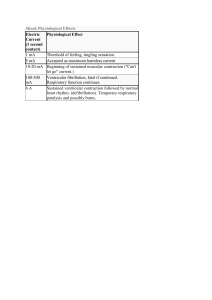
European Heart Journal (1992) 13,966-970 Chagas cardiomyopathy and captopril R. R. ROBERTl*t, E. E. MARTINEZf, J. L. ANDRADEf, V. L. ARAUJOf, F. S. BRITOf, O. P. PORTUGALf AND S. F. H O R O W I T Z * KEY WORDS: Chagas, cardiomyopathy, captopril, arrhythmias. Downloaded from https://academic.oup.com/eurheartj/article-abstract/13/7/966/471537 by University of New South Wales user on 11 November 2019 ^Division of Cardiology, Escola Paulista de Medicina, Rua Botucatu 611 Sao Paulo, SP, 04023 Brazil and the *Division of Cardiology, Beth Israel Medical Center, First Ave. at 16th St. New York, 10003 New York, U.S.A. Chagas disease is a leading cause ofheartfailure in Latin America. Sudden death occurs in approximately 40% of patients with heartfailure due to Chagas disease. We report a single blind, cross-over trial of prolonged treatment with captopril and placebo in 18 Chagas disease patients with class IV NYHA heart failure. Ventricular dimensions, neurohormones, electrolytes and ventricular arrhythmias were analysed in 11 men and seven women receiving stable doses of digoxin and frusemide who were randomly divided into two intervention groups. Group I patients were given increasing doses of captopril up to 150 mg. day~' maintainedfor 6 weeks, group II received the placebo. A 24 h Holter, 2-D echocardiogram, urinary catecholamines, plasma renin and electrolyte determinations were performed at the end of each phase. After a 2-week washout period, the two groups crossed over and another period of 6 weeks was observed. Ventricular arrhythmias were analysed by either Mann-Whitney or the Wilcoxon test. Remaining data were assessed by the Student t-test. A significant reduction in heart rate and urinary catecholamine levels, and enhanced plasma levels of renin, together with a reduction in ventricular couplets wasfound in the captopril-treated group. We conclude that captopril has a beneficial effect on neurohormones with a subsequently reduced heart rate and diminished incidence of ventricular arrhythmias in patients with Chagas disease. This effect might result in a reduction of mortality caused by the disease, suggesting the need for further investigations. Introduction Chagas' disease is a prominent cause of cardiac death in Latin America1'1. Severe congestive heart failure with massive cardiac enlargement is a common finding in infected patients. Once heart failure develops, life expectancy is reduced to a few years'21. Similar to other dilated cardiomyopathies, sudden death occurs in approximately 40% of patients with heart failure;due to Chagas disease121. " In some infected persons sudden death is the first manifestation of illness'31. Studies in cardiomyopathy patients other than those of Chagas disease, who suffered sudden cardiac death while wearing an ambulatory ECG monitor have demonstrated that the mechanism of death is an acute ventricular tachyarrhythmia in approximately 80% of cases'4-51. The incidence of sudden death is increased in patients with marked left ventricular dysfunction and ventricular arrhythmias'4'6-71. Because there has been no definitive study of the impact of antiarrhythmic drug treatment on survival of patients with heart failure and ventricular arrhythmias, the role of therapy with antiarrhythmic drugs remains uncertain at present17"91. Previous reports'3101 have emphasized the importance of structural factors (such as myocardial fibrosis) in predisposing to re-entry phenomena, critical to the development of ventricular ectopic rhythms. Areas of myocardial fibrosis and the presence of left ventricular apical aneurysms are common findings in hearts of patients who die of Chagas disease'"1. Submitted for publication on 3 April 1991, and in revised form September 1991. Correspondence- Dr Steven F. Horowitz, Beth Israel Medical Center, First Ave at 16th St. 8th Dazian, New York, NY (212)42045-60, U.S.A. 0I95-668X/92/070966+05 $03.00/0 However, recent evidence points to potentially reversible arrhythmogenic factors in patients with congestive heart failure: factors such as electrolyte abnormalities, activation of neurohormonal mechanisms and drug therapy for heart failure. Due to its ability to promote cation repletion and to reduce circulating levels of potentially arrhythmogenic neurohormones, captopril may prevent the occurrence of complex ventricular tachyarrhythmias'121 and death from chronic heart failure. A single blind, cross-over trial of prolonged treatment with captopril and placebo in patients with severe congestive heart failure due to Chagas disease is reported here. The effects of the drug on ventricular function, neurohormones, electrolytes and ventricular arrhythmias were analysed. Methods PATIENT POPULATION Eleven men and seven women ranging in age from 23-60 years (mean 43 years), who had suffered from congestive heart failure due to Chagas disease for more than 6 months, were selected for the study protocol. All patients were in NYHA class III or IV and all had shown a positive radioimmunoassay result for Chagas disease. Other cardiomyopathy aetiologies were excluded by clinical history and echocardiography. STUDY PROTOCOL Written informed consent was obtained from every patient. Patients were randomly divided into two groups. Group I consisted of five men and four women, group II © 1992 The European Society of Cardiology Chagas cardiomyopathy and captopril 967 consisted of six men and three women. Initially, stable doses of digoxin (0-25 mg. day"1) and frusemide (mean dose 104 mg. day"1) were given for a period of at least 2 weeks without potassium supplementation. At the end of this period patients were admitted to the hospital and the following measurements were made: Patients I II III IV VI VII VIII IX X XI XII XIII XIV XV XVI (years) 33 35 32 29 37 42 52 60 39 56 60 34 35 59 39 Sex NYHA M IV III III III III M F F M F M M F M M III III III III IV IV IV III III M IV M F F (cm) (kg) 166 176 163 158 165 155 156 172 147 146 165 148 174 162 158 680 66-5 58-5 650 68-5 500 540 530 480 630 57-5 48-5 620 57-5 56-5 Results Patients' age, sex, NYHA functional class for heart failure, height and body weight at the start of the study are presented in Table 1. CLINICAL OUTCOME Of the 18 patients selected, 15 completed the study. Three patients were excluded, all in thefirst2 weeks before Patients from group I received incremental doses of treatment with either the placebo or captopril. Three captopril, starting with 12-5mgt.i.d., increasing to patients had to be admitted to hospital to receive intra50 mg t.i.d. over a 1 week period. This was maintained at venous frusemide, one during captopril treatment and the 50mgt.i.d. for 6 weeks. During a 7-week follow-up other while receiving the placebo. One patient developed period, patients were seen once a week. At the end of this symptomatic hypotension that disappeared when the dose period they were admitted to the hospital and all of the of captopril was reduced to 37-5mg.day" 1 . Another above-mentioned measurements were repeated. Both patient had postural dizziness without demonstrable captopril and the placebo were discontinued for a wash- hypotension that ameliorated after reducing the dose of out period of 2 weeks and all tests were performed again. captopril to 75 mg . day"1. Then, the two groups were crossed over for another period of 7 weeks, after which all measurements were performed for the last time. Due to the severity of the chronic HEART RATE AND BLOOD PRESSURE During treatment with captopril, heart rate was sigheart failure (CHF) in this group of patients we chose a nificantly lower than during treatment with the placebo regimen of matching placebo in a single-blind fashion so (69 ±12 vs 79 ±19 beats, min"1 respectively, P<005). those whose clinical condition worsened could be identThere was no significant difference in systolic and diastolic ified. Ideally, a longer time interval would have allowed us arterial blood pressure during treatment with captopril or to note the beneficial haemodynamic effects of captopril; placebo (Table 2). however, we used the shortest time interval during which captopril effects could be observed and tolerated by patients in the placebo group who were receiving no ECHOCARDIOGRAPHY There were no significant differences in left ventricular vasodilator therapy. end diastolic or systolic dimensions or left ventricular fractional shortening, when comparing the effects of captopril vs those of the placebo (Table 2). STATISTICAL ANALYSIS We compared the two groups using the Student t-test for independent values'161; renin values were first con- RENAL AND HORMONAL EFFECTS verted to logarithms'171. For the comparative analysis of During treatment with captopril urinary excretion of the incidence of ventricular tachyarrhythmias, the Mann- norepinephrine was significantly lower than during treatWhitney test"61 was used; when no difference was seen ment with the placebo (40-7±2-9 vs 56-8±7-8 ug.ml" 1 . we performed a paired t-test or the Wilcoxon'181 paired 24h "' respectively, P < 005) (Table 3).On the other hand, test, comparing the placebo with the captopril phases. the plasma renin level with captopril was significantly Differences were considered significant at P<005. higher than that seen during treatment with the placebo Downloaded from https://academic.oup.com/eurheartj/article-abstract/13/7/966/471537 by University of New South Wales user on 11 November 2019 (i) Arterial blood pressure, heart rate, body weight and height. (ii) 2-D echocardiogram recording with measurement of systolic and diastolic left ventricular dimensions. (iii) Twenty-four-hour ambulatory ECG recording using the Medilog system to determine the total frequency of ventricular premature complexes (VPC), the incidence of ventricular couplets (VC) and the incidence of episodes of nonsustained ventricular tachycardia (NSVT). (iv) Venous blood samples were taken in the morning after patients had been supine for 2 h and after they had fasted overnight to determine serum levels of sodium, potassium, magnesium'131 and plasma renin activity measured by radioimmunoassay'141. (v) Total urinary excretion of catecholamines in 24 h determined by liquid chromatography1151. (vi) The body-urea nitrogen (BUN), plasma creatinine and white blood cell (WBC) count were also determined. Table 1 968 R. R. Roberti etal Table 2 Basal Captoprir Basal Placebo 101 ± 15 72±12 76±11 65 ±10 56±11 16±8 99±10 70±8 69±12' 65±11 54± 12 20±U 98±13 74±12 77 ±20 66±11 56±12 15±7 98±18 68±7 79 ±19* 66±12 56±U 16±7 SBP ^systolic blood pressure (mmHg), DBP = diastolic blood pressure (mmHg), HR = heart rate (beats, min" 1 ), LVEDD = left ventricular end diastolic dimension (mm), LVESD = left ventricular end systolic dimension (mm), LVFS = left ventricular fraction shortening values (%). 'Indicates significant differences between captopril and placebo phases, f < 0 0 5 , values are expressed in mean±SD. Basal BUN Crcatinine RBC WBC Hb Captopril 40±13 37±13 0-9±0-3 0-9±0-3 4-4±0-5 4-3 ±0-3 60±l-5 6-2±23 12-8±ll 12-5± 10 Basal Placebo 36±1O 35±10 0-9±0-2 0-9±0-3 4-3±0-5 4-2±0-5 6-5 ± 2 0 6-6 ± 2 0 12-3±l-4 12-2±I-8 Values are expressed as mean±SD. No significant differences were observed. BUN = body urea nitrogen (mg%). Creatinine is expressed in mg.dl" 1 . RBC = red blood cells (million . c m - \ WBC => white blood cells (thousand . cm" 3 ), Hb = Haemoglobin Table 5 Basal Captopril Basal Placebo 328 406 87 320 222* 41 286 392 68 451 422 317 Table 3 VPC Basal Captopril Basal Placebo vc NSVT Renin 8-6 ±7-6 Norepinephrine 42± 18 Sodium 138±2 Potassium 40±0-3 Magnesium 1 9±01 28-5 ±32* 13 5± 15 40±ll* 46±18 138±2 138±2 4-2 ±0-6 4-2±0-4 l-9±01 l-9±0-l 13-3±21* 56 ±30* 137±3 4-3±0-3 1 -9 ± 0-1 Values are expressed as mean ± SD. 'Indicates significant differences between captopril and placebo phases, P<005. Values for renin werefirstconverted to logarithms, here expressed in Hg.ml~'.h~'. Norepinephrine is expressed in ug.ml-'. 24 h~'. Sodium and potassium are expressed in mEq. 1"' while magnesium is expressed in mg%. Values are expressed as means. 'Significant difference between captopril and placebo phases, P<005. VPC = ventricular premature complexes per 24 h, VC = ventricular couplets per 24 h, NSVT = episodes of non-sustained ventricular tachycardia per 24 h. when they were using the placebo (422 vs 222 VC. 24 h" 1 , /><005)(Table5). Discussion In the present study, captopril induced significant reductions in urinary norepinephrine excretion, heart rate (26-8±8-6 vs 13-4±5-6 ug.ml" . h" respectively, and in the number of ventricular couplets in 24 h, together f<0-05) (Table 3). Although plasma levels of potassium with a significant elevation of plasma renin levels. were higher during the treatment with captopril the differSeveral previous studies have shown captopril to ence did not reach statistical significance (4-0 ±0-4 vs replenish low levels of potassium and magnesium in 1 4-3 ±0-6 mEq . I" ) (Table 3). Mean values for sodium patients with CHF(12'">201. However, similar to other puband magnesium are also listed in Table 3, but differences lications'21"23' plasma levels of potassium and magnesium did not reach levels of statistical significance also. BUN, were not significantly elevated by captopril in the patients creatinine, WBC, red blood cell count (RBC) and haemo- of this study. This may have been related to total body globin levels did not show statistical differences when potassium depletion due to baseline frusemide therapy treatment with captopril or with the placebo were without potassium supplementation. Clearly, captopril compared (Table 4). therapy would suppress any potassium loss; however, the short study interval time might explain the inability to detect potassium repletion. THE 24 H ECG MONITORING Recent studies have shown that elevated levels of plasma In the baseline assessment, before treatment with either captopril or placebo, ventricular premature complexes norepinephrine may indicate a poor prognosis'24'. The most (VPC) and/or ventricular couplets occurred in 80% of striking finding of our study was that captopril induced a subjects, whereas non-sustained ventricular tachycardia reduction in plasma norepinephrine, suggesting a poten(NSVT) occurred in 73% of patients (Table 5). No signifi- tially beneficial effect on the natural history of severe forms cant difference was seen in the incidence of VPC or in the of Chagas disease. Under these circumstances angiotensin number of episodes of NSVT (Table 5) when the treat- II increases central sympathetic discharge'25', increases ments with captopril or placebo were compared. On the norepinephrine release from sympathetic nerve terminals'261 other hand, the number of ventricular couplets was sig- and inhibits re-uptake of norepinephrine'27'. As there was nificantly lower in patients using captopril compared to no significant change in arterial blood pressure, we believe 1 1 Downloaded from https://academic.oup.com/eurheartj/article-abstract/13/7/966/471537 by University of New South Wales user on 11 November 2019 SBP DBP HR LVEDD LVESD LVFS Table 4 Chagas cardiomyopathy and captopril 969 Downloaded from https://academic.oup.com/eurheartj/article-abstract/13/7/966/471537 by University of New South Wales user on 11 November 2019 the decrease in heart rate, also seen in other studies'20*281, of captopril on the occurrence of sudden death and/or may be due to a lessening of risk of heart failure or other overall mortality in severe CHF due to Chagas' disease. angiotensin Il-sympathetic interactions. Elevated plasma renin levels have also been shown to be associated with a poor prognosis in CHF129'. The observed References increase in plasma renin levels during treatment with [1] Marsden PD. Selective primary health care; strategies for control of Chagas disease. Rev Infect Dis 1984; 6: 855-65. captopril indicates inhibition of the converting enzyme [2] Espinosa R, Carrasco HA, Belandria F et al. Expectancy analyactivity with the beneficial result of reduced angiotensin II sis in patients with Chagas1 disease: prognosis after one decade production. (1973-1983). Int J Cardiol 1985; 8:45-6. [3] Prata A. Natural History of Chagas cardiomyopathy. Pan Am Although there were no significant differences in the Health Organ Sci Pub 1976; 318: 191. total numbers of VPC or in the numbers of episodes of [4] Panidis I, Morganroth J. Holter monitoring during cardiac NSVT, thefindingof a significant reduction in the number death: clues to its etiology and prevention. JACC 1983; 2: of ventricular couplets may indicate a tendency towards a 798-805. reduction in ventricular excitability. A longer time course [5] Packer M. Sudden unexpected death in patients with congestive of captopril therapy could further improve haemoheart failure: a second frontier. Circulation 1985; 72: 681-5. [6] Horowitz LN, Morganroth J. Can we prevent sudden death? dynamics, resulting in a further reduction in ventricular Am J Cardiol 1982; 50: 535-8. arrhythmias and/or sudden death. [7] Bigger JT Jr. Why patients with congestive heart failure die: 301 13 1 The CONSENSUS' and the Veterans Administration ' arrhythmias and sudden cardiac death. Circulation 1987; 75 trials emphasize that impairment in cardiac contractility can (IV): 28-35. [8] Wilson JR. Use of antiarrhythmic drugs in patients with heart no longer be viewed as the sole determinant of the rate of failure: clinical efficacy, haemodynamic results, and relation to evolution and progression of CHF. Accordingly, it may survival. Circulation 1987; 75: 64-73. be speculated here that the observed reductions in heart [9] Chakko CS, Gheorghiade M. Ventricular arrhythmias in severe rate, norepinephrine urinary excretion and arrythmias heart failure, incidence, significance and effectiviness of antimay be important in the long-term prognosis of Chagas arrhythmic therapy. Am Heart J 1985; 109:497-504. disease patients, even in the absence of a demonstrable [10] Cranefield PF, Klein HO, Hoffman BF. Condution of the cardiac impulse . 1. delay block and one way block in depressed improvement in left ventricular function. Purkinjefibers.Circ Res 1971,28: 199-219. Peripheral vasoconstriction (due to activation of the [11] Lopes ER, Chapadeiro E, Almeida HO, Rocha A. Contrisympathetic nervous and renin-angiotensin systems), buicao ao estudo da anatomia patologica dos coracoes de chagasicos falecidos subitamente. Rev Soc Bras Med Trop which is evoked in response to an insult to the myocardium 1975; 9: 269. has a central role in this disorder. Such neurohormonal [ 12] Cleland JGF, Dargie HJ, Hodsman GP et al. Captopril in heart activity is an important mechanism that directly contrifailure: A double blind controlled trial. Br Heart J 1984; 52: butes to the function impairment and poor long-term 530-5. outcome of these patients'30'. The reduction of these [13] Hunt BJ. The estimation of magnesium in plasma muscle and bone by atomic absorption spectropnotometry. Clin Chem neurohormones in our study population leads us to 1969; 15:979-96. believe that captopril might improve the prognosis of [14] Millar LA, Leckie BJ, Semple PF, Morton JI, Sokondi S, patients with severe CHF due to Chagas disease even Robertson JIS. Active and inactive renin in human plasma: without a demonstrable marked antiarrhythmic effect. renal arterial venous differences and relationship with angiotensin andreninsubstrate. Circ Res 1978; 43 (Suppl I): 1120-7. The SOLVE)1321 investigators have recently reported that the reduction in mortality in CHF patients receiving [15] Mover TP, Jiang NS, Tyce GM, Sneps SG. Analyses for urinary catecholamines on liquid chromatography, and the anteroenalapril is primarily due to a reduction of deaths classified metric detection. Methodology and clinical interpretation of as being due to progressive CHF; there was little difference results. Clin Chem 1979; 25: 256-63. [16] Skoal RR, Rohlf FJ. Biometry: the principles and practice of in mortality from arrhythmia alone. statistics in biological research. San Francisco: Freeman 1969. Arrhythmias are common and characteristic findings Wenting GJ, Manin'tveld AJ, Woittiez AJ el at. Effects of capin the chronic phase of Chagas disease133-341. Autonomic [17] topril in acute and chronic heart failure. Correlations with 1351 dysfunction is a typical feature of the disease , possibly plasma levels of noradrenaline,reninand aldosterone. Br Heart the result of injury to and reduction in the numbers of J 1983; 49: 65-76. ganglionic cells and cardiac nerve fibres within the myo- [18] Siegel S. Estatistica nao parametrica para ciencias do comportamento. McGraw-Hill 1981. cardium'36371, since T. Cruzi has a predilection for the [19] Cleland JG, Dargie HJ, Robertson JI, Anderson E, East BW. nervous tissue. Heart failure, renin potassium and arrhythmias. Circulation The persistence of ventricular arrhythmias in spite of a 1985; (Suppl III): 111-283 (Abstr). significant reduction in catecholamines may be due to [20] Cleland JGF, Dargie HJ, Ball SG el al. Effects of enalapril in heart failure: a double blind study of effects on exercise performcardiac parasympathetic impairment, typical of Chagas ancerenalfunction, hormones and metabolic status. Br Heart J disease1381. This could result in a predominance of 1985; 54: 305-12. myocardial adrenergic tone as a consequence of the [21] Webster MWI, FitzPatrick MA, Nicholls MG, Ikron H, Wells effect of unopposed norephinephrine release locally JE. Effects of enalapril on ventricular arrythmia in patients with CHF. Am J Cardiol 1985; 56: 566-9. into cardiac muscle by sympathetic nerve terminals'391, even in the presence of near-normal levels of circulating [22] Packer M, Lee WH, Yasnak M, Medina N. Comparison of captopril and enalapril in patients with severe CHF. New Engl J catecholamines. Med 1986; 315: 847-53. The results with a small number of patients suggest [23] Camara EJN, Cruz TRP, Naucri JM, Rodrigues LEA. Muscle magnesium content and cardiac arrythmias during treatment of further clinical studies are warranted to assess the effect 970 R.R.Roberti etal [24] [26] [27] [28] [29] [30] [31] Conn JN, Archibald DG, Ziesche S el al. Effects of vasodilator therapy on mortality in CHF: results of a Veterans Administration cooperative study. New Engl J Med 1986; 314: 1547-52. [32] The SOLVD investigators: Effects of enalapril on survival in patients with reduced left ventricular ejection fraction and congestive heart failure. N Engl J Med 1991,325: 293-302. [33] Chagas C, Villela E. Forma cardiaca de Trypanosomiased Americana. Mens Inst Oswaldo Cruz 1922, 14: 5. [34] Hirschhaut E, Aparicio JM. Stress testing and working capacity in Chagas cardiomyopathy. Cardiology 1978; 63: 343-51. [35] Gallo L. Jr, Marin Neto JA, Manjo JC, Rassi A, Amorin DS. Abnormal heart rate response during exercise in patients with Chagas disease. Cardiology 1975; 60: 147-62. [36] Koberle F. Die Chronishe Chagaskardiopatie. Virc Arch Pathol Anat Physiol 1957; 330 267-95. [37] Mott KE, Hagstron JW. The pathologic lesions of the cardiac autonomic nervous system in chronic Chagas myocarditis. Circulation 1965; 31: 273-86. [38] Oliveira JSM. A natural human model of intrinsic heart nervous system denervation: Chagas cardiomyopathy. Am Heart J 1985; 110: 1092-8. [39] Samuels MA. Neurogenic heart disease: a unifying hypothesis. Am J Cardiol 1987; 60: 15J-9J. Downloaded from https://academic.oup.com/eurheartj/article-abstract/13/7/966/471537 by University of New South Wales user on 11 November 2019 [25] CHF due to chronic Chagas cardiomyopathy. Braz J Med Res 1986;19:49-56. Kao W, Gheorghiade M, Hall V, Goldstein S. Relation between plasma norepinephrine and response to medical therapy in men with congestive heart failure secondary to coronary artery disease or idiopathic dilated cardiomyopathy. Am J Cardiol 1989; 64:609-13. Bickerton RK, Buckley JP. Evidence for a central mechanism in angiontensin-induced hypertension. Proc Exp Biol Med 1961; 106:834-6. Zimmerman BG. Actions of angiotensin on adrenergic nerve endings. Fed Proc 1978; 37: 199-202. Kharallah PA. Action of angiotensin in adrenergic nerve endings: Inhibition of norepinephrine reuptake. Fed Proc 1972,31: 1351-7. Dzau VJ, Colucci WS, Williams GH el al. Sustained effectiveness of converting-enzyme inhibition in patients with severe congestive heart failure. N Engl J Med 1980; 302: 1373-9. Creager MA, Faxon DP, Halperin JL el al. Determinants of clinic responses and survival in patients with CHF treated with Captopril. Am Heart J 1982; 104: 1147-54. The CONSENSUS trial study group: effects of the cooperative North Scandinavian Enalapril survival study. New Engl J Med 1987; 316: 1429-35.