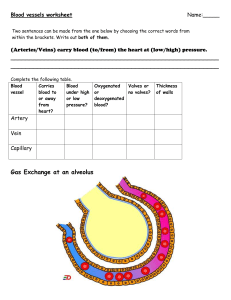
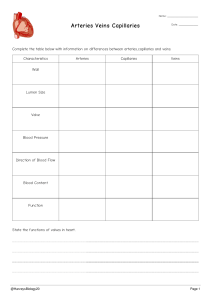
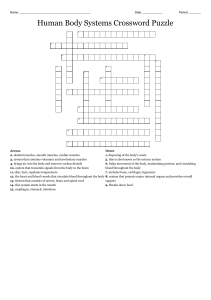
Week 7 Class notes Week 7 Class notes for cardio Adrenergic receptors are for adrenal glands Alpha 1: respond to epinephrine and NE (norepinephrine) , have alpha 1 : responds to chemical signals by increases activity excitatory, found on radial muscles of iris, for pupil dilation, on sweat glands to increase sweating, on smooth muscles of the blood vessels on periphery of Gi vasodilation AND THE HEART to increase RATE of contraction (tachycardia). Stimulation of these receptors mimic the SNS. BUT effect lasts a bit longer bc it’s a hormone Alpha 2 : inhibitory : only located on glands of GI tract, circulatory muscles in walls of GI, reduce GI secretions and reduce GI peristalsis. (SNS effects). because they have inhibitory effect when stimulated because the NE of the SNS is acting in a inhibitory way Beta: respond ONLY to Epinephrine, NE has no effects Beta 1 increase activity, increase vasodilation of heart and increase renin excitatory, located in two main areas – kidney where they stimulate renin secretion renin angiotensin system. W/ renin there is : stimulate increase angiotensin so vasoconstriction, sodium reabsorption and increase blood volume (bc of aldosterone increase) angiotensin and they are also on the heart muscles, they cause increase in STRENGTH reaction. Beta 2 inhibitory. Found on the smooth muscles of the walls of certain BV i.e. heart and skeletal muscles. Causes VASODILATION bc it inhibits smooth muscles – muscles don’t contract and there’s increase blood flow to heart and skeletal muscles. and its also on smooth muscles on Bronchi and bronchioles which causes the muscles to relax and u get bronchodilation and increases air flow to and out of the lungs. If you have a drug that stimulates the same effects as a neurotransmitter/hormones they are called AGONIST for alpha 1 and beta 2 (something that promotes the same effects) i.e. taking epinephrine as a drug and it would act on the heart to increase its speed/heart rate, so this is an agonist. Can also lead to bronchodilation (acts on beta 2) and vasoconstriction peripherally by acting on alpha 1 receptors. Epinephrine can treat anaphylaxis shock bc it acts on alpha 1 to raise blood pressure and beta 2 to open airway (bronchodilation) ANTAGONIST/BLOCKERS (cock blockers) : i.e. beta blockers, beta.1 blocker used for heart failure because it will reduce renin secretion and less angiotensin in turn it will reduce blood pressure and stop heart muscles from contracting so that heart can meet its own needs for blood flow. Review: lipid metabolism Lipids are in your diet, when they are eaten and get to the gut the bile breaks it up into smaller pieces and lipase comes digest into smaller components and it gets absorbed to gut wall in small intestine. you have microvilli (folds in gut wall) in the middle of each microvillus you have a lacteal The Lipids diffuse through membranes to the lacteal lymph and combined with proteins to form chylomicron (lipoproteins) and this is a little protein which can flows through lymph then goes to subclavian vein reaches circulation and spreads along body. so, chylomicrons are transport vehicles when they get to adipose tissue chylomicrons will release its fats (some) and get to the liver. When it reaches liver (most lipid processing is here) they’re then packaged in specific ways, liver makes VLDL very low-density lipoprotein bc high lipid/fat content and low protein content. liver will be released into blood and fats will be transported and given to adipose tissue. As they lose their lipids top adipose tissue they then become LDL (low density lipoprotein.) they deliver lipids to your tissues/circulate the blood all the time. HDL : higher protein content low fat. produced by liver to go and get lipids from tissue and bring to liver ( HDLs like cops and LDLs are bad guys) so there isn’t a lot of LDL;s in the body. Liver either eliminates via bile or recycles/reuses it. high LDL and low HDL you’re in trouble, it will increase the risk of atherosclerosis. You don’t want super low LDL/HDLS. to get LDLS up you eat high far, salt, sugar/processed foods. . Lower LDL by having lots of protein-based foods?? HDL: sit around all day, less physical activity more u have, and you won’t have any but if you exercise you can raise your HDLS’S proteins are denser than the lipids Artery Is vessel, carried blood from heart tissues, high pressure bc its soon after the heart and pulsed bc heart is diastole, systole etc. Artery Characteristics To adapt arteries, have specific characteristics, endothelial lining outside, smooth muscle, connective tissue. So, arteries have more smooth muscle to control pressure and downstream flow. have LOTS of elastic connective tissue so artery can stretch during ventricular systole and recoil during diastole. ARTERIOLES have a smoother muscle than arteries Atherosclerosis Build-up of fatty deposit (plaque) on inside surface of artery. Common : large arteries Mechanical causes can even be hypertension, strokes, can’t reverse it. How it happens: tissue will become inflamed/swollen and macrophages will be attracted and start to respond to tissue damage. if there’s high LDL levels they will deposit the lipids INTO the macrophages (foam cells) and they will form a plaque on the surface that’s inflamed, and a foreign surface happens. You’ll provoke other chemical mediators and smooth muscle will form over the foam cells. It’ll keep happening and get bigger (now called atherosclerotic plaque/atheroma Patho: High levels of oxygen reactant SPECIES (ROS) Combine with molecules and alter them. Smoking LEADS TO HIGH LEVELS OF ROS as the chemicals get absorbed thru the lung walls into the blood. 1. 2. 3. 4. Effects of plaque will restrict blood flow will be narrow/shallow and there will be a turbulent flow will lead to increased risk of thrombus formation. decreased downstream flow to tissues. Decreases forward flow which leads to a resistance to flow and a backup of pressure. Increased PVR Increased system blood pressure. Weakens the artery walls causes two main issues. arterial sclerosis where you lose elasticity and it will raise your BP and systolic pressure ? and increased risk of aneurisms common in aorta/cerebral artery (like large arteries) and branches of large arteries i.e. circle of Willis. Barry aneurysm bulges out. Turbulent flow with aneurisms and increases risk of clots, as it expands it can compress adjacent tissue so the airway, heart or part of the brain as it expands out. It could always rupture, and you will bleed out large volumes of blood and death can occur unless you’re in the hospital Major cause of strokes, hypertension etc. once you have this it’s hard to eliminate, with exercise and diet change you will prevent FURTHER damage but its irreversible. Coronary artery disease is just atherosclerosis in coronary arteries Aneurisms Are weakened walls, can have atherosclerosis, infections like treponema, the pathogen that causes syphilis , physical trauma. Places to get them : aorta arch, places with large arteries and large branches i.e. circle of wilis. like cerebral/aorta aneurisms. WALL bulges out Three Types: Barry: wall bulges out Saccular common, elongated wall Disectular : damage to the wall where if there’s a tear it will allow fluid to leak between the layers. + This can be moved/ split open. Cause of aneurisms 1. 2. 3. 4. Hypertension, weakens cell wall by atherosclerosis, physical trauma by damaging walls in surgery syphilis infection (sexually transmitted disease) as it attacks blood vessel walls and it can pass the BBB and get into the brain. With syphilis you’ll get a canker in the genital region – damp skin surfaces during intercourse the pathogen can move and now you will get a canker. it will form a scab and fall off and now it’s in your bloodstream. Artery: vessel carries blood from heart to tissues, high pressure and pulsed bc its soon after the heart and follows the flow of the heart. all BV except capillaries have endothelial lining, connective and smooth muscle tissue. arteries have a high amount of smooth muscle to control vasoconstriction/vasodilation. in their connective tissue layer, they have lots of elastic tissue, this allows artery to stretch during systole and recoil during diastole. Veins don’t directly receive blood, goes through artery, arterioles, then to capillary beds. the pressure in veins are low and non-pulsated, (so smooth, low pressure flow). they have very little smooth muscle and elastic tissue. blood flows through veins via skeletal muscle pump when muscles contract/ get shorter, the muscles bulge in the middle, raise pressure in vein and blood moves forward. Veins also have one-way valves to allow FORWARD flow, Pathology of veins Varicose veins where one or more of your way valves don’t work or are incompetent valve. So, the blood goes to the first competent valve it sees and it will cause the vein to bulge, and the vein will bulge out because the blood will go back to the working valve. issues of varicose veins: stasis of blood inside vein = above competent one-way valve so it can clot, doesn’t allow forward flow so blood pressure is being raised. blood clot risk increases, high hydrostatic pressure at venous end of capillary and now less fluid will come from ISF back into the blood AND bc osmotic pressure is low. So, edema bc of the fluid retention ISF irritating vessel walls so inflame walls (itchy/painful) reduced venous return to the heart. Risk factor: Common in people who stand upright I one place or sitting in one place. Risk for nurses, office workers. genetics, if you have less skeletal muscle mass, aging \ Pregnancy will compress inferior vena cava and back up venous flow in lower body, also progesterone levels which cause smooth muscle relaxation in veins. Treat: physical exercise, contract your muscles to reduce likelihood, lie down and elevate legs to reduce blood accumulation, put on support hoes before you stand up, don’t wear tight elastic clothes issue with varicose veins are thrombus formation THROMBOPHLEBITIS clots forming in veins as result of inflammation in veins. So when u have varicosities the inflammatory tissue changes and the clot will form and bind with that inflamed tissue, more likely to stay in place here PHLEBOTHROMBOSIS clots form in veins due to inactivity (like being on an airplane for long) or hyperkalemia , excess vit D or dehydrated will increase likelihood of clotting factors. ISSUE is its more likely to be released via circulation because it won’t be held by the inflammatory tissues will get to the right side of the heart , top pulmonary arteries from right ventricle and into pulmonary arterioles and will block the pulmonary circulation where pulmonary arterioles are. PULMONARY EMBOLISM can lead to resp issues and right-side/left side failure Pathophysiology Nov. 12 Class notes Review: heart 4 chambers but two sides are separate pumps RS receives via inferior vena cava and pumps via pulmonary arteries and pumps to lungs LS receives blood from lungs and pumps out through systemic loop, LS is larger than the right, two sides pump at the same time. Left ventricle larger than the rest 4 Valves 2 atrioventricular valves one on right- tricuspid valve LS- mitral/bicuspid valve. 2 semilunar valves that open into pulmonary artery and the aorta. All one-way valves purely mechanical, all valves prevent backflow. Cardiac cycle: bc two sides are working at the same time both atria contracts (atrial systole) ..blood forced through the AV valves into ventricles and then the ventricles contract and also the AV valves shut, open semilunar valves and allow the semilunar valves into the arteries. Cardiac reserve muscles that contract 24/7 can contract faster and harder when they need to for ex. you can change your cardiac output. typical CO is 5L/min what would happen is you could potentially pump out 20-25L/min so your cardiac reserve is 4-5X what your typical CO is on average. (not true for everyone) Its usually states as a present. i.e. CO 250% One things we measure to see if CO is declining CO: amount of blood the heart pumps out per min. A result of 1. HR, so how often it pumps typically 70bpm 2. Stroke volume: amount ejected PER contraction so HR X STROKE VOLUME= CO stroke volume: determined by 1. amount of venous return, how much blood is coming into the heart, causes stretching of heart muscles and that will increase strength of contraction. 2. Strength of contraction.( STARLINGS LAW: more that goes into the heart, more chamber walls stretch and harder heart contracts) and the strength of contraction: Beta 1 receptors can also make heart contract harder. K,Ca can affect it too. Terms: preload amount of blood entering a chamber and stretches it, more it is harder heart muscles have to work. What can increase preload : 1. increased venous return: running to catch. bus your skeletal muscles are contracting more in ur veins and via inferior VC it will increase blood u get to the heart. 2. If your BV goes UP i.e. blood transfusion. consume a lot of fluids, increase aldosterone Incompetent Valve that can cause regurgitation of blood back since it does not close completely some of the blood you pumped forward will come back. Similar thing can happen with incompetence of AV valve, the blood will come back into the atria instead of all into artery and when ventricle relaxes it’ll all come back and stretch more. afterload pressure AGAINST which the heart must pump. High pressure in those vessels to get blood to flow you have to overcome those pressures. What affects it: anything causing hypotension Atherosclerosis : narrows the lumen of arteries, increases peripheral vascular resistance and your afterload increases BP TOO vasoconstriction: usually after stress response. Valve stenosis : narrow valve maybe has been damaged by infection and makes it harder for blood to flow out through that valve. your ventricles have to pump harder to get blood past it. If its increased, the workload of the heart is also increased. Coronary circulation blood flow thru heart muscles. anterior DESCENDING SUPPLIES ANTERIOR OF BOTH VENTRICLES . CIRCUMFLEX SUPPLIES THE LEFT ATRIUM AND LATERAL LEFT VNENTRICLES BRANCHES OF IT SOMETIME FORM POSTERIOR DESCENDING ARTERY POSTERIOR DESCENDING ARTERY SUPPLIES POSTERIOR OF BOTH VENTRICLES CORONARY ARTERY is partially blocked during ventricular systole but semilunar valves close when contraction and high blood in aorta flows into the arteries . MOST CORONARY BLOOD FLOW DURING VENTRICULAR DIASTOLE. pic on ipad Opening of Left and right vein are immediately over semilunar valves, so when they are forced open they partially block coronary circulation so in ventricular systole very little blood flows in but when they close the blood can flow. Most coronary blood flow during ventricular diastole. When heart contracts the muscles compress coronary BV so blood can’t form through so little blood flow during ventricular systole. 1. doesn’t flow into and thru coronary arteries. If ventricles contract FAST a lot there’s less time available for ventricular filling, less blood flowing in your CO goes down. So with tachycardia a small amount increases your CO along with the workload for the heart but more wont increases it bc less time for filling. Coronary arteries can regulate their own local flow so a particular area might get more blood. Regulate by vasodilating, with increase workload. How is it regulated? A lot of it is similar to rest of the body, when muscles work harder more heat and carbon dioxide is generated and increase CO2 levels will increase vasodilation. also increased Hydrogen ions, K levels will do this and adenosine ( in tri/di/mono phosphates). Nitric oxide; chemical released by endothelial cells, will also cause local vasodilation (impt) NO can be raised by giving nitroglycerin and will cause coronary vasodilation quickly. Coronary artery disease : arthrosclerosis In coronary arteries. susceptible to high LDL low HDL levels. Angina: situation where heart muscles are not getting enough blood to reach demands i.e. ischemia that’s localized, and then pain responses will be stimulated by the heart muscles. Often felt in the chest below the sternum. Heart is an organ and its not well supplied with pain receptors so you will feel visceral/referred pain. The Dermatomes/area around the organ will be bundled with the actual organ pain and you will feel it somewhere else. .. so, you will feel pain even though its somewhere else. will affect LS of arms, neck, face (REFERRED PAIN). Almost a crushing/severe/burning pain in the LS. not many individuals feel referred pain or feel it on the LS might be bundled with RS. doesn’t last long usually less than 5 no more than 20. as long as ischemia is temporary no permeant damage will occur but if its more than 50-60mins the heart muscles will die. Resting will help it resolve more quickly. Main cause: Stable angina: Overtime you’ve had atherosclerosis and it has narrowed the arteries in the coronary circulation, may be no effect until you ARE 70-85% EXCLUDED OR NO S/S UNTIL U need the heart muscles to work harder. like running up a flight of stairs. Nitroglycerin/resting will help pain go away. UNSTABLE ANGINA: Thrombus formation THAT breaks off and goes downstream from larger to smaller vessel and it can completely block the vessel. lasts 30mins it can stun your heart muscles and affect your CO Variant angina: d/t vasospasm of arteries in coronary circulation, often dur to stress. With unstable angina resting/nitro won’t help When someone has angina normally they need to change lifestyle/take drugs to improve blood flow and reduce atherosclerosis as much as possible i.e. balloon angiopathy ECG/EKG: What to look for is a depressed ST segment coronary bypass, drugs-vasodilators/nitroglycerin, lifestyle and exercise (mainly) to treat this MI : heart muscle actually dies and the same factors that lead to angina lead to MI. Perceived as severe angina pain that lasts long. more pressing/extreme. Ischemia for too long 30-70 mins. Heart muscles dying If you want to know if you had a heart attack: doesn’t respond to nitro/rest but you can do ECG but this time ST segment will be elevated. (also MI can be called stemis, elevated st) or to see if MI look at intracellular isoenzymes in blood PEAK WITHIN 24-72HRS. Enzymes in blood and if you find them outside it means the cell has died and released its enzymes. two main isoenzymes: CPK creatine phospho kinine : MB which is a form that’s only found in the heart. Should not be present in the blood. CK-MB Lactic acid dehydrogenase: all cells produce it but there is 1LDH-1 in blood it means heart muscles have died. But different enzymes peak at dif times. if you miss the peak you won’t get ECG or find isoenzymes in the blood. will be a zone of necrosis and ischemia: some cells will die, and others wont and a muscle outer will recover quickly but inners wont. Heart failure: HEART IS UNABLE TO PUMP OUT ENOUGH BLOOD to meet TISSUE DEMANDS. Could be d/t heart attack, issue with cardiac conduction/ant send impulses or due to infection, like myo/pericarditis. Valve stenosis or incompetency. Might make it hard to exercise etc.. Classified as LS HF vs RS Heart failure: decreases blood flow into pulmonary circulation. forward is downstream backwards is upstream. LS failure common causes low cardiac output into systemic circulation : cardiovascular disease/ atherosclerosis which causes hypotension. Fwd. effects: reduced CO less blood flow out into the aorta decreased blood flow to skeletal muscles. where to feel effects FORWARD reduced blood to brain, so fainting, loss of consciousness, dizziness, difficulty thinking etc. Decreased flow to skeletal muscles therefore physical weakness and fatigue i.e. walking upstairs will be hard Decreased flow to kidneys- glomerular filtrate will go down, urine will go down and the __ will change bc u aren’t getting enough flow. BACKWARD: if u aren’t pumping forward ! you aren’t as able to receive blood from the left atrium or the pulmonary circulation, so the blood will “back up” the effect is going backwards bc it isn’t moving, the blood will be backed up in pulmonary circulation, pulmonary hypotension HIGH HYDROSTATIC PRESSURE LEAADS TO PULMONARY EFFUUSION AND EDEMA. also decreased gaseous exchange (listen to lecture) RS HF: increases blood flow to the pulmonary circulation? Can also be influenced by LS heart failure valve stenosis, dysrhythmia, MI. most significant is if you have respiratory disease i.e. COPD like chronic bronchitis or emphysema. In both cases mainly caused by smoking. and in the case of both there is damage to the lungs, core pulmonali RS HF due to COPD (another common cause) effects: forward effects will be less blood flow to the lungs and less gas exchange so more likely to see hypoxia or hypercapnia, might see cyanosis, (common) and decreased function of tissues SOB, fatigue bc there is less oxygen available, less blood thru lungs and less blood in LS so u can have LS heart failure. Backward effects of RS: Bc not a lot is being pumped out there’s less coming in being received from inferior and superior VenaCava so as a Sign of RSF the jugular veins distendbigger/prominent bc blood is accumulating in them and in inferior VC there can be systemic edema (or varicose veins) bc as blood accumulates it raises hydrostatic pressure at venous end of capillaries and it accumulates in the ISF, wide spread systemic edema. You have two organs that are highly distensible – liver and the spleen hepatomegaly: large liver that bulges forward bc blood can’t flow from the hepatic vein into inferior vena cava and the liver will start to swell., and your spleen where you normally store blood and normally you don’t use it but if you loose blood the smooth muscles around spleen contract so u can restore blood volume. BUT IN THIS CASE THE SPLEEN WILL EXPANS can also splenomegaly a big big spleen can burst: Explain mechanism of why they would lead to each other on a test. MANAGEMENT OF HF HF once it happens there is no going back and some people can live long with it but have decreased physical activity only a heart transplant can help. Lots of it comes from giving someone an adequate life so that they can make it to receive a heart. Mostly trying to block body’s attempt for compensating HF. bc ALL the compensation effects make HF worse. Example: will have stress response SNS will increase the heart rate even though its failing and it can’t meet demands and you’re saying “beat faster”. that increases workload and will worsen your HF other thing SNS does: widespread peripheral vasoconstriction, I raised peripheral vascular resistance and a increases afterload for the heart and make it worse, SNS: more epinephrine will be secreted and make beta1 receptors influence heart to contract more/quick , beta receptors will also stimulate kidneys and make more renin secretion which activates angiotensin and the two effects of angio10 – vasoconstriction peripherally WHICH RAISES PVR and stimulate aldosterone secretion which will increase sodium and water reabsorption and your blood volume will be increased and that will increase preload and afterload. Kidneys wont be getting enough O2 bc of HF and will increase erythropoietin (RBC production) carried in blood to bone marrow and the thickness of blood will be increased If pressure is low More ADH will be secreted and increase erythropoietin will influence RBC production and increase the blood thickness which will increase afterload of the heart and the workload and exacerbate HF. All of management is usually pharmaceutical to block those things – diuretics to decrease blood pressure, beta 1 blockers for reduced angiotensin response, drugs to block effects of aldosterone block alpha 1 receptors, ACE inhibitors to prevent angiotensin 1 into active form Also exercise more, with small amounts but regularly so that u can maintain efficiency of your skeletal muscles so that you can do more physical things with less requirement for increased blood flow so activities like walking won’t be too hard on heart and fail. like walking in a mall or places where there is no steepness or elevation. (heart pic in ipad) Dysrhythmia at sinoatrial node : sinus dysrhythmia : where rates outside of 60-100bpm, for ex you can have sinus tachycardia where SA node has more impulses and its over 100bpm, how ? ST stress response or high levels of T3T4 can be physical/emotional stresses. Sinus bradycardia can happen as result of PNS stimulation for example, the vasovagal reflex where there is a spontaneous burst of impulses out the vagus nerve and it will lead to vasodilatation and bradycardia. Can also block SNS output and lead to vasodilation. Often happens as response to pain/ or from giving blood Atrial dysrhythmia : heart blocks : blocks in conduction. Accelerator nerve: it’s the SNS essentially