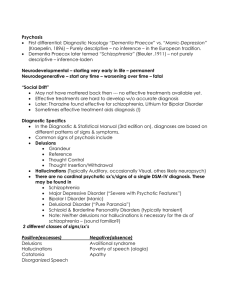
Schizophrenia spectrum and other psychotic disorders 2020 Schizophrenia spectrum and other psychotic disorders • Abnormalities in one or more of the following five domains: 1. Delusions, 2. Hallucinations, 3. Disorganized thinking (speech), 4. Grossly disorganized or abnormal motor behavior (including catatonia), 5. Negative symptoms. Delusions • Delusions are fixed beliefs that are not amenable to change in light of conflicting evidence. • Persecutory delusions (i.e., belief that one is going to be harmed, harassed), • Referential delusions (i.e., belief that certain gestures, comments, environmental cues, and so forth are directed at oneself) • Grandiose delusions (i.e., when an individual believes that he or she has exceptional abilities, wealth, or fame) • Erotomanic delusions (i.e., when an individual believes falsely that another person is in love with him or her) • Nihilistic delusions involve the conviction that a major catastrophe will occur, • Somatic delusions focus on preoccupations regarding health and organ function. Delusions • Bizarre delusions - thought withdrawal, thought insertion, delusions of control outside force has removed his or her internal organs • Nonbizarre delusion is the belief that one is under surveillance by the police, despite a lack of convincing evidence. Hallucinations • Hallucinations are perception-like experiences that occur without an external stimulus. • They are vivid and clear, with the full force and impact of normal perceptions, and not under voluntary control. • They may occur in any sensory modality • Auditory hallucinations are the most common in schizophrenia and related disorders. Disorganized Thinking formal thought disorder • Derailment or loose associations - The individual may switch from one topic to another • Tangentiality - Answers to questions may be obliquely related or completely unrelated • Incoherence or word salad- severely disorganized speech, nearly incomprehensible and resembles receptive aphasia in its linguistic disorganization • Symptom must be severe enough to substantially impair effective communication. Grossly Disorganized or Abnormal Motor Behavior • Childlike "silliness" • Unpredictable agitation. • Difficulties in performing activities of daily living Catatonic behavior is a marked decrease in reactivity to the environment. • Negativism; • Stupor and mutism • Catatonic excitement • Stereotyped movements, staring, grimacing • Echoing of speech. Catatonia A. The clinical picture is dominated by three (or more) of the following symptoms: • 1. Stupor (i.e., no psychomotor activity; not actively relating to environment). • 2. Catalepsy (i.e., passive induction of a posture held against gravity). • 3. Waxy flexibility (i.e., slight, even resistance to positioning by examiner). • 4. Mutism (i.e., no, or very little, verbal response • 5. Negativism (i.e., opposition or no response to instructions or external stimuli). • 6. Posturing (i.e., spontaneous and active maintenance of a posture against gravity). • 7. Mannerism (i.e., odd, circumstantial caricature of normal actions). • 8. Stereotypy (i.e., repetitive, abnormally frequent, non-goal-directed movements). • 9. Agitation, not influenced by external stimuli. • 10. Grimacing. • 11. Echolalia (i.e., mimicking another’s speech). • 12. Echopraxia (i.e., mimicking another’s movements). Negative Symptoms • Diminished emotional expression includes reductions in the expression of emotions in the face, eye contact, intonation of speech (prosody), and movements of the hand, head, and face that normally give an emotional emphasis to speech • Avolition is a decrease in motivated self-initiated purposeful activities. The individual may sit for long periods of time and show little interest in participating in work or social activities. Other negative • Alogia is manifested by diminished speech output. • Anhedonia is the decreased ability to experience pleasure from positive stimuli or a degradation in the recollection of pleasure previously experienced. • Poverty of content of speech. Although the patient’s replies are long enough so that speech is adequate in amount, it conveys little information. Schizophrenia Spectrum and Other Psychotic Disorder • Schizotypal (Personality) Disorder • Delusional Disorder • Brief Psychotic Disorder • Schizophreniform Disorder • Schizophrenia • Schizoaffective Disorder • Substance/Medication-Induced Psychotic Disorder • Psychotic Disorder Due to Another Medical Condition Delusional Disorder • A. The presence of one (or more) delusions with a duration of 1 month or longer • B. Criterion A for schizophrenia has never been met • Hallucinations, if present, are not prominent and are related to the delusional theme • C. Apart from the impact of the delusion(s) or its ramifications, functioning is not markedly impaired, and behavior is not obviously bizarre or odd. Specify whether: • Erotomaniac type • Grandiose type • Jealous type • Persecutory type • Somatic type • With bizarre content Prevalence • The lifetime prevalence of delusional disorder has been estimated at around 0.2% • Most frequent subtype is persecutory delusional disorder • Jealous type, is more common in males than in females, • No major gender differences in the overall frequency of delusional disorder. Differential Diagnosis • Schizophrenia and schizophreniform disorder • Obsessive-compulsive and related disorders (obsessive-compulsive disorder, with absent insight/delusional) • beliefs specifier • Depressive and bipolar disorders and schizoaffective disorder Brief Psychotic Disorder A. Presence of one (or more) of the following symptoms. At least one of these must be (1), (2), or (3): 1. Delusions 2. Hallucinations 3. Disorganized speech (e.g., frequent derailment or incoherence) 4. Grossly disorganized or catatonic behavior B. Duration of an episode of the disturbance is at least 1 day but less than 1 month, with eventual full return to premorbid level of functioning. C. The disturbance is not better explained by other psychotic disorder and is not attributable to the physiological effects of a substance or another medical condition. Specify if: • With marked stressor(s) • Without merited stressor(s) • With postpartum onset: If onset is during pregnancy or within 4 weeks postpartum • With catatonia Associated Features Supporting Diagnosis • Individuals with brief psychotic disorder typically experience emotional turmoil or overwhelming confusion • They may have rapid shifts from one intense affect to another • The level of impairment may be severe, and supervision may be required • Increased risk of suicidal behavior, particularly during the acute episode Prevalence • In the United States, brief psychotic disorder may account for 9% of cases of first-onset psychosis. • Psychotic disturbances that meet Criteria A and C, but not Criterion B, for brief psychotic disorder (i.e., duration of active symptoms is 1-6 months as opposed to remission within 1 month) are more common in developing countries than in developed countries • Brief psychotic disorder is twofold more common in females than in males. Schizophreniform Disorder • A. Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated). At least one of these must be (1), (2), or (3): • 1. Delusions. • 2. Hallucinations. • 3. Disorganized speech (e.g., frequent derailment or incoherence). • 4. Grossly disorganized or catatonic behavior. • 5. Negative symptoms (i.e., diminished emotional expression or avolition). Schizophreniform Disorder • B. An episode of the disorder lasts at least 1 month but less than 6 months. When the diagnosis must be made without waiting for recovery, it should be qualified as “provisional.” • C. Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out • D. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. Development and Course • The development of schizophreniform disorder is similar to that of schizophrenia • About one-third of individuals with an initial diagnosis of schizophreniform disorder (provisional) recover within the 6-month period and schizophreniform disorder is their final diagnosis • The majority of the remaining two-thirds of individuals will eventually receive a diagnosis of schizophrenia or schizoaffective disorder. • Schizophreniform disorder differs in duration from brief psychotic disorder, which has a duration of less than 1 month. Schizoaffective disorder • Classified as having schizoaffective disorder, atypical schizophrenia, goodprognosis schizophrenia, remitting schizophrenia, and cycloid psychosis • 1970, two sets of data shifted the view of schizoaffective disorder from a schizophrenic illness to a mood disorder: 1. Lithium 2. 1968 by John Cooper and his colleagues showed that the number of patients classified as schizophrenic in the United States and in the United Kingdom resulted from an overemphasis in the United States on the presence of psychotic symptoms as a diagnostic criterion for schizophrenia. Schizoaffective disorder • A. An uninterrupted period of illness during which there is a major mood episode (major depressive or manic) concurrent with Criterion A of schizophrenia. • B. Delusions or hallucinations for 2 or more weeks in the absence of a major mood episode (depressive or manic) during the lifetime duration of the illness. • C. Symptoms that meet criteria for a major mood episode are present for the majority of the total duration of the active and residual portions of the illness. • D. The disturbance is not attributable to the effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. Specify if: The following course specifiers are only to be used after a 1-year duration of the disorder • First episode, currently in acute episode or currently in partial remission or currently in full remission • Multiple episodes (after a minimum of two episodes) currently in acute episode currently in partial remission currently in full remission • Bipolar type • Depressive type • With catatonia Epidemiology • The lifetime prevalence range of 0.5 to 0.8% • Approximately equal numbers of men and women have the bipolar subtype and are more than twofold female to male predominance among individuals with the depressed subtype • The depressive type of schizoaffective disorder may be more common in older persons than in younger persons, and the bipolar type may be more common in young adults than in older adults. • The age of onset for women is later than that for men, as in schizophrenia. • Men with schizoaffective disorder are likely to exhibit antisocial behavior and to have a markedly flat or inappropriate affect. Schizophrenia • Lifetime prevalence of 0.6 to 1 .9 percent • Equally prevalent in men and women • The peak ages of onset are 1 0 to 25 years for men and 25 to 35 years for women • Approximately 3 to 1 0 percent of women with schizophrenia present with disease onset after age 40 years Mortality rate • Persons with schizophrenia have a higher mortality rate from accidents and natural causes than the general population • Several studies have shown that up to 80 percent of all schizophrenia patients have significant concurrent medical illnesses • 50 percent of these conditions may be undiagnosed Infection and Birth Season • More likely to have been born in the winter and early spring • Season specific risk factors, such as a virus or a seasonal change in diet, may be operative. • Gestational and birth complications, exposure to influenza epidemics, maternal starvation during pregnancy, rhesus factor incompatibility Substance abuse • The lifetime prevalence of any drug abuse (other than tobacco) is often greater than 50% • Those reporting high levels of cannabis use (more than 50 occasions) were at six fold increased risk of schizophrenia compared with nonusers • ifetime prevalence of alcohol within schizophrenia was 40 percent Other factors • Population Density - twice as high in cities as in rural communities • Socioeconomic and Cultural Factors - Patients with a diagnosis of schizophrenia are reported to account for 15 to 45 percent of homeless Americans • Patients with schizophrenia occupy about 50 percent of all mental hospital beds and account for about 1 6 percent of all psychiatric patients who receive any treatment Etiology • Schizophrenia and schizophrenia-related disorders occur at an increased rate among the biological relatives of patients with schizophrenia • 50 % concordance rate for monozygotic twins • Age of the father has a correlation with the development of schizophrenia (60 and more) • The best current candidates are a-7 nicotinic receptor, DISC 1, GRM 3, COMT, NRG 1, RGS 4, and G 72 Biological factors Neuropathology • Computed tomography (CT) scans - ventricular enlargement and some reduction in cortical volume • There is a reduced symmetry in several brain areas in schizophrenia, including the temporal, frontal, and occipital lobes • Basal ganglia - reduction of volume of the globus pallidus and the substantia nigra. Studies have also shown an increase in the number of D2 receptors in the caudate, the putamen, and the nucleus accumbens Psychoanalytic Theories • Sigmund Freud - Ego disintegration in schizophrenia represents a return to the time when the ego was not yet developed or had just begun to be established • Margaret Mahler - distortions in the reciprocal relationship between the infant and the mother. The child is unable to separate from, and progress beyond, the closeness and complete dependence that characterize the mother-child relationship in the oral phase of development. As a result, the person's identity never becomes secure • "schizophrenogenic mother" - This term designates a mother who is not capable of drawing a clear boundary between herself and her child. The double-bind concept • Learning Theories - children who later have schizophrenia learn irrational reactions and ways of thinking by imitating parents who have their own significant emotional problems Family • Schisms and Skewed Families - one parent is overly close to a child of the opposite gender. In the other family type, a skewed relationship between a child and one parent involves a power struggle between the parents and the resulting dominance of one parent. • Pseudomutual and Pseudohostile - Families. As described by Lyman Wynne, some families suppress emotional expression by consistently using pseudomutual or pseudohostile verbal communication. In such families, a unique verbal communication develops, and when a child leaves home and must relate to other persons, problems may arise. • Expressed Emotion - Parents or other caregivers may behave with overt criticism, hostility, and overinvolvement toward a person with schizophrenia. Types of Schizophrenia ICD 10 • F20.0 Paranoid schizophrenia. • F20.1 Disorganized schizophrenia. • F20.2 Catatonic schizophrenia. • F20.3 Undifferentiated schizophrenia. • F20.4 Post-Schizophrenic Depression • F20.5 Residual schizophrenia. • F20.6 Simple schizophrenia Substance/Medication-Induced Psychotic Disorder A. Presence of one or both of the following symptoms: 1. Delusions. 2. Hallucinations. B. There is evidence from the history, physical examination, or laboratory findings of both (1)and (2): 1. The symptoms in Criterion A developed during or soon after substance intoxication or withdrawal or after exposure to a medication. 2. The involved substance/medication is capable of producing the symptoms in Criterion A. Substance/Medication-Induced psychotic disorder • C. The disturbance is not better explained by a psychotic disorder that is not substance/ medication-induced. Such evidence of an independent psychotic disorder could include the following: The symptoms preceded the onset of the substance/medication use; the symptoms persist for a substantial period of time (e.g., about 1 month) after the cessation of acute withdrawal or severe intoxication • D. The disturbance does not occur exclusively during the course of a delirium. Specify if • With onset during intoxication: If the criteria are met for intoxication with the substance and the symptoms develop during intoxication. • With onset during withdrawal: If the criteria are met for withdrawal from the substance and the symptoms develop during, or shortly after, withdrawal.