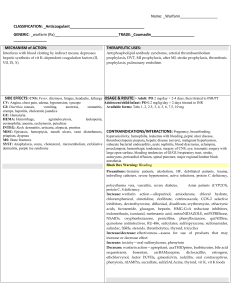
MEDICATION ADMINISTRATION WORKSHEET Medication: Generic/Trade name Classification Usual Dosage (Routes of Administration) Dosage/Route Hydrochlorothiazide Diuretics 25mg PO daily By mouth or in combination with other antihypertensive Clinical Simulation (NUR 360 Clinical Simulation ) Action Side Effects/Drug Nursing Management (Implications & Teachings) Onset/Peak/ Interactions/ Duration Contraindications O: 2hrs P: about 4hrs D: up to 24hrs S: Hypokalemia, dizziness, headache, weakness and dehydration and hyponatremia I: Drug interaction is adjunctive therapy in edema associated with congestive heart failure, hepatic cirrhosis, and corticosteroid and estrogen therapy C: anuria, hypersensitivity to this product or to other sulfon­amide-derived drugs. Gilipizide Sulfonylureas 10mg PO b.i.d. IV or by mouth O: 15-30mins P: 1-2hrs D: up to 24hrs S: Diarrhea, constipation, n/v, loss of appetite, headache, weight gain, skin change, drowsiness, dizziness I: Assess fluid status, monitor daily weight, I&O ratios, lung sounds, skin turgor, and mucous membrane, assess for confusion and excessive thirst, monitor BP before and during administration. Monitor electrolytes (esp. potassium), blood glucose, BUN, serum acid before and periodically throughout treatment Indications for Use/Indication for This Patient Indicated for the treatment of hypertension. This fixed combination drug is not indicated for the initial therapy of hypertension. T: Monitor weight daily, consult a physician before using OTC drugs because they may contain large amounts of sodium and/or potassium, change positions slowly, report signs of hypokalemia and diabetic pt need to monitor blood glucose closely. I: Monitor CBC periodically during therapy, report decrease in in blood counts, toxicity: overdose is manifested as symptoms of hypoglycemia, mild: treated w/ oral glucose, severe: IV D50W followed by continuous IV Control of blood glucose in type 2 diabetes mellitus when diet therapy fails. I: Drug interaction is concurrent use with warfarin may alter the response to both agents, beta blockers may mask the s/s of hypoglycemia C: Contraindication includes low blood sugar, addison’s disease, liver problems, decreased kidney function, alcoholism, severe n/v By mouth Rosuvastatin Statin 20mg PO every evening O: unknown P: 2-4 week D: unknown S: CNS: amnesia, confusion, dizziness, headache, insomnia, memory loss, weakness CV: chest pain, peripheral edema Derm: rash, pruritus EENT: Rhinitis Endo: hyperglycemia GI: abdominal cramps, constipation, diarrhea, flatus, heartburn GU: Erectile dysfunction Resp: bronchitis MS: Rhabdomyolysis infusion of more dilute dextrose solution to keep serum glucose at approx. 100mg/Dl T: Take medication at the same time each day, if miss dose, take soon as they remember unless it is close to take their next dose, explain that it is to help control hyperglycemia not cure diabetes – long term use, encourage to follow prescribed diet, medication, and exercise to prevent hyperglycemia or hypoglycemia episodes, notify healthcare provider if they notice changes in weight gain, swelling of ankles, drowsiness, muscle cramp, weakness, sore throat, rash, or unusual bleeding I: Can be taken at any time of day. Avoid large amounts of grapefruit juice during therapy; may increase toxicity. T: Instruct patient to take medication as directed and not to skip doses or double up on missed doses. No more than 200 mL/day of grapefruit juice. This medication should be used in conjunct with diet restrictions, exercise and cessation of smoking. Notify health care provider if signs of liver injury or if unexplained muscle pain, Slow progress of coronary atherosclerosis. Primary prevention of cardiovascular disease in patients without clinically evident coronary heart disease but with an increased risk of cardiovascular disease because of age Other: Hypersensitivity reactions I: ? C: Severe renal impairment. Avoid use during pregnancy. Avoid breast feeding if treatment is necessary Metoprolol succinate Beta blocker 100 mg PO daily By mouth O: 15mins P: unknown D: 6-12hrs S: Fatigue, weakness, HF, bradycardia, pulmonary edema I: increased hypertension may occur with other antihypertensives, May alter the effectiveness of insulins or oral hypoglycemic agents C: severe bradycardia, second or third heart block, cardiogenic shock, or decompensated cardiac failure Enoxaparin Anticoagulant 40mg subcutaneously daily Subcutaneously or IV O: Unknown P: 3-5 hr D: 12 hr S: CNS: dizziness, headache, insomnia. CV: edema. Derm: alopecia, ecchymoses, pruritis, rash, urticaria. GI: Constipation, increase liver enzymes, N/V. Hemat: Bleeding, anemia, tenderness, or weakness occurs, especially if accompanied with malaise or fever. Importance of follow-up exams to determine effectiveness and to monitor side effects I: Monitor BP, ECG, and pulse frequently during dose adjustment and periodically during therapy, monitor VS and ECG every 5-15mins during and several hrs after parenteral administration. If HR <40 bpm, especially if cardiac output is also decreased, administer atropine 0.25-0.5 mg IV, and monitor I&O and daily weights. Assess s/s of HF. Decreased blood pressure and heart rate T: Instruct to weight daily, advise to regularly check BP, and follow instructions for increasing medication dosage I: assess or signs of bleeding and hemorrhage. Assess for evidence of thrombosis. Monitor CBC, platelet, and stools for bleeding. Recheck for order of this drug. To avoid the loss of this drug, do not expel the air bubble before injection DVT with or without PE (with warfarin) thrombocytopenia. Local: erythema at injection site, hematoma, irritation, pain. MS: osteoporosis. Other: Fever I: Risk of bleeding. Risk for toxicity (protamine sulfate) T: Advise to report any symptoms of dizziness, bruising, itching, rash, fever, swelling, or difficulty breathing to health care professional immediately. Do not take with aspirin or NSAIDs. Correct technique for selfinjection, care and disposal of equipment. C: History of HIT within the past 100 days or in the presence of circulating antibodies. Hypersensitivity to specific agents, infarctional heparin or pork products. Active major bleeding. Severe hepatic or renal disease Warfarin Anticoagulant 7.5mg PO daily by mouth O: 36-72hr P: 5-7 days D: 2-5 days (after d/c) S: dermal necrosis, cramps, nausea, calciphylaxis, bleeding, fever I: Chronic use of acetaminophen may increase the risk bleeding C: uncontrolled bleeding, open wounds, severe liver or kidney disease, uncontrolled hypertension I: assess for signs of bleeding and hemorrhage (bleeding gums, nosebleed, unusual bruising, tarry, black stools, hematuria, fall in hematocrit or BP), Monitor PT, INR and other clotting factors. (PT: 1.3-1.5, INR 2.5-3.5) Pt over 60yrs exhibit greater than expected PT/INR response. Monitor for side effects at lower therapeutic ranges. Monitor stool and urine for occult blood before and periodically during therapy. Toxicity/Overdose: withhold 1 or more doses is sufficient if INR is excessively elevated or minor Prophylaxis and treatment of atrial fibrillation with embolization bleeding occurs; vitamin K if overdose occurs T: Advise to report any s/s of unusual bleeding/bruising and pain, color, or temperature change to any area of the body. Instruct pt to not drink alcohol or take Rx, OTC, or herbal products especially those containing aspirin or NSAIDs, or to start or stop any new medications during warfarin therapy without physician consent. Emphasize the importance of frequent lab tests to monitor coagulation factors Percocet Opioid 10 mg Oxycodone/ 500mg ASAP PO; every 6hrs as needed for pain rated 7-10 Tablets or by mouth O: 10-15 min P: 60-90 mins D: 3-6 hr S: CNS: confusion, sedation, dizziness, dysphoria, euphoria, floating feeling, hallucinations, headache, unusual dreams. CV: orthostatic hypotension. Derm: flushing, sweating. EENT: blurred vision, diplopia, miosis. Endo: adrenal insufficiency. GI: constipation, dry mouth, choking, GI obstruction, N/V. Resp: respiratory depression. Tolerance, dependence. I: additive CNS depression with alcohol, antihistamines and I: Assess type, location and intensity of pain prior to and 1 hr peak after admin. Assess BP, pulse, respirations before and periodically during admin. Assess for opioid addiction, abuse, or misuse prior to admin. Toxicity and overdose. T: When and how to ask for and take meds. Advise that oxycodone is a drug with a known abuse potential. May cause drowsiness or dizziness. Ta take position changes slowly; fall risk. Encourage to turn, cough and breathe deeply every 2 hr to prevent atelectasis. Moderate to severe pain sedative/hypnotics. Risk for opioid toxicity C: Significant respiratory depression; paralytic ileus, acute or severe bronchial asthma, Hypersensitivity. Ofirmev Analgesic 1g IV every 6hrs x 48 hrs then d/c IV drug O: within 30 minutes P: 30 minutes D: 4 to 6 hours S: nausea, vomiting, headache, sleep problem, constipation, itching, agitation I: Chronic oral acetaminophen use at a dose of 4000 mg/day has been shown to cause an increase in international normalized ratio (INR) in some patients who have been stabilized on sodium warfarin as an anticoagulant C: hypersensitivity to acetaminophen or phenacetin; use with alcohol. I: Monitor for S&S of: hepatotoxicity, even with moderate acetaminophen doses, especially in individuals with poor nutrition or who have ingested alcohol over prolonged periods; poisoning, usually from accidental ingestion or suicide attempts; potential abuse from psychological dependence (withdrawal has been associated with restless and excited responses). T: Do not take other medications (e.g., cold preparations) containing acetaminophen without medical advice; overdosing and chronic use can cause liver damage and other toxic effects, Do not self-medicate adults for pain more than 10 d without consulting a physician, Do not use this medication without medical direction for: fever persisting longer than 3 d, fever over 39.5° C (103° F), or recurrent fever, Do not give children more than 5 doses in 24 h unless Treatment of mild to moderate pain, moderate to severe pain with opioid analgesics, fever prescribed by physician, Do not breast feed while taking this drug without consulting physician. By mouth or IV Vancomycin antibiotics 1 gram every 12 hours time 4 O: rapid P: end of infusion D: 12-24 hr S: CV: Hypotension. Derm: rash. EENT: ototoxicity. GI: N/V. GU: nephrotoxicity. Hemat: leukopenia, eosinophilia. Local: phlebitis. Hypersensitivity reactions I: May cause additive ototoxicity and nephrotoxicity with others. C: hypersensitivity, Renal impairment, hearing impairment, intestinal obstruction or inflammation I: Orally administered for c.diff or staphylococcal enterocolitis. T: oral admin to take as directed. Take missed dose asap, do not double. Report signs of hypersensitivity, tinnitus, vertigo, or hearing loss. Advise if no improvement in a few days. Treatment of potentially life-threatening infections when less toxic antiinfectives are contraindicated