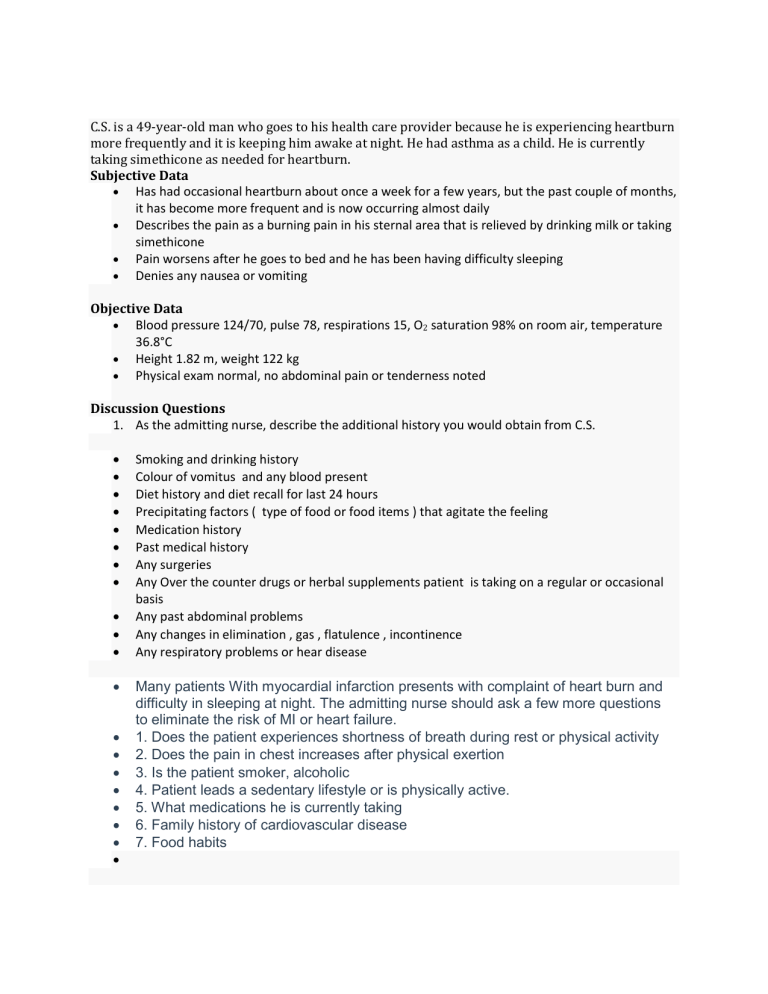
C.S. is a 49-year-old man who goes to his health care provider because he is experiencing heartburn more frequently and it is keeping him awake at night. He had asthma as a child. He is currently taking simethicone as needed for heartburn. Subjective Data Has had occasional heartburn about once a week for a few years, but the past couple of months, it has become more frequent and is now occurring almost daily Describes the pain as a burning pain in his sternal area that is relieved by drinking milk or taking simethicone Pain worsens after he goes to bed and he has been having difficulty sleeping Denies any nausea or vomiting Objective Data Blood pressure 124/70, pulse 78, respirations 15, O2 saturation 98% on room air, temperature 36.8°C Height 1.82 m, weight 122 kg Physical exam normal, no abdominal pain or tenderness noted Discussion Questions 1. As the admitting nurse, describe the additional history you would obtain from C.S. Smoking and drinking history Colour of vomitus and any blood present Diet history and diet recall for last 24 hours Precipitating factors ( type of food or food items ) that agitate the feeling Medication history Past medical history Any surgeries Any Over the counter drugs or herbal supplements patient is taking on a regular or occasional basis Any past abdominal problems Any changes in elimination , gas , flatulence , incontinence Any respiratory problems or hear disease Many patients With myocardial infarction presents with complaint of heart burn and difficulty in sleeping at night. The admitting nurse should ask a few more questions to eliminate the risk of MI or heart failure. 1. Does the patient experiences shortness of breath during rest or physical activity 2. Does the pain in chest increases after physical exertion 3. Is the patient smoker, alcoholic 4. Patient leads a sedentary lifestyle or is physically active. 5. What medications he is currently taking 6. Family history of cardiovascular disease 7. Food habits 2. The health care provider informs C.S. that he probably has gastroesophageal reflux disease (GERD). What is GERD? What are some of the predisposing factors for GERD? GERD stands for gastro oesophageal reflux disease. It is characterised by reflux of the content of the stomach into oesophagus through lower oesophageal sphincture. The symptoms include acidic taste in mouth, halitosis, nausea, vomitting, abdominal pain and discomfort, heart burn. Risk factors include obesity, pregnancy, acidity, eating spicey oily foods, taking medications like antihistamins, antidepressants, sedentary lifestyle, smoking, alcoholism. GERD is a chronic symptom of mucosal damage caused by reflux of stomach acid into the lower esophagus It is a syndrome in which the esophageal defences are overwhelmed and the refluxate causes esophaegeal irritation and inflammation ( esophagits ) PREDISPOSING FACTORS Incompetent LES Decreased LES pressure Certain drugs and foods Obesity Increased intraabdominal pressure Cigarette smoking Hiaal hernia 3. You are counseling C.S. on lifestyle modifications. What should you include for C.S.? Weight reduction Avoid foods and factors that trigger symptoms Smoking cessation Stress coping mechanisms Lifestyle modifications for GERD includes : - avoiding fatty and oily foods, spicey food - avoiding caffeine, smoking and alcohol - emphasise on moderate exercises - increase fiber intake 4. The health care provider prescribes omeprazole for C.S. and instructs him to return for a followup visit in 2 weeks if his symptoms do not improve. What is the mechanism of action of omeprazole and the rationale for returning only if symptoms persist? Mechanism of action of omeprazole - oomeprazole is a proton pump inhibitor which blocks the gastricH,K-ATPase(hydrogen/pottasium ade… oomeprazole is a proton pump inhibitor which blocks the gastricH,KATPase(hydrogen/pottasium adenosine triphosphatase enzyme) reducing the production of acid in the wall of the stomach. Its action is pronounced and long term. The patient is asked to come for follow if symptoms persist because alternative diagnosis can be made excluding GERD and also to find out weekly acidic reflux in patient and also the side effects of medicine. 5. If medications and lifestyle modifications are not effective at eliminating the symptoms of GERD, what is another option? If medicine and lifestyle changes does not work for GERD then surgeries can be done as per doctor's order.. Fundoplication -wrapping the top of stomach to tighten up the muscles to prevent reflux. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/gastroesophageal-refluxdisease-gerd-treatment key findings of heart burn Heart burn frequently at night Occurrence of heat burn almost daily Pain in sternal area relieved by drinking milk or taking antacids Pain worsens at night Difficulty sleeping Obesity The diagnosis of GERD is based mainly on symptoms. Patient presents with complaints of bad taste in moutb due to acid reflux, bad breath, heart burn, nausea, vomiting, abdominal pain and discomfort, chest pain. Avoid High fat foods, Caffeine, Chocolate, Onions, Peppermint, Carbonated beverages, Alcohol, Citrus and tomato products. Add non-citrus fruits such as bananas, melons, apples, and pears among others. Choose lean meats that are grilled, poached, broiled, or baked and egg whites Oatmeal, whole grain bread, rice, and couscous are good sources of healthy complex carbs. Whole grains and brown rice add fiber to your diet. Replace saturated fats with unsaturated ones like oils of olive, sesame, canola, and sunflower; avocados; peanuts and peanut butter; and many nuts and seeds; soybeans and tofu; and fatty fish such as salmon and trout. Potatoes and other root vegetables are great sources of healthy carbs and digestible fiber. and avoid adding onion and garlic during preparation. Sit up while eating and avoid lying flat for a minimum of two hours after eating a meal. Standing up and walking around after a meal helps encourage gastric juices to flow in the right direction. Avoid eating just before the bed time. Have dinner 2 hours before bedtime.