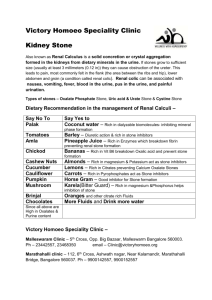
Renal Calculi: Kidney Stones; Urolithiasis; Nephrolithiasis; Staghorn Calculi Renal stones are a common problem, affecting men more frequently than women, and Caucasians more often than African Americans. People in the southeastern and southwestern United States are more likely to develop calculi; this is thought to be a result of warmer weather, higher chance for dehydration, and more concentrated urine. Stones may form anywhere in the urinary tract but most often form in the kidney; they commonly move to other parts of the urinary tract, causing pain, infection, and obstruction. Approximately 90% of stones pass spontaneously. Stones may be treated medically, mechanically (by nephroscopic technique or by lithotripsy [use of shock waves to crush the stones]), or surgically (by pyelolithotomy or nephrolithotomy). Renal stones may be made up of calcium phosphate, calcium oxalate, uric acid, cystine, magnesium ammonium phosphate (also called struvite stones), or combinations of these substances. Calculi NANDA-I develop in situations associated with decreased urine flow, urinary tract injury, and metabolic disorders that alter calcium balance. Changes in urine pH and side effects of some drugs also may contribute to stone formation. Staghorn calculi are large stones that fill and obstruct the renal pelvis. The process of stone formation begins with supersaturation of the urine by one or more salts. As the concentration of salts in the urine increases, the salts precipitate into a solid state. These solid-state salts form crystals that grow into a stone. This growth process is influenced by the pH of the urine, the patient’s hydration status, the presence of other crystals and biological material in the kidney, structural changes in the urinary tract, and crystal growth–inhibiting substances. This care plan addresses management of the patient hospitalized with kidney stones; it also addresses postoperative and postlithotripsy care. Deficient Knowledge Common Related Factors Defining Characteristics Insufficient information Insufficient interest in learning Insufficient knowledge of resources Misinformation presented by others Insufficient knowledge of prevention and treatment of renal stones Inaccurate follow-through of instruction Inaccurate performance on a test Inappropriate behavior Common Expected Outcome Patient verbalizes understanding of factors related to development and recurrence of renal calculi and verbalizes understanding of treatment options. NOC Outcomes Knowledge: Disease Process; Knowledge: Treatment Regimen Ongoing Assessment Actions/Interventions ■ Assess the patient’s knowledge of renal stone prevention. Rationales The recurrence of renal stones may indicate a knowledge deficit regarding prevention. This information provides the starting base for educational sessions. QSEN: Patientcentered care. ■ = Independent = Interprofessional Collaboration Copyright © 2018, Elsevier Inc. All Rights Reserved. Renal and Urinary Tract Care Plans NIC Interventions Health Literacy Enhancement; Learning Facilitation; Teaching: Disease Process; Teaching: Prescribed Diet; Teaching: Prescribed Medication; Teaching: Procedure/Treatment Actions/Interventions ■ Assess for a family history of renal stones. ■ Assess the patient’s self-efficacy to learn and apply new knowledge about the relationship of diet, fluid intake, and activity to the development or recurrence of renal stones. ■ Assess for a history of medical factors that predispose to the formation of renal stones. Rationales An incidence of stones is higher among individuals with a positive family history. A first step in teaching may be to foster increased self-efficacy in the patient’s ability to learn the desired information or skills. Some lifestyle changes can be difficult for the patient to make. Restriction of calcium intake may not prevent the recurrence of calcium salt stones. An increased protein intake may be a more significant factor in calcium stone formation. In some patients, an increased calcium intake may decrease the formation of calcium salt stones. Studies suggest a relationship between the intake of sucrose and sodium with increased stone formation. People who have a sedentary lifestyle or limited mobility are at a higher risk for the development of renal calculi because of calcium loss from bones combined with urinary stasis. QSEN: Evidence-based practice; Safety. Medical conditions that result in the stasis of urine or a calcium imbalance are associated with the development of renal stones. In men, prostatic hyperplasia and the resulting urine stasis may contribute to stone formation. Therapeutic Interventions Actions/Interventions ■ Teach the patient about straining all urine. ■ Teach the patient the following regarding diet: Renal and Urinary Tract Care Plans For patients with stones related to hypercalciuria: • Limit protein intake. For patients with stones related to oxalate: • Foods containing oxalate should be restricted. • Add cranberry juice to the diet. For patients with stones related to uric acid: • An alkaline-ash diet should be followed. For patients with struvite stones: • An acid-ash diet is recommended. ■ Teach the patient the importance of maintaining a fluid intake of 3000 to 4000 mL/day. Rationales This procedure detects the passage of stones, stone fragments, or gravel. If the type of stone (i.e., composition) is unknown, the stone may be sent to a laboratory for analysis. This information assists in planning therapy to prevent the recurrence of stones and for diet modification. Stone fragments may continue to pass for weeks after stone crushing or lithotripsy. The patient may be responsible for straining urine at home and recognizing the passage of a stone. QSEN: Patient-centered care. Dietary modifications are based on the chemical composition of the stone. QSEN: Evidence-based practice. Diets high in protein are associated with calcium stone formation. These sources of oxalate include green leafy vegetables, coffee, tea, chocolate, colas, peanuts, and peanut butter. Cranberry juice has been shown to decrease the formation of oxalate stones. Foods encouraged on an alkaline-ash diet include dairy products; fruits, except cranberries, plums, and prunes; vegetables, beans, and meats. Foods encouraged on an acid-ash diet include meat, eggs, poultry, fish, cereals, and most fruits and vegetables. Increased fluid intake helps dilute the concentration of crystals in the urine, prevents urinary stasis, and flushes urine crystals from the kidney. For additional care plans, go to http://evolve.elsevier.com/Gulanick/. Copyright © 2018, Elsevier Inc. All Rights Reserved. • Sodium cellulose phosphate • Diuretic agents (thiazide) • Cholestyramine • Allopurinol ■ Teach patients to increase activity. ■ Teach the patient the following about the possible courses of treatment: • Medical management • Mechanical intervention • Surgical intervention Rationales Medications can alter the absorption and/or excretion of minerals that contribute to stone formation and prevent recurrence of stones. QSEN: Evidence-based practice; Safety. This drug binds calcium so that the gastrointestinal (GI) absorption of calcium is decreased. The drug may be used for prevention of calcium stones associated with hypercalciuria. These drugs increase tubular reabsorption of calcium, making it less available for calculi formation in the urinary tract. The drugs help with the passage of stones by increasing urine volume. This drug binds oxalate and enhances GI excretion. It is useful for the prevention of oxalate stones. This drug reduces uric acid production for prevention of uric acid stones. It is used for prevention of oxalate stones. The drug helps with passage of stones by decreasing urine pH. Increased physical activity prevents the stasis of urine in the bladder and facilitates passage of stones. Patients may want to focus only on self-care techniques that facilitate discharge from the hospital or enhance home management of renal stones (e.g., how to take medications) and are less interested in specifics of the disease process. The Ask Me 3 program for health literacy stresses the importance of focusing on three questions: What is my main problem? What do I need to do? Why is it important for me to do this? QSEN: Patient-centered care; Evidencebased practice. Ninety percent of stones pass spontaneously; there may be considerable pain, nausea, and vomiting. If it is thought that the stone is moving and will pass, management will consist of fluid therapy, pain management, and antibiotics to prevent or treat infection caused by the stasis of urine or obstruction caused by the stone. Nonsteroidal antiinflammatory drugs (NSAIDs) are the primary drugs used for pain relief. Alpha-adrenergic antagonists, such as tamsulosin (Flomax), relax the smooth muscles of the ureter to reduce pain and facilitate passage of stones. Percutaneous catheters may be used to instill chemicals to dissolve the stone. Ureteroscopic procedures using a basket to catch and crush the stone may be used. Use of shock waves, either passed through percutaneous catheters or transmitted through a fluid medium from outside the body (extracorporeal shock wave lithotripsy), may be used to pulverize stones so that the fragments can pass. Surgical procedures include ureterolithotomy (an incision into a ureter to remove a stone), pyelolithotomy (incision into the renal pelvis to remove a stone), and nephrolithotomy (incision into the calyx of the kidney to remove a stone). Partial or complete nephrectomy may be done if damage or infection from the stone is severe. Many of these procedures are done using minimally invasive techniques. Stents may be placed in the ureter to facilitate stone passage and minimize damage to the ureter by the stone. ■ = Independent = Interprofessional Collaboration Copyright © 2018, Elsevier Inc. All Rights Reserved. Renal and Urinary Tract Care Plans Actions/Interventions ■ Teach the patient about the medications used to prevent the recurrence of renal calculi: Actions/Interventions ■ Teach the patient to report the signs of infection: • Pain not relieved by medication • Fever accompanied by nausea, vomiting, chills • Changes in appearance or odor of the urine NANDA-I Rationales Renal stones may be a factor in developing a urinary tract infection. Some episodes of renal stones may be the result of a urinary tract infection. Early recognition of an infection by the patient allows for prompt treatment. QSEN: Safety. Acute Pain Common Related Factors Defining Characteristics Biological injury agent (irritation by presence of, obstruction by, or movement of the stone) Physical injury agent (obstruction of flow of urine caused by the stone) Self-report of intensity using standardized pain scale Self-report of pain characteristics using standardized pain instrument Expressive behavior (e.g., crying, restlessness, vigilance) Positioning to ease pain Change in physiological parameter (e.g., BP, HR, respiratory rate, and oxygen saturation) Common Expected Outcomes Patient reports satisfactory pain control and a decreased intensity using a standardized pain scale. Patient uses pharmacological and nonpharmacological pain management strategies. Patient exhibits increased comfort such as baseline levels for pulse, BP, respirations, and relaxed muscle tone or body posture. NOC Outcomes Comfort Status; Pain Level; Pain Control; Medication Response NIC Interventions Pain Management; Analgesic Administration Ongoing Assessment Renal and Urinary Tract Care Plans Actions/Interventions ■ Assess the location and duration of pain. A numeric rating scale (0 to 10) or other descriptive scales can be used to assess pain intensity. ■ Assess the patency of drains or catheters in postoperative patients. Rationales The patient is the most reliable source of information about his or her pain. Pain associated with renal stones is typically located in the flank region and may radiate to the pelvic or abdominal area. The pain pattern is sometimes referred to as renal colic. Pain related to obstruction of the ureter by the stone or movement of the stone is commonly severe and may be associated with profuse diaphoresis, nausea, and vomiting. Patients may report extremely severe pain intensity with a rating of 10 on a numeric rating scale. Pain subsides when the stone passes into the bladder. QSEN: Patient-centered care. The obstructed flow of urine results in increased renal pressure and causes or intensifies pain. Therapeutic Interventions Actions/Interventions Administer analgesics as prescribed; evaluate their effectiveness. Rationales NSAIDs are the more commonly used analgesics for management of pain with renal stones. These drugs promote comfort and prevent peak periods of pain. Patients may require opioid analgesics for severe pain. For additional care plans, go to http://evolve.elsevier.com/Gulanick/. Copyright © 2018, Elsevier Inc. All Rights Reserved. Actions/Interventions ■ Use nonpharmacological pain management methods that have been successful for the patient in the past. NANDA-I Rationales Positioning, distraction, and the application of heat may relieve or ease pain and reduce the amount of analgesic required. Patients with renal calculi typically assume a crouched, still position; changing positions may be associated with increased pain. Risk for Infection Common Risk Factors Inadequate primary defenses: stasis of urine Insufficient knowledge to avoid exposure to pathogens Invasive procedures of the urinary tract Common Expected Outcome Patient remains free of infection as evidenced by normal temperature, normal white blood cell (WBC) count, and clear urine. NOC Outcomes Infection Severity; Risk Control; Risk Detection NIC Interventions Infection Protection; Tube Care: Urinary; Incision Site Care Actions/Interventions ■ Assess the patient’s understanding of strategies to prevent urinary tract infection. ■ Monitor the patient’s urine output. ■ Monitor the urine for hematuria, cloudiness, and odor. ■ Observe for changes in the elimination pattern. Monitor the patient’s temperature. Monitor the WBC count. Postprocedure: ■ Observe percutaneous sites and incisions for redness, swelling, and pain. Obtain a culture of urine and drainage from around the catheters (meatal or percutaneous). ■ Check the pH of urine. ■ Rationales The discharge plan of care will be based in part on the patient’s knowledge of strategies to prevent urinary tract infections. QSEN: Patient-centered care; Safety. A desired urine output is 2000 to 3000 mL/24 hr. Urine that is more dilute and has a higher rate of flow will decrease urinary stasis. Increased urine volume increases the possibility that the stone will pass spontaneously and decreases the possibility of further stone formation and infection. Hematuria results from trauma to the urinary tract as the stone moves. Trauma to the urinary tract increases the risk for subsequent infection. Urine cloudiness and foul odor are signs of infection. Dysuria, frequency, and urgency are usually indicative of a urinary tract infection. Urinary tract infection can result in very high fever. An elevated WBC count is a sign of infection. QSEN: Safety. These manifestations may indicate infection. QSEN: Safety. Antibiotic therapy will be based on the specific microorganism causing the infection. QSEN: Evidence-based practice. Urine with a pH of 6.0 or greater (i.e., alkaline urine) is more susceptible to infection than acidic urine. ■ = Independent = Interprofessional Collaboration Copyright © 2018, Elsevier Inc. All Rights Reserved. Renal and Urinary Tract Care Plans Ongoing Assessment Therapeutic Interventions Actions/Interventions ■ Encourage a fluid intake of 3000 to 4000 mL of fluid daily. ■ Teach and encourage perineal care every 8 hours for patients with indwelling catheters. Maintain a closed drainage system. ■ Encourage measures to acidify urine. Administer antibiotics as prescribed. ■ Patients and their caregivers can prevent infection through the use of appropriate hygiene measures at home. QSEN: Patient-centered care. Renal and Urinary Tract Care Plans ■ Instruct the patient to report any worsening in pain, fever, or chills. Following surgical procedures, teach the patient or caregiver to change dressings over percutaneous nephrostomy tubes and incisions as prescribed, using good handwashing and clean or aseptic technique. Rationales An increased fluid intake keeps urine diluted and the flow of urine high to prevent stasis and infection. This measure reduces pathogens around the catheter. Disconnecting drainage devices from the indwelling catheter increases the risk for contamination that may lead to infection. QSEN: Safety. Acidic urine inhibits the growth of pathogenic bacteria. The use of vitamin C supplements (500 to 1000 mg/day) contributes to more acidic urine. Cranberry juice (four to six 8-ounce glasses per day) produces hippuric acid as it is metabolized and excreted in the urine. This metabolism by-product reduces urine pH. The juice may take several weeks to produce a therapeutic result. QSEN: Evidencebased practice. Specific antibiotics will reduce pathogens and resolve infection. Patients need to report signs of infection early. QSEN: Safety. For additional care plans, go to http://evolve.elsevier.com/Gulanick/. Copyright © 2018, Elsevier Inc. All Rights Reserved.