Inflammation & Carcinogenesis: H. pylori & Cancer Development
advertisement
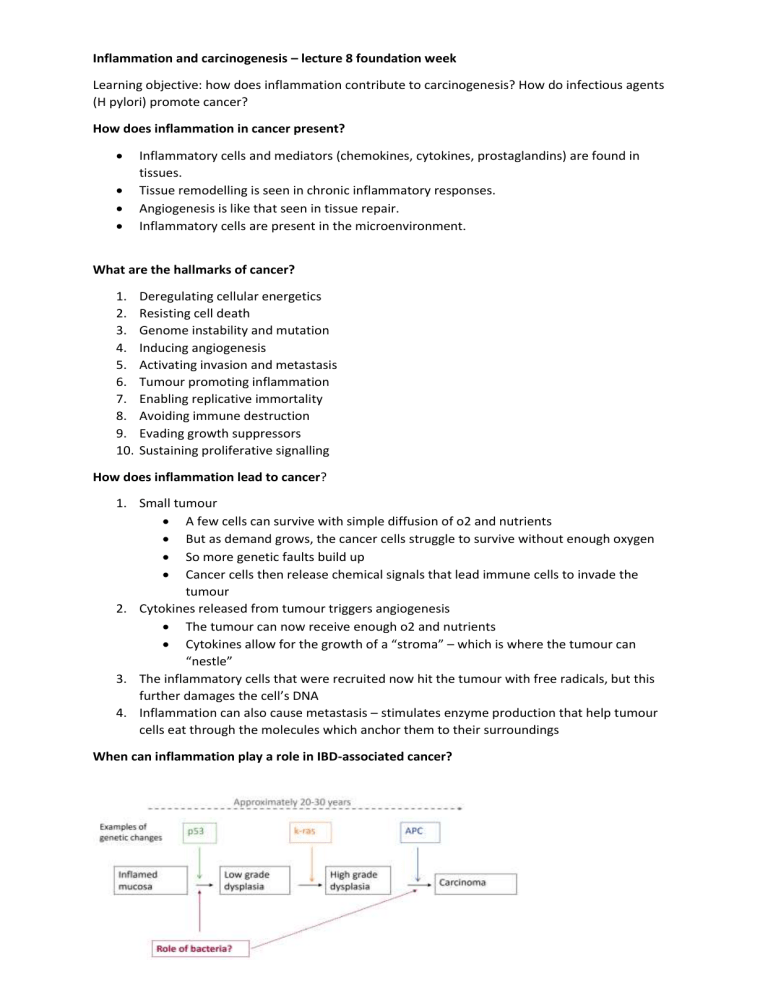
Inflammation and carcinogenesis – lecture 8 foundation week Learning objective: how does inflammation contribute to carcinogenesis? How do infectious agents (H pylori) promote cancer? How does inflammation in cancer present? Inflammatory cells and mediators (chemokines, cytokines, prostaglandins) are found in tissues. Tissue remodelling is seen in chronic inflammatory responses. Angiogenesis is like that seen in tissue repair. Inflammatory cells are present in the microenvironment. What are the hallmarks of cancer? 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Deregulating cellular energetics Resisting cell death Genome instability and mutation Inducing angiogenesis Activating invasion and metastasis Tumour promoting inflammation Enabling replicative immortality Avoiding immune destruction Evading growth suppressors Sustaining proliferative signalling How does inflammation lead to cancer? 1. Small tumour A few cells can survive with simple diffusion of o2 and nutrients But as demand grows, the cancer cells struggle to survive without enough oxygen So more genetic faults build up Cancer cells then release chemical signals that lead immune cells to invade the tumour 2. Cytokines released from tumour triggers angiogenesis The tumour can now receive enough o2 and nutrients Cytokines allow for the growth of a “stroma” – which is where the tumour can “nestle” 3. The inflammatory cells that were recruited now hit the tumour with free radicals, but this further damages the cell’s DNA 4. Inflammation can also cause metastasis – stimulates enzyme production that help tumour cells eat through the molecules which anchor them to their surroundings When can inflammation play a role in IBD-associated cancer? When can inflammation play a role in sporadic colon cancer? In sporadic cancer there are more inflammatory chemicals like: Pro-inflammatory cytokines: il-6 and tnf-alpha Increased intestinal expression of cyclooxygenase 2 (COX2). COX 2 makes prostaglandins from arachidonic acid Which infectious agents are considered carcinogenic? Stomach: helicobacter pylori Liver: hep b, c, Opisthorchis viverrini, Clonorchis sinensis Cervix/uteri: HPV, HIV Anogenital: HPV, HIV Nasopharynx: EBV Oropharynx: HPV Kaposi’s sarcoma: herpes virus type 8 Non-hodgkins lymphoma: H pylori, EBC, HCV Hodgkins lymphoma: EBV Bladder: schistosoma haematobium Which bacteria are involved in cancer? Salmonella typhi: gallbladder cancer Helicobacter pylori: gastric cancer Streptococcus gallolyticus: colon cancer What proportion of people infected with H. pylori develop gastric cancer? <2% What are the “virulence factors” of H pylori? Molecules produced by infectious agents that allow them to succeed How does cancer usually develop in the stomach? Normal gastric epithelium -> superficial gastritis -> atrophic gastritis Atrophic gastritis is a process of chronic inflammation of the gastric mucosa of the stomach, leading to a loss of gastric glandular cells and their eventual replacement by intestinal and fibrous tissues In superficial gastritis: Acute gastritis with superficial erosions. Mucosal erythema and edema consistent with acute gastritis. No correlation exists between microscopic inflammation (histologic gastritis) and the presence of gastric symptoms (eg, abdominal pain, nausea, vomiting Atrophic gastritis -> intestinal metaplasia -> dysplasia -> gastric adenocarcinoma