerky movements that are present at rest, become more apparent during voluntary actions and are absent during sleep. All limbs and often the face and tongue may be involved, with inability to maintain the tongue in a protruded position. The tongue movements may interfere with speech and swallowing. Respiration may be irregular and jerky. The movements may be mild or severe, unilateral or bilateral. If unilateral, it is called hemichorea. 2. Weakness of voluntary movements and hypotonia: When the hands are held forward with palms down, they assume a typical posture of flexion at the wrists and hyperextension at all finger joints (Dinner fork appearance). There is often hyperpronation of the arms if they are held above the head. The hypotonia also causes the deep reflexes to be difficult to elicit, but when obtained they show a characteristic sustained contraction (e.g. in knee jerk, the leg becomes held up at the height of its extension for an appreciable interval before relaxation occurs). Hypotonia may lead also to hyperextensibility of the joints. In some cases, hypotonia may be so severe as to amount to paralysis. 3. Incoordination of the voluntary movements (caused by superimposition of involuntary movements). This can be tested by the finger to nose or finger to finger tests. Difficulties of talking, mastication, swallowing, dressing, writing and walking are all examples of the incoordination. Associated movements are also disturbed, thus if the patient while grasping the hand is asked to protrude his tongue or clench the other fist, irregular contractions of the hand will be felt. 4. Emotional instability: which may vary in severity. In rheumatic chorea, the plantar response is flexor, and there is no sensory loss. Tine CSF is normal. There is usually no pyrexia, the ESR and C-reactive protein are normal. If there is fever or raised ESR, it is likely that active carditis is present. IV. Erythema Marginatum: It appears in rings, crescents, ovals, or in irregular forms characterized by a thin red margin outlining a patch of normal skin. It is distributed mainly on the trunk and proximal parts of the limbs. Sometimes, the rash is at first composed of irregular erythematous macules but the centers soon become clear, leaving red margins. There is no itching or discomfort. Erythema marginatum may be fleeting or persistent. V. Subcutaneous nodules: They are shot like hard bodies seen or felt over the extensor surfaces of certain joints particularly elbows, knees and wrists, in the occipital region or over the spinous processes of the thoracic or lumbar regions At the end of 8 weeks they disappear in the majority of cases. The presence of nodules is an indication that' the heart is involved, both being proliferative lesions. II. Minor Manifestations: 1. Fever: A significant rise of temperature is a common symptom, but because it occurs in so many-illnesses, it has little differential diagnostic value. Approximately 50% of the cases have fever. This fever is controlled by salicylates. 2. Arthralgia: pain clearly located without objective findings is only a minor criterion for diagnosis. The pain must be in the joint and not in the muscles or other periarticular tissues. It must be distinguished from the nocturnal pain in the extremeties occurring in normal children (called growing pains). Arthralgia must not be used as a minor criterion when polyarthritis is included as a major criterion. 3. Previous history of rheumatic fever or the presence of inactive rheumatic heart disease. 4. Prolonged P-R interval in EGG: it cannot be used as a minor criterion if carditis is already included as a major manifestation. 5. Acute Phase reactants: The positivity of one or more of these non specific tests can be considered as a single minor criterion: a) Elevated E.S.R.: simple and reliable test, though sometimes ESR is normal as in heart failure, isolated chorea, erythema marginatum and in old standing subcutaneous, nodules. b) Presence of С - Reactive Protein (CRP): CRP tends to disappear in the convalescent stage before ESR returns to normal. It may not appear if a rebound occurs. It is often absent in chorea and erythema marginatum and long standing nodules. CRP remains positive when congestive heart failure complicates active carditis ( unlike ESR). c) Leucocytosis. III. Evidence of Preceding Streptococcal Infection This must be documented by either: A) A history of scarlet fever, or a typical clinical picture of other Betahemolytic streptococcal infection of upper respiratory tract infection. This should precede the onset of rheumatic fever by one week to one month. The nature of the infection must be confirmed by a history of immediate contact with other individuals having typical streptococcal infection or by positive culture of the nose or the throat in which Beta- hemolytic streptococci predominate. B) An elevated or rising ASLO titre: an ASLO of 250 Todd units or more is considered positive. Approximately 80% of patients have an elevated ASLO. C) Patients suspected to have rheumatic fever and who do not show an elevated ASLO (20%of cases) should be tested for other streptococcal antibodies like anti- dsDNA. IV. Other Manifestations of Rheumatic Fever: These include systemic manifestations such as loss of weight, easy fatiguability, malaise, sweating, pallor , epistaxis, erythema nodosum, abdominal pain, headache and vomiting. These as well as family history of rheumatic fever , provide additional evidence of the presence of rheumatic fever , but are not to be included as diagnostic criteria. Diagnosis of Rheumatic Fever: Acute rheumatic fever is diagnosed when there is: 1. Two major Jones' criteria + evidence of preceding Beta- hemolytic streptococcal infection. Or 2. The presence of One Major + Two minor Jones' criteria + Evidence of Beta-hemolytic streptococcal infection. The main diseases with which it is necessary to differentiate acute rheumatic fever 1. non-Rheumatic myocarditis (bacterial, viral). Typical sign: - the presence of a chronological connection with acute nasopharyngeal (mainly viral) infection; - shortening (less than 5-7 days) or no latency period; - at the onset of the disease, symptoms of asthenization, violations of thermoregulation appear; - gradual development of the disease; - arthritis and severe arthralgias are absent; - cardiac complaints have an active and emotional nature; - there are clear clinical, ECG and EchoCG symptoms of myocarditis; - no valvulitis; - dissociation of clinical and laboratory parameters; - slow dynamics under the influence of anti-inflammatory therapy. 2. Post-streptococcal arthritis. It can occur in middle-aged people. It has a relatively short latent period (2-4 days) from the moment of a pharyngeal BSA infection (beta-hemolytic Streptococcus group A) and persists for a longer time (about 2 months). the Disease is not accompanied by carditis, does not respond optimally enough to anti-inflammatory drugs and completely regresses without residual changes. 3. Endocarditis in systemic lupus erythematosus, rheumatoid arthritis and some other rheumatic diseases. These diseases are characterized by characteristic features of extra-cardiac manifestations. In systemic lupus erythematosus, specific immunological phenomena are detected - antibodies to DNA and other nuclear substances. 4. Idiopathic mitral valve prolapse. In this disease, most patients have an asthenic type of Constitution and phenotypic signs indicating congenital connective tissue dysplasia (funnel-shaped chest deformity, scoliosis of the thoracic spine, joint hypermobility syndrome, etc.). A thorough analysis of the clinical features of extra-cardiac manifestations of the disease and Doppler echocardiography data help to make the correct diagnosis. Endocarditis is characterized by variability of the auscultative picture. 5. Infectious endocarditis. Febrile syndrome in infectious endocarditis, unlike ORL, is not completely stopped only by the appointment of NSAIDs, destructive changes in the valves quickly progress, and the symptoms of heart failure increase. When conducting an Echo found on the valves of the growing season. Characteristic is the allocation of positive hemoculture. Green streptococci, staphylococci and other gram-negative microorganisms are verified as pathogens. 6. Tick-borne migrating erythema. It is a pathognomonic sign of early Lyme disease. Unlike anular erythema, it is usually large (6-20 cm in diameter). In children, it often appears in the head and face, occurs with itching and burning, regional lymphadenopathy. 7. PANDAS Syndrome. In contrast to rheumatic chorea, this syndrome is characterized by the severity of psychiatric aspects (a combination of obsessive thoughts and obsessive movements), as well as a much faster regression of symptoms of the disease against the background of adequate anti-streptococcal therapy alone. Management of Acute Rheumatic Fever 1. Bed Rest: All children may sit up in bed and feed themselves from the day of admission. The duration of bed rest can be as follows: Cardiac Status Duration of Bed Rest No Carditis (arthritis only) Carditis with no failure Carditis with heart failure Bed rest for 2 weeks and gradual ambulation for 2 weeks even if on salicylates. Eed rest for 4-6 weeks and gradual ambulation for 4-6 weeks. Strict bed res~ for as long as heart failure is present and gradual ambulation for 3 months. 2. Eradication of streptococcal infection : The child should receive an intramuscular injection of 400,000 I.U. procaine penicillin daily for 10 days. Patients who are allergic to penicillin can be given oral Erythromycin in a dose of 50 mg/kg/day in 4 divided doses for 10 days. This should be followed by either: a) Long acting penicillin ( 1,200,000 I.U.) called Benzathine penicillin The dose is taken every 2 weeks. b) One tablet of Sulfadiazine (0.5 gram) for those under 25 Kg daily. Two tablets of sulfadiazine (1 gram) for those above 25 Kg daily. This schedule is followed in patients who are allergic to penicillin. 3. Pathogenetic treatment: (A) Cases without cardiac involvement: are given salicylates as follows: - 100 mg/kg/day for the first two weeks, followed by: 75 mg/kg/day in four hourly divided doses (5 times/day) to maintain a blood level of 25 — 35 mg/dL for the following 4 - 6 weeks. (B) Cases with evidence of cardiac involvement are given Steroid therapy: Prednisone is started in з dose of 2 mg/kg/day in divided doses. After about 2 weeks prednisone may be gradually withdrawn, decreasing the daily dose by one tablet ( 5 mg) every 3 days. When tapering is started , Salicylates should be added and continued for one month after prednisone is stopped (dose of salicylates: 75 mg/kg/day). 4. Treatment of heart failure: (a) Mild heart failure can.be controlled by complete bed rest, Oxygen, fluid restriction and steroids. (b) In severe heart failure, diuretics and digitalis are indicated. These children are susceptible to digitalis toxicity, therefore smaller doses than usual must be given. If digitalis is administered potassium is given as well (KC1 2.4 mg/day for those less than 27 kg and 3.6 mg/day for those over 27 kg). (Revise treatment of heart failure later on). 5. For Rheumatic Chorea: Steroids and salicylates are not given unless there are also -signs of active rheumatic inflammatory process. Haloperidol (Haldol) in a daily dose of 1 - 6 mg in divided doses can be given to control the involuntary -movements and agitation. Some patients benefit from barbiturates or chlorpromazine. Prevention of Rheumatic Fever: Rheumatic fever is a recurrent disease which frequently can be prevented. Infection with group A beta hemolytic streptococci precipitates both initial and recurrent attacks; therefore prevention of rheumatic fever and rheumatic heart disease depends upon the control of streptococcal infection. This may be accomplished by : 1. Primary Prevention: by early adequate treatment of streptococcal infection in all individuals. 2. Secondary Prevention: for prevention of recurrences through the prevention and treatment of streptococcal infection in rheumatic subjects. Rules of secondary prevention: a. It should be initiated as soon as the diagnosis of rheumatic fever is made by the long acting penicillin as mentioned before. b. It should be given to all patients who have a well documented history of rheumatic fever or chorea or who show a definite evidence of rheumatic heart disease. c. The long acting penicillin (or sulfadiazine) should be given continuously (winter and summer). d. The prophylaxis should be continued for life. However, it has been recommended by the World Health Organization that prophylaxis should be given for at least 5 years after the last attack of rheumatic fever. Specific Prophylactic Measures: (A) Benzathine Penicillin: an IM injection of 1,200.000 I.U. of long acting penicillin every 2-3 weeks was found to be the most effective prophylactic measure. Penicillin rarely produces allergic reactions. These include urticaria, and angioneurotic edema. Reactions similar to serum sickness with fever and joint pains may occur arid may be mistaken as rheumatic fever. A careful history of allergic reactions to penicillin should be obtained. It is safer not to use penicillin if the reaction has been severe and especially if angioneurotic edema has occurred. (B) Oral Penicillin: is also effective in a dose of 200,000 units twice daily. Its drawbacks include: a. Failures occur frequently in patients who are not compliant or who forget to ingest the drug regularly. b. Oral penicillin causes emergence of resistant strains of alphastreptococci in the oral cavity, a potential hazard for patients with raeumatic heart disease since they are at risk for bacterial endocarditis. (C) Oral Sulfadiazine: from 0.5 - 1 mg (1 - 2 tablets) once a day. The smaller dose is to be used in children under 25 kg. The main toxic reactions include: a. Morbiliform skin eruption: the drug can be continued cautiously. b. Urticaria or scarlitiniform rash associated with sore throat or fevers are indicators of discontinuing the drug. c. Leucopenia: discontinue the drug if the blood count falls below 4000 and polymorphs fall below 35% because of possible agranulocytosis which is often associated with sore throat and rash. Because of these reactions, weekly WBCs counts are advisable for the first two months of prophylaxis.