Health and Social Care Delivery for People
with Dementia
Dr. Nancy Agnes, Head, Technical Operations, Tutorsindia info@ tutorsindia.com
I. INTRODUCTION
Disabilities can be caused by several factors and one
of the leading causes of disability amongst the elderly
population has been recognized as dementia. It has
also been observed that the prevalence of dementia
tends to double during a span of twenty years wherein
the estimated costs of the gross domestic product is
pegged at 1 per cent. The necessities of people
suffering with dementia are quite cumulative, chronic
and they warrant support from social and healthcare
and also from care-givers from the family. Dementia
is known to make a deep societal impact and the
advantages presented by prioritizing early
identification of patients are quite well-rehearsed.
This would comprise of predicting the future
requirements of patients and their families and also
access to interventions at an early stage. Psychosocial
interventions and utilizing medications within
primary care for people with dementia tends to
provide substantial advantages for enhancing the
level of care that is provided. It has been stated by
Alzheimer’s Society [2] that the number of people in
the UK who have been diagnosed with dementia
totals around 850,000. The authors further state that
this number would witness an exponential increase
over the forthcoming decades. As a matter of fact, [3]
goes on to add that one out of every three individuals
who have been born in 2015 would tend to develop
dementia during the course of their life. Such
statistics tend to draw the attention on the growing
issue of dementia within the UK thus rendering it
significant for diverse social and healthcare
professionals to provide health and social care in an
effective manner to individuals suffering from
dementia. This brief essay will deliberate about social
and healthcare delivery to individuals with dementia
on the basis of a bio-psychosocial viewpoint.
[Suprising with the Statistics of Demantia? Want to
write a thesis paper on healthcare? Mail us to
info@tutorsindia.com]
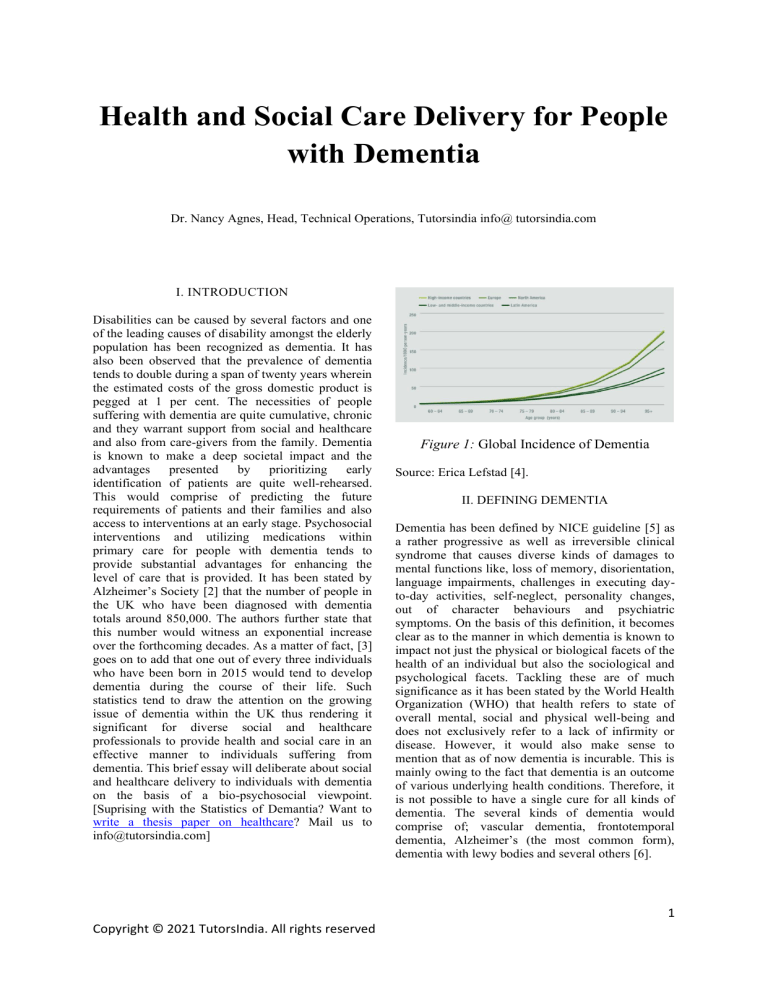
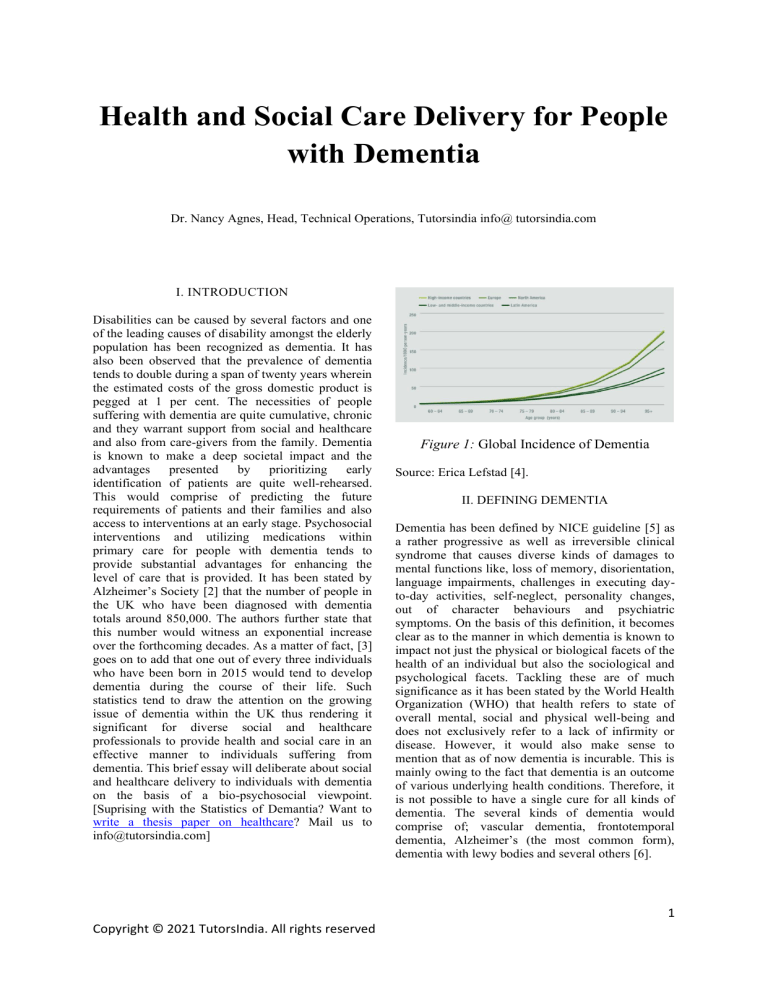
Figure 1: Global Incidence of Dementia
Source: Erica Lefstad [4].
II. DEFINING DEMENTIA
Dementia has been defined by NICE guideline [5] as
a rather progressive as well as irreversible clinical
syndrome that causes diverse kinds of damages to
mental functions like, loss of memory, disorientation,
language impairments, challenges in executing dayto-day activities, self-neglect, personality changes,
out of character behaviours and psychiatric
symptoms. On the basis of this definition, it becomes
clear as to the manner in which dementia is known to
impact not just the physical or biological facets of the
health of an individual but also the sociological and
psychological facets. Tackling these are of much
significance as it has been stated by the World Health
Organization (WHO) that health refers to state of
overall mental, social and physical well-being and
does not exclusively refer to a lack of infirmity or
disease. However, it would also make sense to
mention that as of now dementia is incurable. This is
mainly owing to the fact that dementia is an outcome
of various underlying health conditions. Therefore, it
is not possible to have a single cure for all kinds of
dementia. The several kinds of dementia would
comprise of; vascular dementia, frontotemporal
dementia, Alzheimer’s (the most common form),
dementia with lewy bodies and several others [6].
1
Copyright © 2021 TutorsIndia. All rights reserved
helpful to them in effectively tackling issues
pertaining to the required adjustments they would
have to undergo as an outcome of their ailment.
IV. CONCLUSION
III. CARE DELIVERY
There is scope for deliberating that the focus in terms
of provision of care for people with dementia would
be to assist them to cope and manage their condition
in a highly effective manner, while preventing
complications as well as other challenges associated
with health that would be an outcome of a gradual
progression of symptoms and illness. It has been
stated by Handley, Bunn and Goodman [7] that social
and health care professionals should focus more on
sustaining the independence of patients as much as
possible while tackling the challenges confronted by
patients in terms of their day-to-day functioning, in
order to increase their functionality while reducing
the need for support. It would also be critical to stress
upon the fact that care management in dementia is
rather individualistic as all individuals with dementia
might be confronted with distinct challenges related
to their ailment and this would largely hinge on the
stage and nature of their disease.
From a
psychosocial viewpoint, the argument that people
who have been diagnosed with dementia tend to
suffer negative feelings with regards to their
diagnosis, does hold true. In the likely instance that
the patient happens to be a female who has been
diagnosed with dementia recently, it would be
important on the part of social and healthcare
professionals to provide the patient and her family
with adequate information that would allow them to
better understand the disease and thus be better
prepared to cope with the changes that the patient and
her family members might experience as an outcome
of the diagnosis of dementia of the patient. This
argument is supported with a cross-sectional study
that was carried out by Lee, Roen and Thornton [8]
which found that it was necessary for people with
dementia to be in a position to understand and derive
sense from their diagnosis as this would prove to be
Care management in dementia would comprise of
tackling the psychosocial and biological effects that
emerge due to the condition. The focus in terms of
care delivery should be directed at assisting the
patient to sustain their functionality without any
unnecessary complications and effectively allowing
the patient and the family to cope with the condition.
Social as well as healthcare professionals need to
make sure that interventions of care are largely
personalized which indicate that the stage of
dementia and the required concerns and necessities of
patients should be initially identified using diverse
strategies and tools. Offering information to the
patient as well as his or her family is critical as it
allows them to get better insights about the condition
and thus circumvent any burden or stigma associated
with dementia.
REFERENCES
[1]
F. Bunn et al., “Healthcare organisation and
delivery for people with dementia and
comorbidity: a qualitative study exploring the
views of patients, carers and professionals,”
BMJ Open, vol. 7, no. 1, p. e013067, Jan.
2017, doi: 10.1136/bmjopen-2016-013067.
[2]
Alzheimer’s Society, “Dementia UK Second
edition - Overview,” 2014. [Online].
Available:
http://eprints.lse.ac.uk/59437/1/Dementia_U
K_Second_edition_-_Overview.pdf.
[3]
F. Lewis, “Estimation of future cases of
dementia from those born in 2015,” 2015.
[Online].
Available:
https://www.ohe.org/system/files/private/publ
ications/417 - Estimation of future cases of
dementia.pdf.
[4]
Erica Lefstad, “The Epidemiology and
Impact of Dementia Current State and Future
Trends,”
2015.
[Online].
Available:
https://www.who.int/mental_health/neurolog
y/dementia/dementia_thematicbrief_epidemio
logy.pdf.
[5]
NICE guideline, “Dementia: assessment,
management and support for people living
with dementia and their carers,” 2018.
https://www.nice.org.uk/guidance/ng97.
[6]
NHS,
“Dementia,”
https://www.england.nhs.uk/mental-
2021.
2
Copyright © 2021 TutorsIndia. All rights reserved
health/dementia/.
[7]
M. Handley, F. Bunn, and C. Goodman,
“Dementia-friendly interventions to improve
the care of people living with dementia
admitted to hospitals: a realist review,” BMJ
Open, vol. 7, no. 7, p. e015257, Jul. 2017,
doi: 10.1136/bmjopen-2016-015257.
[8]
S. M. Lee, K. Roen, and A. Thornton, “The
psychological impact of a diagnosis of
Alzheimer’s disease,” Dementia, vol. 13, no.
3, pp. 289–305, May 2014, doi:
10.1177/1471301213497080.
3
Copyright © 2021 TutorsIndia. All rights reserved