Endemic Pemphigus Foliaceus in Colombia: Autoantigen Analysis
advertisement
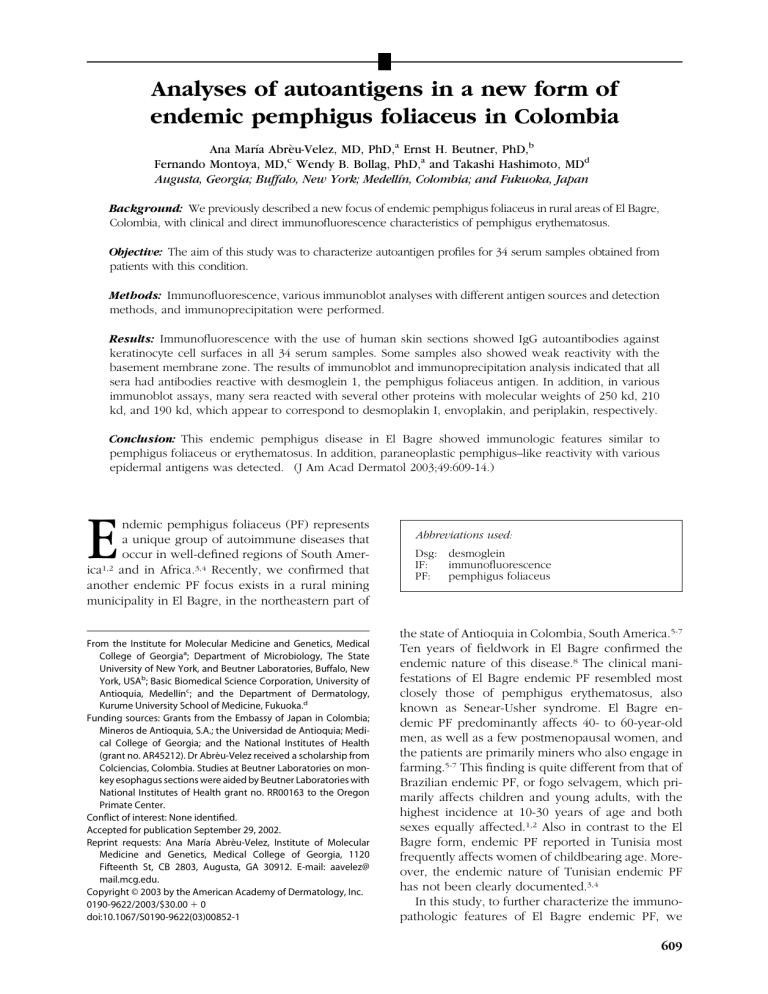
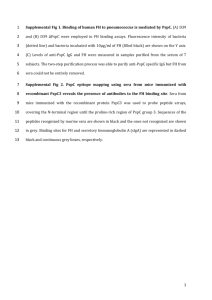
Analyses of autoantigens in a new form of endemic pemphigus foliaceus in Colombia Ana Marı́a Abrèu-Velez, MD, PhD,a Ernst H. Beutner, PhD,b Fernando Montoya, MD,c Wendy B. Bollag, PhD,a and Takashi Hashimoto, MDd Augusta, Georgia; Buffalo, New York; Medellı́n, Colombia; and Fukuoka, Japan Background: We previously described a new focus of endemic pemphigus foliaceus in rural areas of El Bagre, Colombia, with clinical and direct immunofluorescence characteristics of pemphigus erythematosus. Objective: The aim of this study was to characterize autoantigen profiles for 34 serum samples obtained from patients with this condition. Methods: Immunofluorescence, various immunoblot analyses with different antigen sources and detection methods, and immunoprecipitation were performed. Results: Immunofluorescence with the use of human skin sections showed IgG autoantibodies against keratinocyte cell surfaces in all 34 serum samples. Some samples also showed weak reactivity with the basement membrane zone. The results of immunoblot and immunoprecipitation analysis indicated that all sera had antibodies reactive with desmoglein 1, the pemphigus foliaceus antigen. In addition, in various immunoblot assays, many sera reacted with several other proteins with molecular weights of 250 kd, 210 kd, and 190 kd, which appear to correspond to desmoplakin I, envoplakin, and periplakin, respectively. Conclusion: This endemic pemphigus disease in El Bagre showed immunologic features similar to pemphigus foliaceus or erythematosus. In addition, paraneoplastic pemphigus–like reactivity with various epidermal antigens was detected. (J Am Acad Dermatol 2003;49:609-14.) E ndemic pemphigus foliaceus (PF) represents a unique group of autoimmune diseases that occur in well-defined regions of South America1,2 and in Africa.3,4 Recently, we confirmed that another endemic PF focus exists in a rural mining municipality in El Bagre, in the northeastern part of From the Institute for Molecular Medicine and Genetics, Medical College of Georgiaa; Department of Microbiology, The State University of New York, and Beutner Laboratories, Buffalo, New York, USAb; Basic Biomedical Science Corporation, University of Antioquia, Medellı́nc; and the Department of Dermatology, Kurume University School of Medicine, Fukuoka.d Funding sources: Grants from the Embassy of Japan in Colombia; Mineros de Antioquia, S.A.; the Universidad de Antioquia; Medical College of Georgia; and the National Institutes of Health (grant no. AR45212). Dr Abrèu-Velez received a scholarship from Colciencias, Colombia. Studies at Beutner Laboratories on monkey esophagus sections were aided by Beutner Laboratories with National Institutes of Health grant no. RR00163 to the Oregon Primate Center. Conflict of interest: None identified. Accepted for publication September 29, 2002. Reprint requests: Ana Marı́a Abrèu-Velez, Institute of Molecular Medicine and Genetics, Medical College of Georgia, 1120 Fifteenth St, CB 2803, Augusta, GA 30912. E-mail: aavelez@ mail.mcg.edu. Copyright © 2003 by the American Academy of Dermatology, Inc. 0190-9622/2003/$30.00 ⫹ 0 doi:10.1067/S0190-9622(03)00852-1 Abbreviations used: Dsg: desmoglein IF: immunofluorescence PF: pemphigus foliaceus the state of Antioquia in Colombia, South America.5-7 Ten years of fieldwork in El Bagre confirmed the endemic nature of this disease.8 The clinical manifestations of El Bagre endemic PF resembled most closely those of pemphigus erythematosus, also known as Senear-Usher syndrome. El Bagre endemic PF predominantly affects 40- to 60-year-old men, as well as a few postmenopausal women, and the patients are primarily miners who also engage in farming.5-7 This finding is quite different from that of Brazilian endemic PF, or fogo selvagem, which primarily affects children and young adults, with the highest incidence at 10-30 years of age and both sexes equally affected.1,2 Also in contrast to the El Bagre form, endemic PF reported in Tunisia most frequently affects women of childbearing age. Moreover, the endemic nature of Tunisian endemic PF has not been clearly documented.3,4 In this study, to further characterize the immunopathologic features of El Bagre endemic PF, we 609 610 Abrèu-Velez et al J AM ACAD DERMATOL OCTOBER 2003 demonstrated the presence of autoantibodies to various autoantigens in patients with this disease by means of various immunologic and biochemical methods, including immunofluorescence (IF), immunoblot, and immunoprecipitation. MATERIALS AND METHODS Sera and antibodies For this study, we used sera from 34 patients with El Bagre endemic PF in a clinically active stage. These sera were randomly selected from the stock collected during our 10-year survey in the endemic areas of El Bagre. The criteria for diagnosis of this disease have been previously described.5-7 All patients participated willingly in this study and gave informed consent. As controls, serum samples were collected from 34 healthy persons living in nonendemic areas in Medellı́n, Colombia, and having a similar but not identical ethnic background to the endemic PF patients. These nonendemic controls were about 50% American Indian and white (mestizo), 40% white, 6% American Indian and black (zambo), 4% white and black (mulatto), and a few American Indians, most of whom were only temporarily visiting the city.9 We also tested 34 matched controls from the endemic area of El Bagre, identical in age, sex, and ethnic background to the PF patients from the endemic area. The El Bagre population includes about 41% mestizos, 15% whites, 14% zambos, 3% mulattoes, and 1% American Indians.10 The proportions of the individuals studied reflect the ethnic backgrounds in the respective regions. Finally, sera from 34 patients with nonendemic (sporadic) PF, 3 typical bullous pemphigoid patients, and 3 typical paraneoplastic pemphigus patients from Medellı́n city were used as additional controls. IF analysis Indirect IF with sections of normal human skin was performed by means of standard methods.11 To determine IgG subclasses, fluorescence-conjugated mouse monoclonal antibodies specific to human IgG1-4 (Sigma, St Louis, Mo) were used. Immunoblot analysis We performed various immunoblot methods using different antigen sources and different detection procedures to identify possible autoantigens recognized by the El Bagre endemic PF sera. Normal human epidermis (full thickness) was split with a dermatome, powdered using liquid nitrogen, and prepared as described previously.12 The extracts of 1mol/L NaCl-split human epidermis were also prepared as previously described.13 For the third antigen source, we prepared extracts of cultured Fig 1. The results of indirect IF using human skin sections and a representative El Bagre endemic PF serum. a, IgG reactivity with keratinocyte cell surfaces (small arrow) and weak reactivity with the basement membrane zone (large arrow). b, IgG4 reactivity with cell surfaces (arrows) is illustrated. MCF-12 cells, a human mammary epithelial cell line (American Type Culture Collection). Detection with the use of alkaline phosphatase– conjugated secondary antibodies was performed with standard methods. Detection using iodine 125– labeled protein A was performed as reported previously.14-18 We also utilized a chemiluminescence detection procedure (SuperSignal; Pierce, Milwaukee, Wis). Mouse monoclonal antibodies to desmoglein 1 (Dsg1) and desmoplakin were obtained from Progen Biotech (Heidelberg, Germany). Immunoprecipitation analysis Protein samples were released from bovine snout epidermis by means of trypsin digestion and purified with the use of a concanavalin A column. These proteins were radiolabeled with iodine 125 by means of the chloramine-T method, as described previously.14,18 Immunoprecipitation was performed as described previously.14-18 RESULTS IF studies Indirect IF with the use of human skin sections showed IgG antikeratinocyte cell surface antibodies in all 34 El Bagre endemic PF serum samples (Fig 1, a). Furthermore, 7 (20%) of the sera showed IgG anti– basement membrane zone antibodies, although the reactivity was weak. Indirect IF with monoclonal antibodies to human IgG subclasses showed that all 34 endemic PF sera contained IgG4 antibodies to the keratinocyte cell surface (Fig 1, b). In addition, 9 (26%) sera showed IgG1 anti– cell surface antibodies, but no sera showed either IgG2 or IgG3 antibodies. Some sera also showed IgG4 antibodies to the basement membrane zone, although the reactivity was again weak (data not shown). All 34 sporadic nonendemic PF sera also showed IgG anti– cell surface antibodies and contained specifically IgG4-type antibodies, while no sera showed Abrèu-Velez et al 611 J AM ACAD DERMATOL VOLUME 49, NUMBER 4 reactivity with the basement membrane zone. Interestingly, 3 (9%) sera of the 34 healthy persons in endemic areas showed IgG anti– cell surface antibodies (data not shown), while none of the 34 sera from the healthy persons in nonendemic areas had this reactivity. antibody and sporadic PF sera. The 250-kd protein comigrated with the protein detected by an antidesmoplakin monoclonal antibody. In addition, the 210-kd and 190-kd proteins comigrated with envoplakin and periplakin, which were identified with the use of paraneoplastic pemphigus sera. Immunoblot studies With the use of extracts of full-thickness epidermis as an antigen source and alkaline phosphatase– labeled secondary antibody for detection, immunoblot analysis showed that 11 (33%) of the 34 El Bagre endemic PF sera recognized a 160-kd protein band (Fig 2, a). This band comigrated with Dsg1, which also was detected in approximately one third of the 34 sporadic PF sera. However, other protein bands with molecular weights of approximately 250 kd, 210 kd, and 190 kd were also detected in 12 (35%) endemic PF sera. An antidesmoplakin monoclonal antibody reacted with the 250-kd desmoplakin I, which comigrated with the 250-kd antigen recognized by endemic PF sera. This monoclonal antibody did not show clear reactivity with the 210-kd desmoplakin II, probably because the amount of desmoplakin II was too little to be detected. All three paraneoplastic pemphigus sera also showed reactivity with 210-kd and 190-kd proteins (data not shown). Surprisingly, 8 (23%) of the 34 sera from healthy persons in the endemic area also showed reactivity with the 160-kd protein (data not shown). Similar reactivity was observed when chemoluminescence was used as a detection procedure in place of the alkaline phosphatase–labeled secondary antibody (data not shown). In addition, we performed immunoblot analysis using iodine 125–labeled secondary antibodies for detection. With this method, 11 (33%) endemic PF sera showed the 160-kda protein in the extracts of 1mol/L NaCl-split epidermis (Fig 2, b). In addition, 13 (38%) of the 34 endemic PF sera exhibited reactivity with several other protein bands, particularly those with molecular weights of approximately 250 kd and 210 kd. The 250-kd protein comigrated with the protein shown by antidesmoplakin monoclonal antibody. The 160-kd Dsg1 was also shown by 11 (33%) sporadic PF sera. With immunoblot analysis, we further characterized the recognized antigens using MCF-12 cell extracts as an antigen source and alkaline phosphatase–labeled secondary antibody to visualize reactivity, since this method showed various protein bands most clearly. With this method, 15 (44%) endemic PF sera reacted with proteins of molecular weights of about 300 kd, 250 kd, 210 kd, 190 kd, and 160 kd (Fig 2, c). The 160-kd protein comigrated with Dsg1 detected by an anti-Dsg1 monoclonal Immunoprecipitation studies Immunoprecipitation analysis with trypsin-released radiolabeled proteins from bovine snout epidermis showed that 32 (94%) of 34 endemic PF sera clearly immunoprecipitated a 45-kd protein band (Fig 3). In previous studies, this 45-kd protein was shown to be an extracellular fragment of Dsg1 by excision of the band and amino acid sequence analysis. The sequence thus obtained, EXIKFAAAXREGED, matched the N-terminal domain of the mature form of bovine Dsg1.16,17,19 The 45-kd band was recognized by all PF sera and in all patients affected with El Bagre endemic PF. Three sera obtained from patients with mild conditions showed relatively weak reactivity with the 45-kd protein (data not shown). Interestingly, some endemic PF sera were able to immunoprecipitate several other protein bands of approximately 80 kd and 34 kd (Fig 3). These protein bands may be related to the other antigens detected by means of immunoblot, such as the plakin family proteins; however, the proteins were detected in association with strong reactivity to the 45-kd Dsg1 fragment. It is also plausible that these proteins are related to Dsg1 or are degradation products of Dsg1. Three (9%) of the sera from healthy individuals in the endemic area also precipitated the 45-kd protein, as well as other proteins of about 80 kd and 34 kd (Fig 3). None of the healthy persons in nonendemic areas showed positive reactivity (data not shown). DISCUSSION In this study, we found with indirect IF that all endemic PF sera possessed circulating IgG autoantibodies reactive with the keratinocyte cell surfaces, the gold standard for the diagnosis of pemphigus.9 Thus this result confirms the autoimmune nature of this new endemic PF in El Bagre, Colombia. The IgG subclass study revealed the predominant subclass to be IgG4, as has been shown previously for other forms of endemic PF.20 In addition, some endemic PF sera showed circulating IgG (particularly, IgG4) anti– basement membrane zone antibodies, although the significance of this finding and the antigens recognized by these autoantibodies are not clear. The presence of anti– basement membrane zone autoantibodies has also been reported in a few cases of Brazilian endemic PF, although this reactivity was not carefully stud- 612 Abrèu-Velez et al J AM ACAD DERMATOL OCTOBER 2003 Fig 3. Results of immunoprecipitation analysis using a trypsin-released radiolabeled protein sample from bovine snout epidermis. Endemic PF sera recognized a 45-kd protein, representing a fragment of Dsg1 (EPF, lanes 2-6). In addition, these sera also reacted with several other molecules in the region of 80 kd and 34 kd. Serum from a sibling of an endemic PF patient also showed similar reactivity (SIB, lane 7). In contrast, a sporadic PF serum reacted with the 45-kd Dsg1 fragment but not with other proteins (lane 1). A representative normal serum from the nonendemic area did not show any specific reactivity (lane 8). The position of the 45-kd fragment is shown to the left. Fig 2. Results of immunoblot studies using different antigen sources and detection methods. a, The results of immunoblot analysis with extracts of keratome-separated epidermis, alkaline phosphatase– conjugated secondary antibody, and PF serum (lane 2) are illustrated. Four representative El Bagre endemic PF sera (EPF, lanes 4-7) also reacted with a 160-kd protein. In addition, the endemic PF sera reacted with several other proteins, particularly 250kd, 210-kd, and 190-kd proteins. An antidesmoplakin monoclonal antibody reacted with 250-kd desmoplakin I (DPL, lane 1), which comigrated with the 250-kd antigen recognized by endemic PF sera. A bullous pemphigoid serum reacted with the 180-kd bullous pemphigoid antigen (BP, lane 3); whereas normal serum did not show any specific reactivity (lane 8). b, The results of immunoblot analysis with extracts of 1M NaCl-split epidermis and iodine 125– conjugated secondary antibody show that the antidesmoplakin monoclonal antibody reacted with the 250-kd desmoplakin I (DPL, lane 1). An anti-Dsg1 monoclonal antibody (lane 2) and a PF serum (lane 3) reacted with 160-kd Dsg1. Three of the 4 representative El Bagre endemic PF sera (EPF, lanes 4-7) also reacted with a 160-kd protein. In addition, all endemic PF sera reacted with the 250-kd and 210-kd proteins. Reactivity with a 190-kd protein was not observed. Normal serum showed no specific reactivity (lane 8). The broad band seen in the lower portion of each lane is nonspecific reactivity with the large quantities of keratins in these extracts. c, Immunoblot analysis with extracts of MCF-12 cells and alkaline phosphatase– conjugated secondary antibody shows that an antidesmoplakin monoclonal antibody reacted with 250-kd desmoplakin I (DPL, lane 1). An anti-Dsg1 monoclonal antibody (lane 2) and PF serum (lane 3) reacted with 160-kd Dsg1. A paraneoplastic pemphigus serum showed reactivity with 210-kd envoplakin and 190-kd periplakin, as well as many lower molecular weight protein bands (PNP, lane 4). All 4 endemic PF sera reacted with the 160-kd, the 210-kd, and the 190-kd proteins (EPF, lanes 5-8). Two of 4 endemic PF sera reacted with the 250-kd protein (lane 6). The molecular weight of each recognized protein is indicated to the left. J AM ACAD DERMATOL VOLUME 49, NUMBER 4 ied.21 In vivo deposition to the basement membrane zone was found in 8 (17%) of 47 Brazilian endemic PF skin biopsy specimens, but the authors described this finding as nonspecific reactivity.22 Nearly all of the El Bagre endemic PF sera reacted specifically with Dsg1, the PF antigen,18 in both human and bovine protein samples using immunoblot and immunoprecipitation methods, as well as a newly developed enzyme-linked immunosorbent assay.18 This result further indicates the similarity of this disease to Brazilian endemic PF, in which about one-third of fogo selvagem sera have autoantibodies against linear epitopes of Dsg1 and almost all cases recognize a conformational epitope of the 45-kd Dsg1 antigen by means of immunoprecipitation.15,16,18 Because Tunisian endemic PF patients showed variable reactivity with either Dsg1 or Dsg3,4 this type of endemic PF does not seem to be closely related to endemic PF in Colombia and Brazil. However, the most interesting and puzzling finding was the complex immunoreactivity exhibited by the El Bagre endemic PF sera as shown with immunoblot studies. These experiments showed that a considerable number of El Bagre endemic PF sera reacted with multiple protein bands, particularly 250-kd, 210-kd, and 190-kd proteins. Studies using specific monoclonal antibodies and paraneoplastic pemphigus serum indicated that the 250-kd protein was likely desmoplakin I and the 210-kd and 190-kd doublet proteins were envoplakin and periplakin, respectively. This potential reactivity with various plakin family proteins may indicate a possible relationship between El Bagre endemic PF and paraneoplastic pemphigus.23-25 This possibility would then suggest the idea that paraneoplastic pemphigus could be the result of viral activation of the hematologic malignancy and not a paraneoplastic phenomenon per se. However, to date no reports indicate that viral activation occurs and plays a role in the production of these autoantibodies in paraneoplastic pemphigus. Therefore, presently we have no evidence that the production of antidesmoplakin antibodies in paraneoplastic pemphigus or in endemic PF is related to viral infection in affected patients.23-25 The heterogeneous reactivity with multiple antigens shown by the sera of El Bagre endemic PF patients has not been clearly described in Brazilian endemic PF.26,27 Therefore, the results of this study suggest that there is a difference between Brazilian endemic PF and El Bagre endemic PF, although the two diseases occur inside South America and have many identical features. Interestingly, some sera from healthy individuals living in the endemic area Abrèu-Velez et al 613 around El Bagre showed IgG anti– cell surface antibodies by indirect IF and reacted with Dsg1 and other El Bagre endemic PF–related molecules with both immunoblot and immunoprecipitation analyses. This reactivity was not seen in healthy persons living in nonendemic areas. These results are consistent with the finding that some sera from healthy persons living in Brazilian endemic PF areas frequently have anti-Dsg1 autoantibodies.27 Therefore, it is conceivable that environmental factors present in the endemic areas are responsible for the development of endemic PF both in Brazil and in El Bagre, Colombia. An additional puzzling result was the observation that a considerable number of serum samples from patients with endemic PF and those with sporadic PF reacted with a Dsg1-like 160-kd protein in extracts of MCF-12 cells, which were originally derived from mammary cells. This protein may not be Dsg1 but another molecule with the same molecular weight or a similar conformational epitope. However, because the protein specifically reacted with endemic PF and nonendemic PF sera, and because epidermal-specific Dsg may be expressed in some cultured nonepidermal cells, such as MDCK cells,28 we considered the possibility that Dsg1 may be expressed in MCF-12 cells in cell culture. Indeed, a monoclonal antibody to Dsg1 also recognized this 160-kd protein in extracts of MCF-12 cells, suggesting that this protein is Dsg1 or a closely related protein. Although the present study is still somewhat preliminary, this research clarifies the immunologic nature of endemic PF in El Bagre and further suggests some unique, yet unknown, pathogenic mechanism specific for this disease. Further studies using modern molecular biologic techniques are in progress to better characterize the autoimmune mechanism mediating this interesting disease. We extend our thanks to the people of El Bagre and to all public and private companies in Colombia that supported our program. We also acknowledge our co-workers who participated in the visits to El Bagre for their contribution to this research and humanitarian program. We gratefully appreciate Francois Tron, MD, Joly Pascal, MD, Fabianne Jouen-Beades, MD, Danielle Gilbert, PhD, and Vincent Saulot, PhD, Institut National de la Santé et de la Recherche Médicale (INSERM), France, for their kind encouragement and for generously providing us with the MCF-12 cells. In addition, we thank Rhea-Beth Markowitz, PhD, of the Medical College of Georgia for her excellent editorial assistance. This article represents a portion of the PhD thesis of Ana Marı́a Abrèu-Velez, who received a scholarship from Colciencias, Colombia, administered by the Latin American Scholarship Program of American Universities (USA). 614 Abrèu-Velez et al REFERENCES 1. Castro RM, Proenca NG. Similarities and differences between South American pemphigus foliaceus and Cazanave’s pemphigus foliaceus. Anais Bras Dermatol 1983;53:137-9. 2. Chiossi MP, Roselino AM. Pemphigus foliaceus (“Fogo selvagem”): a series from the Northeastern region of the State of Sao Paulo, Brazil, 1973-1998. Rev Inst Med Trop Sao Paulo 2001;43: 59-62. 3. Morini JP, Jomaa B, Gorgi Y, Saguem MH, Nouira R, Roujeau JC, et al. Pemphigus foliaceus in young women. An endemic focus in the Sousse area of Tunisia. Arch Dermatol 1993;129:69-73. 4. Joly P, Mokhtar I, Gilbert D, Thomine E, Fazza B, Bardi R, et al. Immunoblot and immunoelectron microscopic analysis of endemic Tunisian pemphigus. Br J Dermatol 1999;140:44-9. 5. Abreu AM, Yepes MM, León W. Pemphigus Abreu-Manu. A lost link in skin autoimmunity in endemic fashion. J Invest Dermatol 2000;114:846a. 6. Abreu AM, Maldonado JG, Jaramillo A, Patiño PJ, Prada S, Leon W, et al. Immunological characterization of a unique focus of endemic pemphigus foliaceus in the rural area of El Bagre, Colombia. J Invest Dermatol 1998;110:516a. 7. Abreu AM, León W, Hashimoto K. An autoimmune skin disease with simultaneously acantholysis between keratinocytes and separation of the basal membrane zone of the skin. J Invest Dermatol 1999;112:614a. 8. Abrèu-Velez AM, Hashimoto T, Bollag WB, Arroyave ST, AbrèuVelez CE, Londoño ML, et al. A unique form of endemic pemphigus in northern Colombia . J Am Acad Dermatol 2003;49:599608. 9. Bravo ML, Valenzuela YC, Arcos-Burgos OM. Polymorphisms and phyletic relationships of the Paisa community from Antioquia (Colombia). Gene Geogr 1996;10:11-7. 10. Angulo Mira G. Monografia de El Bagre: 50 Barras de Oro [Monograph of El Bagre: 50 gold bars]. In: Ciudades de Antioquia [Antioquia’s Cities]. Barranquilla (Colombia): Tipográficas de Bedont; 1985. p.17-111. 11. Beutner EH, Prigenzi LS, Hale W, Leme CA, Bier OG. Immunofluorescence studies of autoantibodies to intercellular areas of epithelia in Brazilian pemphigus foliaceus. Proc Soc Exp Biol Med 1968;127:81-6. 12. Calvanico NJ, Swartz SJ, Diaz LA. Affinity immunoblotting studies on the restriction of autoantibodies from endemic pemphigus foliaceus patients. J Autoimmun 1993;6:145-57. 13. Jenkins RE, Rodenas J, Bhogal BS, Black MM. Optimal conditions of 1 M NaCl splitting technique to demonstrate basement membrane zone antigens in bullous pemphigoid, epidermolysis bullosa acquisita and linear IgA bullous dermatoses. Dermatology 1994;189(suppl):133-4. 14. Calvanico NJ, Swartz SJ. A non-desmoglein component of bovine epidermis reactive with pemphigus foliaceus sera. J Autoimmun 1994;7:231-42. 15. Labib RS, Camargo S, Futamura S, Martins R, Anhalt GJ, Diaz LA. Pemphigus foliaceus antigen: characterization of a keratinocyte envelope associated pool and preparation of a soluble immunoreactive fragment. J Invest Dermatol 1989;93:272-9. J AM ACAD DERMATOL OCTOBER 2003 16. Martins CR, Labib RS, Rivitti EA, Diaz LA. A soluble and immunoreactive fragment of pemphigus foliaceus antigen released by trypsinization of viable human epidermis. J Invest Dermatol 1990;95:208-2. 17. Chen P, Hussain A, Tai HH, Dittert LW. An improved method of radioiodination with chloramine T [published correction appears in Anal Biochem 1995;225:379]. Anal Biochem 1994;219: 159-61. 18. Abreu AM, Olague-Marchan M, Lopez-Swiderski A, Mascaro JM, Giudice GJ, Diaz LA. Characterization of 45 kD epidermal tryptic peptide recognized by pemphigus foliaceus sera. J Invest Dermatol 1997;108:541a. 19. Abrèu-Velez AM, Abrèu-Velez CE, Patiño PJ, Montoya F, Bollag WB. The tryptic cleavage product of the mature form of the bovine desmoglein 1 ectodomain is one of the antigen moieties immunoprecipitated by all sera from symptomatic patients affected by a new variant of endemic pemphigus. Eur J Dermatol In press. 20. Rock B, Martins CR, Theofilopoulos AN, Balderas RS, Anhalt GJ, Labib RS, et al. The pathogenic effect of IgG4 autoantibodies in endemic pemphigus foliaceus (fogo selvagem). N Engl J Med 1989;320:1463-9. 21. Silva dos Reis VM, Cuce LC, Rivitti EA. Anatopatologia e imunofluorescencia direta e indireta das lesoes de penfigo foliaceo endemico resistentes a corticoterapia [Anatopathological, direct and indirect immunofluorescence analysis on lesions from patients with endemic pemphigus foliaceus resistant to steroid therapy]. Rev Inst Med Trop Sao Paulo 1991;33:97-103. 22. Mey O, Rodriguez RML, Myyauchi L. Immunofluorescencencia direta em biopsia de pele no penfigo foliaceo brasileiro [Direct immunofluorescence analysis from patients with endemic pemphigus foliaceus]. Anais Bras Dermatol 1981;56:131-4. 23. Anhalt GJ. Paraneoplastic pemphigus. Adv Dermatol 1997;12: 77-96. 24. Hashimoto T, Amagai M, Watanabe K, Chorzelski PT, Bhogal BS, Black MM, et al. Characterization of paraneoplastic pemphigus autoantigens by immunoblot analysis. J Invest Dermatol 1995; 104:829-34. 25. Nagata Y, Karashima T, Watt FM, Salmhofer W, Kanzaki T, Hashimoto T. Paraneoplastic pemphigus sera react strongly with multiple epitopes on the various regions of envoplakin and periplakin, except for C-terminal homologous domain of periplakin. J Invest Dermatol 2001;116:556-63. 26. Ogawa MM, Hashimoto T, Konohana A, Castro RM, Nishikawa T. Immunoblot analyses of Brazilian pemphigus foliaceus antigen using different antigen sources. Arch Dermatol Res 1990;282: 84-88. 27. Warren SJ, Lin MS, Giudice GJ, Hoffmann RG, Hans-Filho G, Aoki V, et al. The prevalence of antibodies against desmoglein 1 in endemic pemphigus foliaceus in Brazil. Cooperative Group on Fogo Selvagem Research. N Engl J Med 2000;343:23-30. 28. Vilela MJ, Hashimoto T, Nishikawa T, North AJ, Garrod DR. A simple epithelial cell line (MDCK) shows heterogeneity of desmoglein isoforms, one resembling pemphigus vulgaris antigen. J Cell Sci 1995;108:1743-50.