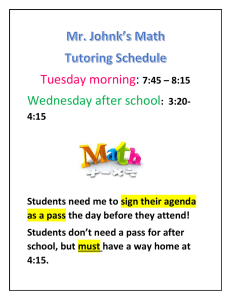
CONTRACEPTION Associate Professor Dr Hanifullah Khan Objectives 1. Understand the definition, classification & terminology 2. Understand the reason for contraception 3. Know the advantages & side-effects 4. Know the proper use of each method 5. To be able to advise on the use Introduction • Definition – any method used to prevent pregnancy 19 May 07 • Allows to choose whether & when to have a child 3 Reproduction • Ovulation • Fertile period • Fertilisation 19 May 07 4 Consequences of unintended pregnancies - fetus • Late booking or no booking. • Fetus more likely to be exposed to harmful substances (smoking tobacco and drinking alcohol). • The child is at greater risk of – weighing < 2.5kg at birth – of dying in its first year of life – of being abused – of not receiving sufficient resources for healthy development. Cleland NEJM 2011 5 Consequences of unintended pregnancies - mother • Late booking or no booking – increased antenatal risks • The mother may be at greater risk of physical abuse • Her relationship with her partner is at greater risk of dissolution. • Both mother and father may suffer economic hardship and fail to achieve their educational and career goals. October NEJM Cleland 2003 2011 6 Reproductive age • The typical woman - capacity to bear children for an 39 years of her life • Different contraceptive methods required for each life stage – to accommodate the complex factors accompanying each stage • Without contraception - 85% of couples conceive within 1 year. Trussell J. Contraception 2010 Female Contraception Reversible Non-Reversible Hormonal Tubal ligation Non-Hormonal COC IUD POP Barriers POP Spermicides Injectables Implants Emergency Mirena 7 June 2006 8 COMBINED CONTRACEPTION Combined Oral Contraception I • Large number of users • Prompt return of ovulation – 70% in 1st cycle , 98% by 3rd cycle* • No permanent loss of fertility • Beneficial effects on future fertility – ↓ ascending infection & PID (progestogenic effect) – ↓ risk of EP – ↑ ferritin levels & Hb *Rice-Wray E et al. Return of ovulation after discontinuation of oral contraception. Fertil Steril 1967;18:212-8. Combined Oral Contraception II • Women who conceive after discontinuation of COC: – No ↑ risk of pregnancy loss or EP – No alteration in sex ratio • No ↑ miscarriage rate or chromosomal abnormalities in women who continue COC during early pregnancy* • No risk of masculinization *Huggins GR. Fertility after contraception or abortion. Fertil Steril 1990;54:559-73. Patch • Transdermal supply of 750 µg ethinyl estradiol (an estrogen) and 6000 µg norelgestromin (a progestin) • Side effects similar to COC • ? Slightly increased risk of TED PROGESTOGEN ONLY CONTRACEPTION Progestogen-only Methods POP ● Subdermal implants ● Injectables ● Combined injectables ● Emergency contraception ● Mirena ● Progestogen-only Methods Of Contraception* Route of administration Very low dose Oral Progestogen-only pill Subdermal High dose Etonogestrel-releasing implant (Implanon®) Levonorgesterelreleasing implant (Norplant®) Intrauterine Levonorgesterelreleasing intrauterine system (Mirena®) Vaginal Vaginal rings (under development) Intramuscular injection Low dose DepoProvera® POP - Effects • Local effect on cervical mucous & endometrium – inhibits gamete transport & implantation • No effect on future fertility • Does not offer same protection against EP as COC Subdermal Implants • Implanon – single rod. Between biceps & triceps of non-dominant arm. – 3 year efficacy. – Inhibits LH surge – ovulation inhibition – Oestradiol levels unchanged – The only contraceptive method to have a Pearl Index of 0.* – Prompt return of fertility* • Norplant – older. 6 rods. *Croxatto HB. The pharmacodynamics and efficacy of Implanon. An overview of the data. Contraception 1998;58:91S-97S. Implanon Injectables • DMPA • Inhibition of ovulation caused by Gn suppression • Ovulation returns after 4-5 months & median conception time of 5-7 months* • No permanent effect on fertility. However, may take 2 years to return.** • Delay may be due to slow drug metabolism (microcrystalline deposits in muscle)*** *Kaunitz AM. Ob/Gyn 1993 ** Kaunitz AM. Int J Fertil Womens Med 1998 ***Hickey M. Clin Obstet Gynecol 1995 Emergency contraception I • ECP/ "morning-after pills • a short course – – – either a high-dose combination of estrogen & progestin or progestin-only used within 72 hours of unprotected intercourse to prevent pregnancy • taken after SI but before implantation • more effective the sooner they are initiated after SI. • estrogen-progestin combinations (commonly known as the Yuzpe regimen) – may reduce the risk of pregnancy by 75% and the progestinonly formulation by 88% EC IUCD • copper-containing intrauterine device (IUD) inserted within 120 hours of unprotected intercourse to prevent pregnancy • work by the same mechanisms of action as OC inhibit ovulation, fertilization, or implantation. • They will not terminate an existing pregnancy Emergency Contraception III Levonorgestrel 0.15 mg +ethinyl estradiol 30 mcg Nordette (light orange tablets) 4 tablets/dose 2 doses Levonorgestrel 0.75 mg Plan B 1 tablet/dose 2 doses First dose within 72 hours of unprotected intercourse; second dose 12 hours later(no anti-emetic required) NATURAL METHOD Wednesday 15 23 Body changes during menstruation • Likelihood of pregnancy high if SI just before or after ovulation • During the menstrual cycle, a number of changes occur in a woman's body – By keeping track of these changes, couples can plan when to have intercourse and when to avoid intercourse, depending on whether they are trying to achieve or avoid pregnancy. Wednesday 15 24 What is natural family planning? • A way to help decide when SI can or cannot result in pregnancy • Learn to recognise the changes in a woman’s body that shows when she is fertile each month • Avoid sex at the fertile times, or use condoms or a diaphragm. Wednesday 15 25 Advantages: • • • • • Acceptable to most faiths and cultures No need to take any hormones No side effects Gives a greater awareness of fertility Can be used to plan pregnancy as well as avoid it Wednesday 15 26 Disadvantages • • • • • No protection against STIs Takes a long time to learn (3 to 6 months) Daily tests and records need to be made Illness, stress and travel can affect fertility indicators Both partners need to be committed to using the method • Unsuitable for: – – – Women who can't check their temperature and cervix every day Couples who are even slightly disorganised Women with very irregular periods Wednesday 15 27 Methods • Coitus Interruptus • Rhythm Method – – – – – Calendar BBT Cervical Mucous (Ovulation) Symptothermal Ovulation Predictor Kits • Abstinence • Lactational Amenorrhoea Method Wednesday 15 28 Coitus Interruptus Wednesday 15 29 Coitus Interruptus (Withdrawal) • The penis is withdrawn from the vagina prior to ejaculation • When done correctly - failure rate of 6.7% (6.7 out of every 100 women) • Advantages - immediately available and it is free • Disadvantages – unsure able to withdraw before ejaculating – preejaculatory fluids may contain viable sperm Wednesday 15 30 Effectiveness Among typical couples - 19 in 100 will experience an accidental pregnancy in the first year o Some men cannot tell when they are going to ejaculate. o Some men ejaculate very quickly, before they realize it. o Before ejaculation, almost all penises leak fluid that contains sperm that can cause pregnancy. o Some men lack the experience and self-control to pull out in time. o Some men are unreliable o It offers no protection against STD's and infections. o It's free Wednesday 15 31 Rhythm Method Wednesday 15 32 What is it? • Also known as "fertility awareness" • Uses the menstrual cycle to predict the most fertile time of the month . • Once the fertile time has been identified - don't have sex or use a barrier method during that period. Wednesday 15 33 How does it work? • Based on the fact that: – The fertile period lasts about 4 days following ovulation, when the mature ovum travels through the fallopian tubes to the uterus and can be fertilized • Sperm may live in the female reproductive tract for up to 7 days • The female egg lives for only a day • fertilization may occur even days after intercourse • "safe days" occur 2 days after ovulation and continue until the next period Wednesday 15 34 How effective is it? • Choose a fertility awareness method only if: – There is a cooperative partner – A regular, steady monthly cycle – Willing to invest time and effort required to learn about fertility awareness methods – accept the fact that protection against pregnancy is not perfect • There are no side effects Wednesday 15 35 Several Methods • Several methods of determining which are the most fertile days of the cycle: – Calendar Rhythm Method – Basal Body Temperature Method – Ovulation Method – Symptothermal Method – Ovulation Predictor Kits Wednesday 15 36 Calendar Rhythm Method • Requires keeping track of the cycle for 6 to 12 months to determine the pattern of ovulation -will determine when it is most "dangerous" to have sexual intercourse. • Estimate the first and last days of the fertile period – subtract 18 from the length of the shortest cycle and 11 from the length of the longest cycle – if the shortest cycle is 28 days and her longest cycle is 32 days, the first and last days of the fertile period should be days 10 and 21 – should abstain from SI for 12 days, starting on the 10th day after the beginning of the menstrual cycle • The failure rate for this method is 40% (40 out of 100 women). Wednesday 15 37 Shortest cycle (S) minus 18 = Last infertile day of the pre-ovulatory phase Longest cycle (L) minus 11 = Last fertile day For example:Length of cycles during last six months = 28, 29, 28, 27, 30, 28 (S = 27) S - 18 = Last infertile day 27 - 18 = 9 (L = 30) L - 11 = Last fertile day 30 - 11 = 19 Wednesday 15 38 Basal Body Temperature Method • Keeping track of body temperature • Body temperature rises two days prior to ovulation. Wednesday 15 39 RECORDING & CHARTING THE BBT • The temperature should be taken immediately on waking before getting out of bed, drinking tea or any other activity, and at about the same time each morning Wednesday 15 40 THERMOMETERS • Two types of thermometer – Glass / mercury fertility thermometer – Digital thermometer • covers only the range from 35-39 deg. C Wednesday 15 41 Ovulation (Billing) Method • Requires feeling and observing the cervical mucus to determine the time of ovulation. • Note the production of clear, watery mucus in the days immediately before ovulation • To avoid pregnancy, intercourse is avoided for several days following change in the color and consistency of cervical mucus. Wednesday 15 42 Changes in the Cervix - in Relation to Ovulation Cervical changes take place over an interval of around 10 days. Approximately 6/7 before the shift in temperature the cervix will begin to show fertile characteristics. Following ovulation, the cervix returns to its infertile state within 2448 hours Wednesday 15 43 RECOGNISING THE CHANGES IN CERVICAL MUCUS • Sensation - at the vulva :the sensation may be a distinct feeling of dryness, of dampness or moistness, stickiness, wetness, slipperiness or lubrication. • Appearance – use toilet tissue to blot or wipe the vulva white, creamy, opaque, or transparent (clear). – Mucus is often noticed on underclothing, where it will have dried slightly causing some alteration in its characteristics • Finger Testing - finger-tip applied to the mucus on the tissue and then pulled gently away to test its capacity to stretch – – It may feel sticky and break easily or it may feel smoother and slippery like raw egg white and stretch between the thumb and first finger, from a little up to several inches before it breaks. This stretchiness is described as the Spinnbarkeit or Spinn effect, and shows that the mucus is highly fertile. Wednesday 15 44 Sensation at Vulva Finger Test Appearance Moist or Sticky Early Mucus Scanty Thick White Sticky Holds its shape Wetter Transitional Mucus Increasing Amounts Thinner Cloudy Slightly Stretchy Slippery Highly Fertile Mucus Profuse Thin Transparent Stretchy (like raw egg white) Wednesday 15 45 Mucus changes throughout the cycle Complete cycle showing typical pattern of menstruation, preovulatory dry days, mucus days with increasingly fertile characteristics approaching peak day, the abrupt change back to less fertile characteristics, the count of four after peak day and post-ovulatory dry days Wednesday 15 46 Symptothermal Method • A combination of the calendar and cervical mucus methods and the woman's basal body temperature (BBT) • The first day is estimated by subracting 21 from the shortest menstrual cycle (the calendar method) or noting the first day of cervical mucus associated with ovulation (the cervical mucus method), whichever comes first • BBT is used to predict the end of the fertile period. The woman takes her temperature every morning and notes when body temperature rises, indicating that the corpus luteum is producing progesterone and ovulation has occurred • She can resume sexual intercourse 3 days after this so-called thermal shift Wednesday 15 47 Interpretation of the Sympto-Thermal Chart This sympto-thermal chart shows the correlation between all indicators of fertility Wednesday 15 48 Fertility Chart Wednesday 15 49 Ovulation Predictor Kits • used to test urine to identify hormones that indicate ovulation is about to occur • electronic fertility computer tells a woman which days she is fertile • Persona: fertile days are indicated with a red light and infertile days with a green light • failure rate as low as 6% among women who abstain on fertile days as indicated by the device Wednesday 15 50 Anovulation • A monophasic chart indicates that there has been no ovulation in this cycle. • The temperature remains on one level. • The bleed, not a true period, is often lighter than usual. Wednesday 15 51 Faulty technique • Erratic temperature chart - result of poor technique. • Implications of disturbances, such as illness, alcohol, medication, or disturbed sleep patterns and note their occurrence. • A temperature chart showing erratic and abnormally low readings usually indicates faulty technique. Wednesday 15 52 Abstinence Wednesday 15 53 Easily stated, not always easily done • takes commitment from both partners • Abstinence is the most effective method of preventing pregnancy and transmitting sexual disease • Not having traditional sexual intercourse, so the penis does not enter the vagina, at all • Become familiar with the fertility patterns - abstain from vaginal intercourse on the days pregnancy can occcur • Effectiveness - If practiced perfectly, there should not be any pregnancy. Wednesday 15 54 Pros and Cons • The Pros – – – – – – – 1) Anyone can do it, with commitment. 2) It's free. 3) Encourages the building of a relationship. Trust. 4) No supplies 5) No infections or STI's 6) Endorsed by some religions. 7) No hormonal side effects. • The Cons – – 1) It can be frustrating for some couples. 2) If not used properly, infections can be acquired. i.e. oral sex transmission. Wednesday 15 55 Lactational Amenorrhea Method Wednesday 15 56 LAM • Average Failure Rate: 6% • Most BF women do not ovulate for 4-24 months postpartum – whereas non-breastfeeding women can ovulate as early as 1-2 months • Conditions to be fulfilled – – – Fully BF No periods Recommended up to 6 months - the longer LAM is used, the more likely it is that ovulation will precede the first menses • Cervical mucus changes herald the first ovulation – should start checking daily at six weeks postpartum • Women with no periods who BF without practicing LAM - pregnancy rate of 6% over a year. Perfect users can expect a failure rate of only 0.5%. Wednesday 15 57 What are the advantages of natural family planning? • Does not involve the use of medicines, mechanical devices or chemicals. – Side effects or risks that may occur with the use of such medicines or devices will not occur • Inexpensive • Require partners to share the responsibility for planning or avoiding pregnancy – Typically, couples who use these methods notice an increase in communication and in cooperation. Wednesday 15 58 INTRAUTERINE DEVICES Introduction a small device made of plastic or copper that is placed into the uterus as an effective method of contraception 60 19 May 07 Types Levonorgestrelreleasing device 19 May 07 Copper-releasing device 61 Copper IUDs: Mechanisms of Action Interfere with ability of sperm to pass through uterine cavity Thicken cervical mucus Interfere with reproductive process before ova reach uterine cavity Change endometrial lining IUDs: Contraceptive Benefits • Highly effective • Effective immediately • Long-term method (up to 10 years protection with Copper T 380A) • Do not interfere with intercourse • Immediate return to fertility upon removal • Do not affect breastfeeding 1 Trussell et al 1998. 19 May 07 63 IUDs: Contraceptive Benefits continued • Few side effects • After followup visit, client needs to return to clinic only if problems • No supplies needed by client • Can be provided by trained nonphysician • Inexpensive (Copper T 380A) 19 May 07 64 IUDs: Noncontraceptive Benefits • Decrease menstrual cramps (progestin-releasing only) • Decrease menstrual bleeding (progestinreleasing only) 19 May 07 65 Who Can Use IUDs Women of any reproductive age or parity who: – Want highly-effective, long-term contraception – Are breastfeeding – Are postpartum and not breastfeeding – Are postabortion – Are at low risk for STDs – Cannot remember to take a pill every day – Prefer not to use hormonal methods or should not use them – Are in need of emergency contraception 19 May 07 66 IUDs: Who Should Not Use (WHO Class 4) IUDs should not be used if woman: – – – – – – – – Is pregnant (known or suspected) Has unexplained vaginal bleeding until the cause is determined and any serious problems are treated Has current, recent PID Has acute purulent (pus-like) discharge Has distorted uterine cavity Has malignant trophoblast disease Has genital tract cancer Has an active genital tract infection (e.g., vaginitis, cervicitis) Source: WHO 1996. 19 May 07 67 IUDs: Common Side Effects Copper-releasing: – – – – – Heavier menstrual bleeding Irregular or heavy vaginal bleeding Intermenstrual cramps Increased menstrual cramping or pain Vaginal discharge Progestin-releasing: – Amenorrhea or very light menstrual bleeding/spotting 19 May 07 68 IUDs: Possible Other Problems • Missing strings • Slight increased risk of pelvic infection (up to 20 days after insertion) • Perforation of the uterus (rare) • Spontaneous expulsion • Ectopic pregnancy • Spontaneous abortion • Partner complains about feeling strings 19 May 07 69 IUD Insertion: Withdrawal Method (2) Withdraw inserter tube (1) Hold plunger Source: PATH and Population Council 1989. 19 May 07 70 Postpartum insertion • Delayed (4-6 weeks) or immediate postpartum insertion • safe and effective • Expulsion - more common for immediate than with interval insertions 19 May 07 71 Postabortal insertion • • • • Safe and practical Convenient Avoid some discomfort from the procedure Expulsion of the device is marginally increased 19 May 07 72 Benefits of IUDs • Long-acting reversible contraceptives • Require no adherence on the part of the user – leaving virtually no scope for user error • More than 99% effective • Once they’ve been inserted, users need not take any action to continue using them – Reduce the number of unintended pregnancies that are due to user error or contraceptive failure. • Exceptionally cost-effective. Trussell J. Contraception 2010 CURRENT CONCEPTS IN CONTRACEPTION Guidelines Regarding the Use of Combination Estrogen-Progestin Contraceptives in Women >=35 Years of Age, According to Risk Factors Kaunitz A. N Engl J Med 2008;358:1262-1270 Breast feeding • Previously, progestin-only • Low dose COC still possible 19 May 07 76 Cancer risk • Long term – • If used for more than a protect against Ca year – protect against Ca ovary endometrium • Ca breast? uncertain • Those with Ca breast should not take pill Failure Rates User Failure 19 May 07 Method Failure 78 Failure rates • • • • • • • Implants, IUDs and LNG-IUS - <1% Contraceptive pills - 5% Male condoms - 14% Diaphragm with spermicide - 20% Cap with spermicide - 20-40% 'Natural' methods - 35% Withdrawal - 19% 19 May 07 79 1. Contraception provides an effective means to plan a family 2. Many methods are available suitability has to be decided based on a proper history & examination 3. Pregnancy should be ruled out first 4. You should know the advantages & side effects 5. Contraception also provides non-contraceptive benefits KEY POINTS Further reading • Cleland et al. Family Planning as a cost saving preventive health service. NEJM April 20, 2011. • Trussell J. Update on the cost effectiveness of contraceptives in the United States. Contraception 2010;82:391.