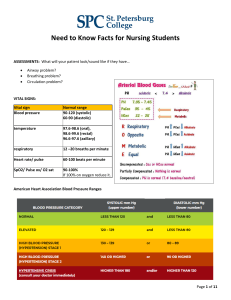
Need to Know Facts for Nursing Students ASSESSMENTS: What will your patient look/sound like if they have… • • • Airway problem? Breathing problem? Circulation problem? VITAL SIGNS: Vital sign Blood pressure Normal range 90-120 (systolic) 60-90 (diastolic) temperature 97.6-98.6 (oral), 98.6-99.6 (rectal) 96.6-97.6 (axillary) respiratory 12 –20 breaths per minute Heart rate/ pulse 60-100 beats per minute SpO2/ Pulse ox/ O2 sat 90-100% If 100% on oxygen reduce it. American Heart Association Blood Pressure Ranges Page 1 of 11 DIGNOSTIC STUDIES: Lab Normal Range Complete Blood Count (CBC) WBC 5 – 10 × 109/L Plts 150 – 400 × 109/L RBC Female: 4.2 to 5.4 million cells/mcL Male: 4.7 to 6.1 million cells/mcL Hgb Female: 12 – 16 g/dL Male: 14 – 18 g/dL Female: 37 – 47 % Male: 42 – 52 % Hct Differential Neutrophils (segs + bands) 55 – 75 % Segs 55 – 70 % Bands 0–8% ANC > 1,500 (absolute neutrophil count) Eosinophils 1–4 % Metabolic Panel (BMP/CMP) Na+ 136 – 145 mEq/L K+ 3.5 – 5 mEq/L Ca+ 9 – 10.5 mg/dL Mg+ 1.3 – 2.1 mEq/L Glucose AST/SGOT Fasting1: 70 – 100 mg/dL Diabetic < 130 mg/dL 90 min after eating: 100 – 140 mg/dL Diabetic < 180 0 – 35 U/L ALT/SGPT 4 – 36 U/L Abnormal Findings ↑ = inflammation or infection ↓ = decreased ability to fight infection ↓ = less material to create clot > bleed easier ↑ = could indicate cancer # of RBCs in serum ↓ = anemia (body is not making/destroying RBCs) or bleeding Part of RBC that carries O2 to all cells in body ↓ = ↓ oxygenation to cells (fatigue, dyspnea) % of blood volume that contains RBCs ↓ = ↓ % volume of RBCs in blood Bodies primary defense against bacterial infection or physiologic stress ↑ = acute bacterial infection ↓ = virus/depleted immune system Mature neutrophils ↑ = acute bacterial infection Immature neutrophils ↑ = acute bacterial infection ↓ = immune system unable to fight infection ANC = (% neutrophils + % bands) x WBC 100 ↑ = Allergic reaction, parasites Fluid balance2 ↓ = swelling of cells > CNS problems3 Fluid balance, muscle, and nerve function2 ↓ = Heart arrhythmia, muscle cramps, fatigue3 ↑ = Heart arrhythmia/palpitations, muscle weakness, diarrhea3 Bone strength, muscle and nerve function2 ↓ = tetany (+Trousseau, + Chvostek), numbness3 ↑ = emotional lability, confusion3 Muscle and nerve function, blood sugar and BP regulation2 ↓ = tetany, personality change3 ↑ = respiratory depression, hypotension, cardiac arrest (torsades)3 *If ↓Mg AND ↓K+ GIVE Mg FIRST* ↑ = diabetes1, stress, steroids ↑ = inflammation/damage to liver > ↓ liver function (may see jaundice, lethargy) ↑ = inflammation/damage to liver > ↓ liver function (may see jaundice, lethargy) Page 2 of 11 Lab Normal Range Metabolic Panel (BMP/CMP) Continued… Alk Phos 30 – 120 U/L BUN 10 – 20 mg/dL Creatinine Female: 0.5 – 1.1 mg/dL Male: 0.6 – 1.2 mg/dL 3.5 – 5 g/dL Albumin GFR Special Hgb A1C1 100 dL/min CK Female: 30-135 U/L Male: 55-170 U/L Coagulation (times) PTT (aPTT) (heparin) PT (warfarin) INR (warfarin) < 5.6% 30 – 40 sec 11 – 12.5 sec 1 D-Dimer < 250 mcg/mL Cardiac Enzymes CK-MB < 4% - 6% of total CK Troponin -Troponin I (more specific for MI) -Troponin T (less specific for MI) < 0.03 mcg/L Abnormal Findings Found in liver and bone ↑ = liver damage/disease (blocked bile duct) OR bone breakdown ↑ = either kidneys are not functioning properly, OR increase in protein catabolism (fever, sepsis, stress) ↑ = ↓ kidney function ↓ = decreased nutritional status or ↓ liver function ↓ = edema r/t low oncotic pressure ↓ = decreased renal filtration (damage to kidneys) Avg blood sugar for the past 2-3 months ↑ = Diabetes1 ↑ = breakdown of muscle > muscle damage ↑ = longer it takes to form clot > bleed easier ↑ = longer it takes to form clot > bleed easier ↑ = longer it takes to form clot > bleed easier ratio = patient PT time normal PT time Released when blood clot is dissolved/dissolving ↑ = lots of small clots or a big clot is being dissolved ↑ = breakdown of cardiac muscle > cardiac muscle damage ↑ = breakdown of cardiac muscle > cardiac muscle damage specific to infarction < 0.1 mcg/L BNP (brain < 100 pg/mL natriuretic peptide) Inflammatory Indicators ESR < 20 mm/hr CRP < 1.0 mg/dL Procalcitonin Urinalysis Sp. Gravity < 0.15 ng/mL Protein Glucose Leukocytes Nitrites Negative Negative 1.01 – 1.02 Negative ↑ = ↑ stretch of heart muscle > heart not effectively pumping blood out into body (heart failure) ↑ = inflammatory response Made by the liver in response to acute inflammation ↑ = acute inflammation ↑ = bacterial infections or tissue injury ↑ = concentrated urine > dehydration ↓ = diluted urine Present = kidneys are inflamed/damaged Present = ↑ serum glucose levels or kidney damage ↑ = inflammation or infection Present = Bacterial UTI (neg nitrites does not mean they do not have UTI. Only some bacteria create nitrites) Page 3 of 11 IV FLUID Type Description Isotonic • Replaces losses without altering intravascular electrolyte concentrations • Only IV Fluid used as a bolus • Increases intravascular volume Normal Saline (NS) 0.9% NaCl in water Lactated Ringer’s (LR) 0.9% NaCl, K+, Ca++, Lactate (buffer) D5W* 5% Dextrose in water D5 ¼ NS* Use/Misc • • • • Helpful for Na+ replacement Often seen with surgery Physiologically hypotonic Isotonic in the bag* 5% Dextrose, 0.22% NaCL Hypertonic • IVF that contains more than an isotonic solution • Moves fluid from intracellular space to extracellular space (monitor for fluid volume overload) D5NS 5% Dextrose, 0.9% NaCl D5 ½NS 5% Dextrose, 0.45% NaCl D5LR 5% Dextrose, LR (0.9% NaCl, K+, Ca++, Lactate) Hypotonic • IVF that contains less than an isotonic solution • Moves fluid from extracellular space to intracellular space (monitor for cerebral edema) • Must infuse very slowly ½ NS 0.45% NaCl in water *Considered isotonic but not used as bolus RULES OF MATH: 1. Rounding to the nearest… a. Whole number = 1 b. Tenths = 0.1 c. Hundredths = 0.01 2. NO trailing zeros (2.6 not 2.60) 3. ALWAYS put a zero before a decimal (0.3 not .3) 4. Gtts/min is ALWAYS a whole number (you can’t give a fraction of a drop) 5. Insulin units is always a whole number (don’t round up) 6. IVF (mL/hr) rate is ALWAYS a whole number 7. ALWAYS use commas! (1,000,000 not 1000000) or your answer will be considered incorrect. Page 4 of 11 ORGAN/STYSTEM: Organ/System Function Liver • Bile production and stores in gallbladder • Excretion of bilirubin, cholesterol, hormones and drugs • Metabolizes fats, proteins, carbohydrates • Stores glycogen (helps to balance glucose levels) , vitamins, iron • Makes albumin, clotting factors • Detoxifies blood • Makes immune factors and removes bacteria from blood • Converts ammonia (dangerous) into urea (excreted in urine) Gall bladder • Stores and excretes bile (when needed by small intestine) o Bile helps digest fats Pancreas • Makes insulin – promotes glucose entry into cells • Makes glucagon – promotes the breakdown of glycogen to glucose in the liver • Makes amylase – helps digest carbohydrates • Makes lipase – helps digest fats Kidneys • Fluid & Electrolyte balance • Acid/Base balance • Excretion of wastes/toxins • Help regulate BP • Stimulation of RBC production • Produce active form of Vit D Spleen • Removes old/abnormal/damaged RBCs o Recycles the iron for use in making new RBCs o Metabolizes the hgb > bilirubin > excreted by liver • Plays a role in immunity o Stores WBC to fight infection o Filters out bacteria and viruses • Stores platelets Lymphatic • Removes fluid from body tissues into the blood System • Contains lymphocytes to fight infection • Lymph vessels drain into lymph nodes o Lymph nodes trap or destroy anything harmful that the body does not need o Lymph nodes contain lymphocytes which attack and break down bacteria, viruses, damaged cells or cancer cells o The lymph fluid carries the waste products and destroyed bacteria back into the bloodstream > excreted by liver or kidneys Renin• Stimulated in response to ↓ in BP Angiotensin • Stimulates production of Angiotensin II System (RAS) o ↑ ADH secretion > kidneys keep H2O o ↑ Aldosterone secretion > kidneys keep H2O and Na+, excrete K+ o Vasoconstriction PHARMACOLOGIC THERAPY: Adrenergic – means “working on epi or nor epi”, part of the autonomic nervous system Agonist – a substance that acts like another substance = stimulates an action Antagonist – blocks an action Page 5 of 11 Anticholinergics – blocks acetylcholine in the CNS & PNS a. Keeping it from binding to nerve cells = inhibiting parasympathetic nerve impulses in the: a. GI tract (constipation) b. Lungs (↓ mucous production, bronchodilation) c. GU tract (urinary retention) b. To help control salivation, digestion, urination and mucous production. MEDICATIONS: Generic name Prefix/suffix Function Anti-coagulants • Stop prior to surgery/procedures Warfarin • ↑ time it takes to form clot > ↑ bleeding • MOA - Inhibits Vit K (liver needs to form factors) • Antidote – Vit K • Labs – PT, INR • Long half-life = approx. 40 hrs (1eek to reach therapeutic level) Heparin • ↑ time it takes to form clot > ↑ bleeding • MOA - Binds activated factors • Antidote – protamine sulfate • Labs – PTT, aPTT • Short half-life = 60 – 90 min (works quickly) Enoxaparin • ↑ time it takes to form clot > ↑ bleeding • Low molecular weight heparin • Antidote – protamine sulfate • Labs – none Apixaban, Rivaroxaban -xaban • ↑ time it takes to form clot > ↑ bleeding • MOA – Direct factor Xa inhibitor • Antidote – none • Labs – none Aspirin • MOA – prevents plts from sticking together • Give if suspect MI • Can cause GI bleeding, tinnitus Anti-Infectives: Antibiotics • Kill or prevent reproduction of bacteria • ↑ risk of opportunistic infections Anti-viral -vir • ↓ virus ability to get into cell • ↓ virus ability to reproduce • ↓ time patient has virus/↓ symptom severity Anti-Inflammatories: NSAIDs • Inhibit COX-1 & COX-2 (↓ prostaglandins) Ibuprofen, Ketorolac - ↓ Renal perfusion - ↓ Plt aggregation - ↓ inflammation • ↑ risk for GI bleeding Steroids • Stop/suppress inflammatory response Prednisone, prednisolone, • ↑ Glucose, ↑ GI acid secretions, ↑ BP, ↑ bone Methylprednisolone breakdown Page 6 of 11 Anti-Hypertensive Meds: • Do not give if HR < 50 bpm or SBP < 100 mmHg ACE Inhibitors -pril ARBs (Angiotensin receptor blockers) -sartan Beta Blockers Cardio Selective: - Metoprolol - Atenolol - Esmolol Non-selective: - Propranolol - Nadolol -lol MOA – inhibits production of Angiotensin II o Vasodilation o ↓ intravascular fluid volume • Labs – K+ (can cause ↑ K+ levels) • Can cause irritating cough • MOA – inhibits action of Angiotensin II o Vasodilation o ↓ intravascular fluid volume • Labs – K+ (can cause ↑ K+ levels) Given in acute stages of MI • MOA – block Beta1 only o ↓ HR, ↓ contractility, ↓ renin secretion • • • • Alpha & Beta Blockers: - Carvedilol - Labetalol Diuretics: Monitor BP Safety: Fall precautions, Orthostatic Hypotension - Loop (furosemide) - K+ sparing (spironolactone) - Thiazide (hydrochlorothiazide) Heart Failure Meds: Daily weights Cardiac Glycosides (Digoxin) GI Meds PPI (proton-pump inhibitors) H2 Blockers Antacids (Tums, Milk of Magnesia) Prokinetic (metoclopramide) Anti-Nausea/Emetic - Ondansetron - Phenergan - Compazine • • MOA – block all Beta Cells o ↓ HR, ↓ contractility, ↓ renin secretion Bronchoconstriction (contraindicated in asthma, COPD, etc.) Hypo/Hyperglycemia (inhibits glucose release, blocks pancreatic beta cells) Non-selective traits Vasodilation ↓ intravascular fluid volume MOA – ↑ urination Labs – Na+, K+, Creatinine • can cause ↓ K+ levels, ↑ Glucose, Ototoxicity • can cause ↑ K+ levels (inhibit aldosterone) • can cause ↓ K+ levels, ↑ Glucose • CAUTION: Allergy to sulfonamide Abx -prazole -tidine • • • MOA – ↑ contractility of heart, ↓ HR Labs – K+ (do not give if ↓K+ > Dig toxicity) S/S of Toxicity: HR < 60 bpm, fatigue, weak, nausea, visual changes (halos) o Antidote – Digoxin Immune Fab • • • • • • • • MOA – stops ALL acid production in stomach Used with antibiotic to treat H. Pylori Should only use for 1 month MOA – decreases acid production in stomach MOA – neutralize acid already in the stomach MOA – increases gastric emptying Can cause extrapyramidal movements MOA - Stops signal to brain to induce vomiting - Blocks histamine receptors in stomach - Blocks dopamine receptors in brain Page 7 of 11 Diabetic Meds: Monitor glucose levels Insulin • • • Metformin Incretin mimetics (exenatide, dulaglutide, liraglutide, albiglutide) -tide Sulfonylureas (glipizide, glyburide, glimepiride) Glucagon -ide Narcotics: Monitor: RR, BP, LOC; Fall Precautions Opioids: Heroin, Oxycodone, Hydrocodone, Opium, Hydromorphone, Morphine, Fentanyl, Tramadol, Methadone Benzodiazepam: -pam Lorazepam, Midazolam, Diazepam, -lam Alprazolam, Clonazepam • • • • • • • • Type I Diabetes MOA – supplements bodies inability to produce insulin MOA - ↑ glucose uptake and use by muscles - ↑ insulin receptor sensitivity - ↓ glucose absorption of intestines - ↓ glucose production by the liver First line treatment for Type II diabetes STOP 24 hrs before GETTING CONTRAST MOA - ↑ release of insulin - ↓ release of glucagon - Delays gastric emptying SQ injection ↑ release of insulin CAUTION: Sulfonamide allergy ↑ glucose release by liver (ADMIN for HYPOGLYCEMIA) SQ, IM, IV – turn pt before admin (prevent aspiration) • Antidotes – Naloxone (may give multiple doses as it wears off) Long acting forms ↓ risk of abuse • Antidote - Flumazenil • RESPIRATORY MEDICATIONS: Category β-adrenergic agonist Mechanism of Action Relaxes the muscles of the small airways →widening the airway. Anti-cholinergic Relaxes smooth muscle → bronchodilation of large airways (bronchi), and ↓ mucous production. Increases watery secretions→ thinning mucous Breaks up the sputum → dissolving mucous Decrease inflammation Expectorants Mucolytic Corticosteroids Antitussives Mast cell stabilizers Leukotriene receptor agonist Suppress cough Inhibits hypersensitivity reaction → inhibits histamine release from mast cells Inhibits leukotrienes → produced by the immune system Leukotrienes promote: bronchoconstriction, inflammation, capillary permeability, and mucus secretion Examples Short acting: Albuterol, Levalbuterol, racemic epi Long acting: salmeterol Short acting: Atrovent (Ipratropium bromide) Long acting: Spiriva (tiotropium) Guaifenesin Mucomyst (acetylcysteine) Inhaled: Pulmicort (budesonide), Flovent (fluticasone propionate), QVAR (beclomethasone) PO/IV: Solu-medrol (methylprednisolone), Prelone/Orapred (prednisolone), prednisone Delsym (dextromethorphan) NasalCrom (Cromoglicic acid), Xolair ( Omalizumab) Singulair (Montelukast) Page 8 of 11 INSULIN COMPARISON CHART: Insulin Name Lispro (Humalog) Aspart (Novolog) Glulisine (Apidra) Afrezza (inhaled insulin) Regular (Novolin R or Humulin R) Isophane suspension (NPH) (Novolin N or Humulin N) Glargine (Lantus) Detemir (Levemir) Humulin 70/30 (isophane/regular) Novolin 70/30 (isophane/aspart or regular) Novolog Mx 70/30 (aspart protamine/aspart) Humalog Mix 75/25 (lispro protamine/lispro) When does it start working? (onset) 15-30 min When will the effect be the greatest? (peak) Rapid Acting Black box warning: acute bronchospasm in pts w/chronic lung disease Short Acting 30-60 min Intermediate Acting 1-2 hrs 70 min 15-30 min 15-30 min Long Acting Combinations How long will it lower blood glucose? (duration) 1-2 hrs 3-5 hrs 1-5 hrs 6-10 hrs 6-14 hrs 16-24 hrs none Up to 24 hrs 1st: 1-2 hrs 2nd: 6-14 hrs 16-24 hrs 1st: 1-2 hrs 2nd: 4-8 hrs 16-24 hrs Page 9 of 11 MEDICATION ERROR PREVETION: Page 10 of 11 NEEDLE SIZE/SITE Parenteral Route Intradermal Subcutaneous Syringe Selection 1-mL tuberculin syringe ½-3 mL Needle Diameter and Needle Angle Needle length 25-27 gauge, ½ - 5/8 inch 5-15 degrees 25-27 gauge, 3/8-5/8 inch (up to 1 inch for an obese patient) 45 to 90 degrees Subcutaneous Insulin syringe U-100, Pre-attached to insulin Insulin U-50, or U-30 syringe: 25-31 gauge, 5/16 to ½ inch 45 to 90 degrees Intramuscular Adults: 1-5 mL 18-25 gauge, 5/8 to 1 ½ (IM) depending on site and inch muscle mass Oil based solutions: 18-20 gauge 90 degrees Site Selection Inner forearm, upper arm and across the scapula Abdomen, lateral aspects of the upper arm and thigh, scapular are of the back, and upper ventrodorsal gluteal area Abdomen, lateral aspects of the upper arm and thigh, scapular are of the back, and upper ventrodorsal gluteal area Ventrogluteal, vastus lateralis, and deltoid. ATI and Yoost, B. L., & Crawford, L. R. (2020). Fundamentals of Nursing: Active learning for collaborative practice (2nd ed.). Elsevier. Resources: 1. American Diabetes Association. https://www.diabetes.org/a1c/diagnosis 2. National Institutes of Health. Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/list-all/ 3. Merck Manual: Professional Version. https://www.merckmanuals.com/professional Page 11 of 11