Biochemistry Lecture Notes: Bioenergetics, Gluconeogenesis, Glycogen
advertisement

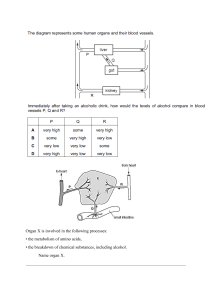
Maria Lopez Barazarte MD2 Block 2: Quiz 2 biochem notes Lecture 7: Bioenergetics 2 - Cytochrome c: cytochrome c is the only one not fixed to the imm. Is the bridged bt complex 3 and 4 - Complex 2 is the only one that does not pump hydrogens - this complex bypasses complex 1 - Need succinate → fumarate (from TCA) for complex 2 (succinate bypasses complex 1, electrons directly to CoQ) - NADH for complex 1 of ETC ( produced from the oxidation of glycolysis, FA oxidation, ketones metabolism, and TCA) - Vitamin B2 (riboflavin) constituent of FMN and FAD is needed for complex 1 and 2 - Vitamin B3 (niacin) a precursor of NAD+ complex 1 - Copper required for cytochromes a and a3 in complex 4 - Iron required for cytochromes and Fe-S centers - Sulfur required for Fe-s centers - Complex 1 inhibitors: rotenone (pesticides, fish poisoning), barbiturates (amytal, hypnopic) Complex 2 inhibitors: malonate Complex 3 inhibitors: antimycin Complex 4 inhibitors (cytochrome a,a3): cyanide (byproduct of nitroprusside), CO Complex 5 / atp synthase (ATP production): oligomycin ADP/ATP translocase: atractyloside (herbicide) Maria Lopez Barazarte MD2 Thermogenin is a proton channel present in uncoupler humans, allowing protons reentering to MM from IMS independent of ATP synthase. Is found in brown fat of newborns to generate heat Recall that ATP synthase takes all those protons and pumps them back in - mtDNA (from mom) is 10 times more susceptible to mutations than nuclear DNA Mitochondrial encephalopathies affect the tissues with high rate of oxidative phosphorylation (muscle - skeletal and cardiac, brain, eyes, liver, kidneys) Mitochondrial myopathies are tissue specific, some affect heart other muscle, major symptom is lactic acidosis Leber’s hereditary optic neuropathy (LHON): sudden onset of blindness (15-35 y/o) degeneration of optic nerve Disorders hints in vignette: - MELAS: lactic acid accumulation, incoordination, muscle weakness, seizures Maria Lopez Barazarte MD2 Lecture 8: Gluconeogenesis: synthesis of glucose from non carb Main precursors: lactate, pyruvate, glycerol and glucogenic AA such as alanine - PHD for insulin world - Pyruvate carboxylase for glucagon world DOES NOT OCCUR IN SKELETAL MUSCLE BECAUSE OF LACK OF G6P DOES NOT OCCUR IN HEART MUSCLE BECAUSE OF DEF PF F1,6BP CORI cycle links anaerobic glycolysis and exercising muscles to gluconeogenesis in the liver → prevents lactate accumulation Lactate is picked up by the liver. Muscle fatigue is caused by accumulation of lactate - Pyruvate carboxylase (PC)needs biotin as a cofactor in the reaction of pyruvate to OAA OAA is transported through the malate shuttle because is polar and cant pass Maria Lopez Barazarte MD2 - ATP is needed as a cofactor for PEPCK to convert OAA to PEP GLU-6-P only in the liver and kidney. NO MUSCLE. Required for glycogenolysis and gluconeogenesis CLINICAL CORRELATES 1. Pyruvate carboxylase deficiency: Fast state. accumulation of pyruvate, severe lactic acidosis because of increase in lactic acid, fasting hypoglycemia. LAB: increase blood lactate, increase blood pyruvate. In urine, high alanine, citrulline and lysine. Hyperammonemia (decreased urea cycle), and ketonemia - Most individuals present failure to thrive, developmental delay, recurrent seizures, hypotonia, intellectual disability, metabolic acidosis - RX: high carb, high protein diet to prevent gluconeogenesis. Avoid fasting and keto diet - Biotin deficiency 2. Pyruvate dehydrogenase deficiency: fed state. blood lactate, pyruvate, and alanine are elevated. Glucose is normal. Low atp levels _ low citrate. No ketone bodies detected. - Rx: low carb diet, high fat keto diet 3. Biotinidase deficiency: not able to recycle biotin. Which is a cofactor for PC. acidosis (mild), rashes (dermatitis), brittle hair, hair loss. RX: biotin replacement 4. PEPCK deficiency: defective gluconeogenesis, hypoglycemia, failure to thrive, loss muscle tone, hepatomegaly 5. Von Giere disease (type 1 glycogen storage disease): mutation on G-6-P 6. Fructose 1,6 biphosphate deficiency: lactic acidosis and hypoglycemia - When energy charge of the cells is low, glycolysis is favored, and gluconeogenesis is inhibited and vice versa - Fructose 2,6 bisphosphate is the most important allosteric modulator of glycolysis and gluconeogenesis Alcohol metabolism - 3 routes ** most important route: Ethanol --(ADH)--> acetaldehyde --(ALDH)--> acetic acid - Acetaldehyde is toxic → causes nausea and vomiting - NAD+ is a cofactor for both ADH and ALDH → gets reduced to NADHH+ (leading to high levels of NADH++) - Acetate generated enters the blood - Ethanol and methanol are competitive inhibitors Maria Lopez Barazarte MD2 - Fomepizole inhibits ADH Disulfiram inhibits ALDH - prescribed for recovering alcoholics. Inactive ALDH causes dislike for alcoholic beverages - Alcohol consumption can cause hypoglycemia. High NADH++ generated favors other conversions (pyruvate to lactate → lactic acidosis, OAA to malate → decreases OAA to gluconeogenesis). - Fatty liver due to accumulation of NADHH+ and glycerol 3P + excessive acetic acid - ****Hypoglycemia, lactic acidosis, hyperlipidemia and ketoacidosis are common findings in alcoholics - Alcohol inhibits active transport of thiamin → thiamine def in alcoholics (Wernicke korsakoff syndrome). Confusion, ophthalmoplegia, ataxia. Hints from questions: - Depletion of Hepatic glycogen stores → lactate would be present - Low carb, high fat diet, how do we produce glucose? - using glycerol Kinases are activated by dephosphorylation Lecture 9: Glycogen is stored in cytosol granules of: 1. Liver: maintain the normal blood glucose concentrations 2. Muscle: do not contain G-6-pase. G6P stays inside the muscle cells a a local source of energy during muscle contraction. Do not use for maintain the normal blood glucose concentration Trapping and activation of glucose: - Glucose transformed to G6P by hexokinase / glucokinase → from glycolysis - glucokinase/hexokinase reaction (traps glucose as G6P inside of the cells). - phosphoglucomutase (PGM) reversibly isomerizes G6P to G1P. - UDP-glucose pyrophosphorylase transfers G1P to UTP, which generates UDP-glucose (the active form of glucose) - UDP GLUCOSE IS THE IMMEDIATE PRECURSOR FOR GLYCOGEN SYNTHESIS, PROTEOGLYCANS/ GLYCOLIPIDS/ GLYCOPROTEINS Maria Lopez Barazarte MD2 For the formation of the linear structure of glycogen - Glycogen synthase the rate limiting enzyme transfer/attaches glucose from UDP-glucose onto the non reducing end of the primer by formation of alpha 1-->4 glycosidic bond making a linear polyglucose chain called amylopectin. CAN ONLY USE UDP GLUCOSE FOR THE CHAIN For the branching - RXN: amylo-(1,4 → 1.6) transglycosylase/ glucosyl. Enzyme: 4:6 transferase. Alpha 1.6 linkages make the branches For degradation - Glycogen attacked by debrancer enzyme → releases a little bit of glucose → attacked by glycogen phosphorylase and Pi→ changed to Glucose 1-P→ phosphoglucomutase transforms it to glucose 6-P → G-6-Pase (ONLY LIVER) transforms it to glucose - Chain shortening by release of G1P - Glycogen phosphorylase uses inorganic phosphate (Pi) to attack nonreducing ends Debranching enzyme - Transferase domain: transfer residues from outer branch to another - ******Alpha 1,6 glucosidase domain (hydrolase activity): cleaves alpha 1-->6 glycosidic bond and release free glucose - The small amount of glycogen is degraded by lysosomes by acid maltase / lysosomal a-glucosidase (hydrolyzes both a-1,4 and a1,6) to get glucose Maria Lopez Barazarte MD2 The control of glycogen metabolism is needed to maintain physiological blood glucose level and provide energy for exercising muscles - FED/ glycolysis: glycogen synthase is ON (because we want to make reserves) - FAST/ glycogenolysis: glycogen phosphorylase is ON (because we need some source of energy - from storage / reserve) to feed the muscle. - GLYCOGENOLYSIS BY EPINEPHRINE AS IN ACUTE STRESS OR EXERSICES (muscle does not have receptors for glucagon). CLINICAL CORRELATION - glycogen storage diseases (GSD) 1. GSD type 0: Glycogen synthase deficiency. This enzyme uses UDP to make the alpha 1→ 4 bonds. So no storage of glycogen because there is no chain elongation. In the liver, there is hyperglycemia after meals, and in the muscle there is fatigue and muscle cramps. 2. GSD Type I: Von Gierke disease: Glucose-6-Pase. Problems in dephosphorylation of Glc-6-P to Glucose. - Hepatic form. Hypoglycemia. Hepatomegaly. Person does not respond to epinephrine or fructose. Slightly acidic blood pH, elevated ketones, triglycerides, cholesterol, and liver enzymes. DOLL LIKE FACE. Normal structure glycogen is biopsy. - Avoid fasting, high carb diet 3. GSD Type II; Pompe disease: lysosomal a glucosidase / acid maltase defective. Problems in lysosomal attack to release glucose. - Progressive muscle weakness, congestive heartfailure and enlarged heart. No rolling, baby is flaccid, flops back when lifted - FLOPPY BABY. increase glycogen stores in lysosomes. Normal lactate (no acidosis), no hypoglycemis, increase CK, AST, LDH 4. GSD type III: Cori disease. Defective debranching enzyme (amylo 1,6 glycosidase) - Irritability, failure to thrive. Mild fasting hypoglycemia. High protein diet or fructose increases glucose concentration. Hepatomegaly Biopsy shows increased amount Maria Lopez Barazarte MD2 5. 6. 7. 8. of glycogen with short outer branches. - increased abnormal glycogen with many branch points GSD type IV: Andersen disease: branching enzyme deficiency (amylo 4,6 glucosidase). Abnormal glycogen with few branches in the liver. Long linear glycogen without or few branches, amylopectin. - Hepatomegaly, cirrhosis, cardiomyopathy, begin the first months of life. Liver becomes cirrhotic. GSD Type V: McArdle disease. Defective glycogen phosphorylase. Problems with Glc 1-P release. - Myopathy. Increased fatigue and muscle pain in legs after exercise. lactate concentration remains decreased/ same in blood after exercise. Accumulation of normal glycogen in muscle tissue. Normal blood glucose. Burgundy colored urine after exercise. - Rx: admi of glucose before exercise GSD type VI: Hers disease. Glycogen liver phosphorylase is defective. Problems with Glc 1-P release in liver - Hepatomegaly, hypoglycemia, symptoms present at young age, nomral lactic an uric acid GSD Type VII: Tauri disease. Mutation in muscle PFK-1. - Myopathy. Severe exercise intolerance, trouble with anaerobic activities, lack of lactate production, hemolytic anemia. Defective isoenzyme M in PFK-1 in muscle. Normal blood glucose. Hepatic forms: 1,3,4,6 - hepatomegaly, hypoglycemia, lactic acidosis, hyperuricemia, hyperlipidemia Myopathic forms: 5 and 7 - muscle cramps, pain, fatigue upon exertion Lysosomal: 2 - POMPE all organs involved, specially myocardium, skeletal muscle, liver, motor nuclei of spinal cord Hyperuricemia is caused by lactate inhibition of kidney tubule excretion or urate