Review
1.
Introduction
2.
The circadian clock and its
regulators in humans
3.
Evidence for circadian
dysregulation in BD
4.
Lessons from existing circadian
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
rhythm-related treatments
5.
Conclusion
6.
Expert opinion
Sleep- and circadian
rhythm--associated pathways
as therapeutic targets
in bipolar disorder
Frank Bellivier†, Pierre-Alexis Geoffroy, Bruno Etain & Jan Scott
†
Groupe Hospitalier Saint-Louis-Lariboisie`re-Fernand Widal, Department of Psychiatry, Paris
Cedex, France
Introduction: Disruptions in sleep and circadian rhythms are observed in
individuals with bipolar disorders (BD), both during acute mood episodes
and remission. Such abnormalities may relate to dysfunction of the molecular
circadian clock and could offer a target for new drugs.
Areas covered: This review focuses on clinical, actigraphic, biochemical and
genetic biomarkers of BDs, as well as animal and cellular models, and highlights that sleep and circadian rhythm disturbances are closely linked to the
susceptibility to BDs and vulnerability to mood relapses. As lithium is likely to
act as a synchronizer and stabilizer of circadian rhythms, we will review pharmacogenetic studies testing circadian gene polymorphisms and prophylactic
response to lithium. Interventions such as sleep deprivation, light therapy
and psychological therapies may also target sleep and circadian disruptions
in BDs efficiently for treatment and prevention of bipolar depression.
Expert opinion: We suggest that future research should clarify the associations between sleep and circadian rhythm disturbances and alterations of
the molecular clock in order to identify critical targets within the circadian
pathway. The investigation of such targets using human cellular models or
animal models combined with ‘omics’ approaches are crucial steps for new
drug development.
Keywords: bipolar disorders, circadian rhythm, sleep, therapeutic response
Expert Opin. Ther. Targets [Early Online]
1.
Introduction
The recognition of abnormal sleep and circadian rhythms as core symptoms of
bipolar disorder (BD) led to the development of important research efforts to
characterize these features [1]. It has also stimulated the development of new pharmacological and nonpharmacological treatments. Abnormal sleep and circadian
rhythms are found in individuals at high risk of developing BD and are observed in
euthymic, prodromal and syndromal periods [2]. The role of sleep disturbances as
disease course modifiers is also well established, mainly due to their association
with treatment-refractory or prolonged mood phases and as predictors of early
relapse [3-5].
Taken together, these data suggest that the exploration of sleep and circadian
rhythms, and their modification by psychological and pharmacological interventions alongside the study of putative associated biomarkers in the blood or in the
brain could facilitate the development of novel therapeutic targets.
In this review, we summarize data obtained from remitted bipolar cases (i.e., in
euthymic periods). We first review the molecular functioning of the circadian clock.
Then we present data demonstrating disruptions of sleep and circadian rhythms in
10.1517/14728222.2015.1018822 © 2015 Informa UK, Ltd. ISSN 1472-8222, e-ISSN 1744-7631
All rights reserved: reproduction in whole or in part not permitted
1
F. Bellivier et al.
Article highlights.
.
.
.
.
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
.
Disruptions in sleep and circadian rhythms are part of
the pathophysiology of bipolar disorders.
Preliminary studies suggested that genetic variants in
circadian genes were associated with bipolar disorders
but also with lithium response.
Cellular and animal models have also been used with
some promising results to identify circadian pathways as
potential targets for mood stabilizers, mainly lithium.
There is an urgent need to combine clinical, biochemical
and global ‘omics’ approaches to disentangle the
potential circadian targets for existing drugs but also to
validate models to be used in the screening of new
compounds.
Targeting sleep and circadian rhythms related pathways
may be an important avenue for developing new
mood-stabilizing agents.
This box summarizes key points contained in the article.
BD at phenotypic, biochemical (melatonin and cortisol) and
genetic levels. Lastly, new avenues for the development of
new drugs targets are presented.
The circadian clock and its regulators in
humans
2.
A circadian rhythm is any biological process that displays an
endogenous, entrainable oscillation of about 24 h. A circadian
clock drives these rhythms, which have been widely observed
in plants, animals, fungi and cyanobacteria. Biological
temporal rhythms include daily, tidal, weekly, seasonal and
annual rhythms. Although circadian rhythms are endogenous
(biologically determined; ‘built-in’; self-sustained), they are
adjusted to the local environment by external cues called zeitgebers, commonly the most important of which is daylight [6].
Circadian rhythmicity is present in the sleeping and feeding
patterns, core body temperature, brain wave activity, hormone production, cell regeneration and several biological
activities [7]. The main brain structures controlling circadian
rhythms are the suprachiasmatic nuclei (SCN) located in the
hypothalamus and the pineal gland.
The molecular circadian clock
The SCN, located in the anterior hypothalamus, host ‘the
master circadian pacemaker.’ The pacemaker comprises a
complex network of transcriptional--translational feedback
loops that result in the rhythmic expression of clock genes
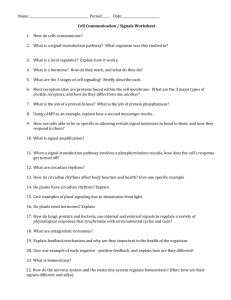
(with a periodicity of just over 24 h) [7]. The main players in
these feedback loops are circadian locomotor output cycles
kaput (CLOCK), BMAL1, period homolog (PER), CRY,
REV-ERBa (or nuclear receptor subfamily1, groupe D, member1 [orphan nuclear receptor REV-ERBa] [NR1D1]), timeless homolog (TIMELESS) and retinoid-related orphan
receptor A (RORA) proteins (Figure 1). Another regulatory
loop involves TIMELESS, PER, CLOCK and BMAL1 [8].
2.1
2
Glycogen synthase kinase 3b (GSK3b) (a well-known site of
action of lithium) is involved in the regulation of the circadian
clock as it phosphorylates CRY, BMAL1, PER2, CLOCK,
TIMELESS and REV-ERB [9-11]. The molecular structure of
the circadian clock is highly conserved throughout the evolution of species, suggesting that circadian rhythms are mainly
biologically determined (genetic aspects are discussed further
in a later section) [12]. In humans, it is well established that circadian rhythms are also influenced by environmental factors
such as light, external temperature, social activities, seasonal
variations and psychological factors. The day--night cycle is
the main environmental driver that synchronizes the circadian
‘clock’ with environmental time signals [7]. This synchronization process involves retinal ganglion and retinohypothalamic
tracts that converge to the SCN.
The SCN oscillation controls the rhythmic expression of
clock-controlled genes, which are widely distributed among
all peripheral tissues such as liver, endocrine tissues, heart,
skeletal muscles, and so on [13,14]. The rhythmic expression
of these genes controls rhythmic functions including the
sleep--wake cycle, feeding behavior, core body temperature,
release of hormones, and metabolic regulation [7,15].
Variations in the gene sequence or in the expression profile
of the circadian genes observed in bipolar individuals are
further described in the ‘genetic’ section of this review (see
Section 3.3).
The melatoninergic system
The pineal gland is another important element of the circadian system and is the brain structure where melatonin is synthesized. The dark--light cycle regulates melatonin secretion
via the SCN. Melatonin secretion is high during the periods
of darkness, whereas light inhibits its secretion [16,17]. Seasons
of the year also regulate melatonin secretion due to changes in
the number of daylight hours. Melatonin is a useful marker of
circadian regulation and activity and it can be assayed in
blood, saliva and urine. The most valid circadian melatonin
phase marker is the dim light melatonin onset (DLMO)
[18,19]. Blood melatonin concentration increases before
bedtime, remains high during nocturnal sleep and decreases
rapidly after light exposure (in particular, sunlight and blue
wavelength). Body temperature and cortisol concentrations
follow inverse circadian variations [20].
2.2
Circadian systems and neurotransmitters that
regulate mood
2.3
Circadian rhythms influence serotonergic [21-23], dopaminergic [24-27] and noradrenergic [28,29] neurotransmissions.
Serotonin (5HT) signaling via efferent pathways from
median raphe nuclei to SCN increases the regularity of circadian rhythms [30-32]. These serotonergic projections represent
the anatomical interface between circadian functions and
mood regulation [33]. 5HT regulates the SCN activity by
photic [34-36] and nonphotic factors [32,37]. Moreover,
Expert Opin. Ther. Targets (2015) 19(6)
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
Nucleus
RORs
Ccg
RRE
Per1/Per2
RRE
Cry1/Cry2
RRE
REV-ERBa
REV-ERBs
RRE
Bmal1
Bmal1
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
RRE
CLOCK
RRE
RORa
REV-ERBs
CRYs
PERs
CK1ε/δ
RORs
Cytoplasm
Figure 1. Molecular circadian clock. Black arrow: relocation, Green arrow: stimulation, Red arrow: inhibition.
bmal1: Brain and muscle ARNT like 1 orphan nuclear receptor REV-ERBa; Ccg: Clock-controlled gene; CLOCK: Circadian locomotor output cycles kaput;
CRY: Cryptochrome; PER: Period homolog; ROR: Retinoid-related orphan receptor.
serotonergic activity is influenced by light exposure and time
of year [38]. Interestingly, in Drosophila, serotonergic signaling increases the phosphorylation of SHAGGY (homolog of
human GSK3b) and light-induced degradation of TIMELESS [39]. In the pineal gland, melatonin is synthesized from
5HT and the SCN modulates the catabolism of 5HT into
melatonin [40].
In the retina, dopamine (DA) plays an important role in the
adaptation to light [41]. Moreover, in the tegmental ventral area
and substantia nigra, DA signaling is a key component of the
sleep/wake cycle and rapid eye movement (REM) sleep [42,43].
In the SCN, the activity of the CLOCK--BMAL1 complex is
regulated by dopaminergic D2 receptors [44]. Finally, noradrenalin regulates the melatonin synthesis in the pineal gland [45].
In summary, disruption of circadian rhythms and abnormal emotional regulation are core features of BD that may
result from complex interactions between serotonergic and
dopaminergic systems and the circadian clock [46].
3.
Evidence for circadian dysregulation in BD
Phenotypic characteristics
Individuals with BD demonstrate abnormal chronobiological
rhythms that affect mainly sleep homeostasis and circadian
3.1
rhythms. Disrupted circadian rhythms are observed in individuals who later develop BD, even before disease onset, and
in BD cases during acute episodes and during inter-episode
periods [47] (see the following sections and Table 1).
Chronotypes
The term chronotype refers to the attributes of individuals
that reflect the time of the day that their physical functions
(hormone level, body temperature, cognitive faculties, eating
and sleeping) are active, change or reach a certain level. However, this term is often used in research to describe a person’s
preference for daytime versus nighttime activities. The
€
Horne--Ostberg
morningness--eveningness questionnaire [48],
the Composite Scale of Morningness [49] and the Munich
ChronoType Questionnaire [50] are the most frequently used
tools to categorize individuals as ‘morning types’ or ‘evening
types.’ Studies using such measures demonstrate that, in the
general population, diurnal preference (i.e., morningness-eveningness) is a heritable trait [51-55] and is strongly associated
with other endogenous phase markers, such as circadian shifts
in body temperature [56,57], salivary melatonin secretion [58]
and the cortisol awakening response [59]. In a given subject,
morningness--eveningness preference is relatively stable over
3.1.1
Expert Opin. Ther. Targets (2015) 19(6)
3
F. Bellivier et al.
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
Table 1. Circadian phenotypes as potential trait markers of bipolar disorders.
Circadian parameter
Association with
bipolar disorders
Presence
during remission
Heritability
Over-represented
among high-risk subjects
for bipolar disorders
Lifestyle irregularity
Evening type
Higher sleep--wake cycle variability
Higher cortisol secretion
Supersensitivity of nocturnal plasma
melatonin in response to light
Lower overnight serum melatonin
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
?
Yes
Yes
Yes (awaking)
Yes
Yes
?
Yes
Yes (afternoon)
Yes
Yes
Yes
Yes
?
time, as confirmed in studies of various populations with
different cultural habits [60,61].
Several studies of individuals with BD demonstrate a
significantly higher prevalence of ‘evening chronotypes’ than
reported in healthy controls [62-66] or cases of recurrent major
depressive disorder [67]. In individuals with BD, eveningness is
also associated with earlier age of onset, a rapid-cycling course,
and other factors such as a reduction in the peak of the melatonin secretion at night [64]. Furthermore, population-based
studies demonstrate that eveningness is more common in
cyclothymic individuals (especially those with at least one
prior episode of depression), and some, but not all, studies
of temperaments that are putatively linked to risk of BD
(such as hyperthymia) show a higher prevalence of this chronotype in the at-risk populations [68]. In summary, although
possible confounders were not always taken into account in
these studies, this heritable trait (vesperal preference) commonly co-occurs with BD and may be associated with some
risk syndromes, early illness onset and course characteristics.
Sleep--wake cycles
Polysomnography (PSG) and actigraphy are the main tools
used to assess sleep--wake cycles and studies suggest that BD
cases differ in several important aspects from healthy
controls [69]. For example, higher-density REM sleep during
the first REM period, more frequent nocturnal arousals and
higher sensitivity to the cholinergic receptor agonist were
observed on PSG recordings of remitted bipolar cases compared with healthy controls [70,71]. Several actimetry studies
show that euthymic BD cases have a greater variability in their
sleep/wake patterns and poorer sleep quality than individuals
with insomnia or controls [72-80]. Interestingly, a recent
meta-analysis of actigraphy studies in remitted BD cases confirmed significant differences on several sleep parameters
compared to healthy controls: longer sleep latency, longer
sleep duration, more wake after sleep onset and poorer sleep
efficiency [81]. Furthermore, small-scale studies of actigraphy
and DLMO identify that delayed sleep phase -- the most
common circadian disorder, especially in adolescents -- is
3.1.2
4
even more prevalent in young people with emerging mood
disorders compared to their peers, being twice as common in
unipolar depression compared to healthy controls (14 vs 7%)
and four times more common in young adults with recent
onset BD [82]. Other small-scale studies of individuals at
high risk for BD suggest that they exhibit greater variability
in sleep duration, fragmentation and efficiency, as well as
shorter sleep duration, later and more variable bedtimes, and
lower relative amplitude of activity patterns than control subjects [80,83]. Twin- and family-based studies show that sleep
length is heritable and the genetic contribution to the variance
was 33% for sleep quality and to sleep disturbance was 40%
for sleep pattern [84,85].
Although actigraphy studies have mainly focused on sleep
profiling, in recent years, there has been an increasing interest
in using the data to assess daytime activity. Such studies reveal
that the daily activity of euthymic BD cases is significantly
lower than other mental health service users or control participants [86]. In addition, investigations of lifestyle regularity
indicate that diurnal preference and regularity of sleep and
social rhythms are highly interconnected [87,88]. While BD
cases may demonstrate disrupted social rhythms as a consequence of the illness, it has also been demonstrated that individuals at risk of BD or with subsyndromal presentations
exhibit less regularity of lifestyle than healthy controls even
before the disorder is fully manifested [89-91]. The most prominent abnormalities are lower regularity of daily activities and
more variation in sleep duration [72,92]. In euthymic BD, activity level predicts the onset of major depressive, hypomanic and
manic episodes during the following 3 years [92]. These findings are also consistent with the idea that individuals with
BD or BD spectrum are more sensitive to environmental clues
that precipitate or contribute to mood, sleep and activity disruptions, which are the commonest prodromal symptoms of
further episodes [93]. Finally, several studies investigated differences between bipolar I and II and failed to show any difference [62,65,67]. Studies using actigraphy have included only
type I (or very limited number of bipolar type II) [81].
Expert Opin. Ther. Targets (2015) 19(6)
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
Table 2. Association studies between circadian genes and bipolar disorders.
Gene
Online Mendelian inheritance in man (OMIM) nomenclature
Ref.
CLOCK
NPAS2
ARNTL1 (or BMAL1)
Circadian locomotor output cycles kaput
Neuronal PAS domain protein 2
Aryl hydrocarbon receptor nuclear translocator-like 1
(or brain and muscle ARNT like 1)
Periodhomolog 1
Periodhomolog 2
Periodhomolog 3
Cryptochrome 1
Cryptochrome 2
Timeless homolog
Nuclear receptor subfamily 1, group D, member 1
(or orphan nuclear receptor REV-ERBa)
Retinoid-related orphan receptor A
Retinoid-related orphan receptor B
Casein kinase 1 d
Casein kinase 1 e
Glycogen synthase kinase 3 b
Basic helix-loop-helix domain containing, class B, 2
Acetyl serotonin methyl transferase
Aryl alkylamine N-acetyl transferase
[131,133-136]
[135]
[117]
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
PER1
PER2
PER3
CRY1
CRY2
TIMELESS
NR1D1 (or REV-ERBa)
RORA
RORB
CSNK1d
CSNK1e
GSK3b
BHLHB2
ASMT
AANAT
Biochemical phenotypes
The secretion of cortisol and melatonin shows a circadian
pattern. Biochemical studies have investigated their secretion
in plasma, serum or saliva.
3.2
Hypothalamic--pituitary--adrenal axis: cortisol
In healthy individuals, cortisol secretion has a morning peak
with a 24-h cycle. In a given individual (from the general
population), the cortisol awakening response is highly regular
across extended periods [94]. The 24-h cortisol secretion is
significantly higher in patients with BD than in controls,
irrespective of the phase of BD (manic, depressive or euthymic) [95]. This is consistent with the observation of glucocorticoid receptor mRNA in the hippocampi and amygdala nuclei
in patients with BD by comparison with healthy controls [96].
Cortisol secretion, in particular cortisol awakening response, is
a heritable trait and the heritability of cortisol secretion has
been estimated to be 62% [97-99]. However, investigations of
cortisol secretion in high-risk individuals have produced conflicting results [100-102]. In addition, increased cortisol secretion
is not very specific to BD (also encountered in unipolar
depression, psychotic disorders as well as eating disorders), as
confirmed in a recent meta-analysis [103].
3.2.1
Pineal function: melatonin
Hypersensitivity to light has been proposed as a trait marker
of mood disorders including seasonal affective disorders and
BD [104,105], although some publications do not support this
conclusion [106,107]. However, studies focusing on nocturnal
melatonin secretion report lower levels of secretion in BD
cases compared with controls [108,109] and indicate the
3.2.2
[135]
[135,188]
[117,131,135]
[147]
[134,135,137]
[132,134,135,148,197]
[132,146-148,197]
[127,128,137]
[127,128]
[135]
[118,134,135]
[144,145,148]
[140]
[138,139]
[138]
existence of abnormal amplitude and periodicity of melatonin
secretion [47]. Some researchers suggest that findings of
reduced nocturnal melatonin levels in BD that occurred
independent of current mood state suggest that this may be
a trait rather than a state marker of BD [109]. In contrast, daytime melatonin levels appear to be elevated in manic patients
compared to controls [110]. Recently, Robillard et al. used
saliva samples and demonstrated that compared to unipolar
patients, bipolar patients had later DLMO and smaller
melatonin AUC than the unipolar group [111].
Interestingly, monozygotic and dizygotic twin studies show
a genetic component to nocturnal melatonin secretion and
sensitivity to light [112]. Furthermore, supersensitivity in the
melatonin response to light exposure has been shown in individuals at high risk of BD [113]. However, no differences in
total pineal volume have been observed between BD cases
and healthy controls [114].
Genetic studies
Circadian genes may increase vulnerability to several psychiatric disorders [115]. In particular, genomic and post-genomic
studies may help to identify pathways implicated in vulnerability to BD as well as in treatment response. Some circadian
genes as well as genes encoding proteins involved in related
pathways are strong candidate genes in BD. In this section,
we review genetic and pharmacogenetic studies that have
investigated some circadian genes.
3.3
Genetic association studies and candidate gene
approach
3.3.1
Findings regarding circadian gene polymorphisms and vulnerability to BD are summarized in Table 2. The most replicated
Expert Opin. Ther. Targets (2015) 19(6)
5
F. Bellivier et al.
findings involve the CLOCK, NPAS2, aryl hydrocarbon receptor nuclear translocator-like 1 (or brain and muscle ARNT
like 1) (ARNTL1), NR1D1, PER3, related orphan receptor B
(RORB) and CSNKe genes. Although GSK3b is often
regarded as a strong candidate gene, no association with
GSK3b gene polymorphism has been reported [116-118]. However, the frequency of a copy number variant in the GSK3b
locus has been shown to be higher in BD cases compared
with controls [119].
Human cell cultures
Cell cultures derived from human skin biopsies, blood samples [120] or hair follicle cells [121] have been used in laboratory
experiments. Cultures of human fibroblasts have been used to
examine circadian functions, including the amplitude- and
phase-resetting responses, and these have been found to be
correlated with the chronotype of the individual from whom
the cells were derived [122]. Using a transcriptomic approach,
Yang et al. demonstrated that the amplitude of rhythmic
expression of BMAL1, REV-ERBa and D site of albumin promoter (DBP) was lower in fibroblasts derived from BD cases
than controls [123]. In this study, the overall mRNA expression
levels for DEC2 and DBP were reduced in biological material
drawn from BD cases. Posttranslational modifications were
also observed with reduced level of GSK3b phosphorylation
in BD individuals.
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
3.3.2
Animal studies
The role of circadian genes in modulating behavior has also
been highlighted in genetically manipulated animals. In
mice, the deletion of exon 19 in the CLOCK gene is associated
with manic-like hyperactivity, craving for rewarding stimuli
(similar to BD cases in a manic state), less depression-like
behavior, lower anxiety levels and abnormal sleep/wake
cycles [124]. The manic-like behavior of the Clock mutant
mice can be reversed by lithium treatment or the restoration
of a functional CLOCK gene in the ventral tegmental
area [125]. Other examples of mouse models involving circadian genes include transgenic mice overexpressing GSK3b,
which show a manic-like phenotype [126].
In summary, the results of studies using different experimental design, in different species, can be difficult to interpret.
Convergent functional genomic approaches are particularly
useful to integrate data from classical genetic studies, gene
expression studies in human cell cultures or in animals and
postmortem human brain studies. Studies applying convergent functional genomics suggest that ARNTL1, GSK3b,
RORA and RORB are the top candidate circadian genes for
BD [127,128].
3.3.3
Disrupted circadian rhythms in BD and circadian
genes
3.3.4
PER3, REV-ERBa and GSK3b genes have been associated
with an early age of BD onset [129-133]. This is consistent
with the observation that early age at onset is associated with
6
more severe circadian disruptions (eveningness and sleep quality). Other circadian genes are associated with rapid cycling of
BD and/or with a high recurrence of illness: CRY2, CLOCK,
ARNTL2, TIMELESS and CSNK1e [134,135]. These findings
suggest that variations in some circadian genes may explain
the high sensitivity to rhythm changes observed in BD, and
may be associated with disease onset or relapses.
Two studies have examined the relationship between circadian gene variants and chronotypes in patients with BD: in a
Korean sample, the CLOCK gene 3111T/C variant was associated with an extreme evening chronotype [135,136], and a
nonsynonymous coding single-nucleotide polymorphism
(SNP) in PER3 and two intronic SNPs in CSNK1e were
associated with eveningness [118].
Behavioral consequences of at-risk variants have been
studied using phenotypic subjective and objective biomarkers
such as chronotypes, circadian types or sleep--wake patterns.
Using a ‘reverse phenotyping approach’ to look for association
between at-risk polymorphisms and circadian phenotypes, it
has been observed that TIMELESS (rs774045) was associated
with eveningness and languid (i.e., lacking energy in the
morning) circadian type, whereas RORA (rs782931) was associated with rigid (i.e., less flexible) circadian type in euthymic
cases compared to controls [137]. Actigraphy has been used to
explore carriers of the at-risk allele associated with BD of a
common polymorphism (rs4446909) of the promoter of the
acetylserotonin O-methyltransferase gene, encoding one of
the two enzymes involved in melatonin biosynthesis [138].
Interestingly, the GG at-risk genotype was associated with
longer sleep duration, greater activity in active periods of sleep,
and greater interday stability [139]. A further recent study
examining circadian polymorphisms observed that delayed
sleep and eveningness were inversely associated with NFIL3
(rs2482705) and RORC (rs3828057), and that a group of
haplotypes overlapping BHLHE40 was associated with non24-h sleep--wake cycles, with delayed sleep and with BD
(rs34883305, rs34870629, rs74439275 and rs3750275) [140].
These preliminary studies highlight that variants of circadian genes that may increase susceptibility to BD also influence circadian phenotypes, and thus may point to future
treatments after further replication and identification of the
causal polymorphisms.
Pharmacogenetic studies
Most of the pharmacogenetic studies that have tested circadian genes have explored lithium response [141]. Although
the mechanism of action of lithium is unknown, it has been
found that lithium influences the expression of circadian
genes and so it is possible that this pathway is involved in
the therapeutic effects of this mood stabilizer [142].
GSK3a and GSK3b are inhibited by lithium. Lithium acts
on these enzymes either by direct inhibition or indirectly via
other mechanisms such as the formation of a signaling
complex involving b-arrestin 2 and Akt [143]. Genes coding
these enzymes are obvious candidates for modulating lithium
3.4
Expert Opin. Ther. Targets (2015) 19(6)
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
therapeutic response. An association of GSK3b (-50 T/C)
polymorphism with the therapeutic response to lithium
among 88 BD-I cases was recently reported: the relapse risk
(measured by the recurrence index) for homozygotes for the
wild variant (C/C) did not change under treatment, whereas
carriers of the mutant T allele showed improvement, suggesting that the GSK3b-50 T/C polymorphism may influence
prophylactic response to lithium in BD [129]. However, this
result has not been replicated in subsequent studies [144,145].
GSK3b also phosphorylates and stabilizes REV-ERBa, one
of the main components of the circadian rhythm system that is
involved in the cyclic regulation of BMAL1. Lithium reduces
REV-ERBa and BMAL1 gene expression, implicating REVERBa as a target of lithium in its mechanism of action [10].
The association between REV-ERBa gene (NR1D1) and
prophylactic response to lithium in BD has been investigated
in three studies. In a sample of 199 Sardinian BD patients
characterized for lithium, no association was found [146]. However, more recently, an association between the rs2314339
variant of the NR1D1 gene and lithium response was
reported. Furthermore, in a sample of 282 Caucasian bipolar
patients characterized for lithium response, an association
between the NR1D1 rs2071427 variant and response to
lithium was found [147]. The same study reported that a variant
in cryptochrome-1 (CRY1; rs8192440) was nominally
associated with the response to lithium. Finally, GSK3b and
NR1D1 genotypes considered together predicted the response
to lithium robustly and additively; the response was proportional to the number of response-associated alleles [148].
Glucocorticoid receptors are likely to regulate circadian
rhythms. A polymorphism of the glucocorticoid receptor
gene (NR3C1) on chromosome 5q31-32 is associated with
lithium responder status [149].
Lessons from existing circadian
rhythm-related treatments
4.
Chronotherapies
Chronotherapeutics are based on controlled exposure to environmental stimuli such as photic, sleep--wake cycle or lifestyle
regulation approaches that are purported to modify biological
rhythms.
Classical chronotherapeutic techniques include light
therapy, sleep phase advance, sleep deprivation therapy
(SDT), dark therapy and extended bed rest. Strong evidence
of efficacy has been demonstrated for SDT and sleep phase
advance disorders [150], with some evidence for light therapy
in patients with BD [151]. Some publications on BD depression indicate that sleep deprivation combined with antidepressants or mood stabilizers may lead to an earlier
response [152-154] and that light therapy may be used in the
treatment of BD depression [155,156]. Other studies suggest
that BD cases who receive medication (mood stabilizer and
antidepressant) in combination with three established
circadian-related treatments (sleep deprivation, bright light,
4.1
sleep phase advance) show an earlier and more sustained
decrease in depression scores than a medication-only
group [157]. There is also some research that indicates that
dark therapy [158,159] or the use of specific lenses that block
blue light [160] can reduce manic symptoms or rapid cycling.
The techniques identified are mainly adopted from sleep
research. However, two other streams of research have
recently been used in BD. First, cognitive behavior therapy
for insomnia (CBT-I) has now been applied to mood disorders [161]. The initial pilot studies of CBT-I for BD demonstrate a good effect in > 60% cases, and suggest that sleep
regulation techniques (especially regularizing bedtimes, etc.)
are the most beneficial. However, it was notable that a small
number of cases (where sleep deprivation was employed)
appeared to be destabilized and demonstrate an increase in
(hypo)manic symptoms [161]. Larger studies are now ongoing,
although there are suggestions that some circadian-based
abnormalities (such as delayed sleep phase) may prove lower
response than other sleep problems in BD [162].
The second source of evidence for psychological interventions modifying sleep in BD comes from studies of the therapies that were developed specifically for individuals with BD.
Although these interventions derive from several different
models, there are a number of shared elements that are common to all therapies, and all effective therapies incorporate
specific techniques aimed at enhancing social and circadian
rhythm stabilization [163]. The classic example of this
approach comes from interpersonal social rhythm therapy
(IPSRT) developed by E. Frank [164] and recently
reviewed [165]. The main difference between these BD-specific
approaches such as IPSRT and CBT-I is that the former
incorporates a number of interventions related to regulation
of daytime activity, reduction of stressors or overstimulation,
and more overtly try to identify and reduce the intake of
substances (caffeine, nicotine, alcohol, etc.) that disrupt
sleep--wake cycles, as well as regularizing sleep patterns.
However, as yet, there is no direct evidence that such changes
mediate change in mental state; indeed, in several studies, stabilizing social rhythms was not associated with improvement
in BD [163]. In addition, no biomarkers of response to any
type of chronotherapy have been identified so far.
Pharmacological treatments
Lithium and valproate may work in part via a chronobiological mechanism [166]. Lithium has phase-delaying properties
because it lengthens the circadian period in a variety of organisms, including humans [142,167]. The amplitude of PER2
protein cycling in the central and peripheral circadian clockwork is enhanced by lithium [168]. As noted previously,
chronic administration of lithium reverses the manic-like
phenotype of transgenic mice carrying a mutation in the Clock
gene [125]. We also previously described that GSK3b and
NR1D1 genes may modulate response to lithium. Low doses
of lithium carbonate and sodium valproate reduce melatonin
secretion in response to light in healthy volunteers, suggesting
4.2
Expert Opin. Ther. Targets (2015) 19(6)
7
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
F. Bellivier et al.
that lithium also acts on the melatonergic system [169,170].
Valproic acid also increases the amount of melatonin receptors in C6 glioma cells [171] and influences the expression of
several circadian genes in the amygdala [172].
Some pharmacological compounds directly act on the
circadian or melatonergic systems. These include melatonin
and melatonin receptor agonists that have the potential to
synchronize the sleep/wake cycle. The efficacy of these treatments is still to be fully established, but several reports suggest
that adjunctive melatonin can improve sleep quality [173-176].
These case reports describe patients in manic, depressive or
rapid-cycling phases of BD who are given the chronobiotic
medications in combination with other mood stabilizer and
treatment regimens [173-176].
Ramelteon is a melatonin receptor agonist that is used for
insomnia and for people who have difficulty falling asleep.
One study in euthymic patients with BD reported that ramelteon (24 weeks) contributes to relapse prevention by comparison with placebo in association with a mood stabilizer [177].
Agomelatin (a melatonin receptor agonist and a serotonin
5-HT2C receptor antagonist) synchronizes circadian rhythms
involving body temperature, cortisol and other hormones in
animal models and in humans [178]. Three studies have
reported the efficacy of agomelatin as an adjunctive treatment
in bipolar depression [179-181].
5.
Conclusion
Several core features of vulnerability to BD onset or to episode
recurrence in established cases of BD appear to indicate underlying abnormalities of the circadian and melatonergic systems.
As such, the further characterization of circadian-related dysregulations and of therapeutic response to novel interventions
that target the circadian system would appear to be a critical
theme for future BD research. Considerable research has
been dedicated to the characterization of circadian mechanisms implicated in the pathophysiology of BD. The most
promising pathways include i) melatonin synthesis and modulation of melatonin receptors, in particular by monoamine
neurotransmission and pulsatile melatonin release regulations;
ii) the brain circadian clock, in particular ARNTL1, CLOCK,
GSK3b, RORA and RORB genes and their regulation and
iii) factors (peptide, proteins, light, etc.) and mechanisms of
modulation of the circadian clock and monoamine neurotransmission. The exploration of GABAergic, dopaminergic,
serotonergic and glutamatergic neurotransmission is also of
major interest, in particular the multiple links between these
systems and circadian rhythms.
It should be emphasized that factors associated with disease
vulnerability and drug response are not necessarily the same.
In terms of future drug development, the exploration of the
biological pathways involved in successful treatments is of
major interest. Lithium and, to a lesser extent, valproate
have produced interesting data. Biomarkers of response of
8
nonpharmacological treatments represent an important
insufficiently covered area of research.
Based on the exploration of the mechanisms underlying lithium efficacy, GSK3b seems to play a central role. However,
GSK3b is involved in many molecular cascades (MAP-1B,
tau, Heat shock factor protein 1, C-JUN, C-AMP Response
Element-binding protein, Cyclin D, b-catenin, etc.) and it
remains unclear which is involved in lithium prophylactic efficacy and in tolerance. Other pathways of interest include myoinositol pathway, WINT pathway, Trkb/BDNF pathway or
protein kinase C. Close links between circadian rhythms and
GABA-ergic, dopaminergic and glutamatergic neurotransmissions lead also to consider lithium effects on these neurotransmitter systems. Lithium inhibits excitatory neurotransmission
by decreasing presynaptic DA activity and inactivating
postsynaptic G-proteins. It also exerts an inhibitory effect
downstream on the adenyl cyclase system, and, via effects on
cAMP, modulates further neurotransmission. Similarly,
lithium promotes inhibitory neurotransmission through its
modulation of glutamatergic neurotransmission by downregulating the NMDA receptor and inhibiting the myo-inositol
second messenger system, which is responsible for maintaining
signaling efficiency. When activated, the myo-inositol system
leads to phosphorylation of phosphoinositides, which in turn
initiate two second messenger pathways involving diaglycerol
and inositol triphosphate. These components of the phosphorylation cycle are responsible for modulating neurotransmission
and regulating genetic transcription. Chronic modulation of
this cycle through lithium exposure eventually alters gene
transcription, including circadian genes. Lithium additionally
inhibits neurotransmission by facilitating the release of
GABA and upregulating the GABAB receptor.
6.
Expert opinion
More than a decade after the development of atypical antipsychotics in BD, virtually no new compounds have emerged in
this field. The drug development pipeline is almost empty
with only three available main classes of mood stabilizers
(lithium, anticonvulsants and atypical antipsychotics). The
development of hypothesis regarding pathways altered in BD
should help renew interest in the pathophysiology of BD
and increase prospects for novel pharmacological approaches
to BD.
Clinical, actigraphic, biochemical, genetic, pharmacogenetic and gene expression studies have consolidated the
hypotheses that major disruptions in sleep and circadian
rhythm regulation pathways occur in BD and this research
has provided new insights into the pathophysiological
processes involved in the evolution and progression of BD,
alongside a better understanding of the putative mechanisms
of action of existing treatments (mainly lithium). While these
pathways offer an opportunity to develop novel approaches,
this review demonstrates that the level of evidence implicating
which genes/proteins might be targeted by drugs remains
Expert Opin. Ther. Targets (2015) 19(6)
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
relatively low and requires further replication in large-scale
well-conducted studies. The next stage of research will need
to incorporate comprehensive translational approaches to
sleep and circadian rhythm pathways, ranging from animal
to human cellular models to provide reliable models for
high-throughput screening of new drugs. Combinations of
phenotypic approaches, large-scale analyses with time
frequency methods and ‘omics’ (genomics, transcriptomic,
proteomic, methylomic) will also be necessary.
Phenotype studies, large data collection analysis
and biochemical markers
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
6.1
Characterization of sleep disturbances and circadian rhythm
disruptions in BD cases is common, and persistence of sleep
abnormalities during remission has been identified as a predictor of relapse [4]. Several studies have addressed this issue
using questionnaires that provide quick and inexpensive
assessments of sleep parameters and circadian rhythms. However, the association between these basic assessments and
endogenous measures of sleep or circadian rhythms requires
clarification [182].
More efforts dedicated to ecological assessments such as
actigraphy are required to gain more detailed insights into
daily sleep and circadian rhythm patterns and how they vary
according to environmental stressors and so on. Almost all
ecological studies (using actigraphy for example) have
included small samples (around 30 per study) and few have
targeted BD as compared with a range of mood disorders.
Although two meta-analyses [81,183] have clearly demonstrated
that sleep quality and sleep/wake regularity parameters are
altered among BD cases in remission, little is known regarding variability of such parameters. It has been hypothesized
that for a given parameter, interday or intraday variations
would be more important than the quantity (mean) of the
parameter [72]. This could be achieved only if studies include
larger samples assessed for long periods of time to capture
this variability. Furthermore, the whole field has used the
case--healthy control design, rather than addressing the more
important and clinically relevant question of whether BD is
associated with circadian abnormalities that are not seen in,
for example, unipolar disorders or psychosis.
Initiatives such as Chronorecord have been developed to
allow extended ecological assessments of cases and to provide
feedback to patients in clinical settings [184,185]. This desktop
computer-based assessment is now being replaced by new
technologies that are able to collect data from sensors in
smartphones, and wearable technologies [186]. Actigraphs can
also be worn for long periods of time to collect multiple
parameters concerning sleep and activity, although this
approach does not allow for subjective self-ratings unless
paired with other technologies of self-observations.
Although offering a robust measure of physiological processes, biochemical measures are of more limited use due to
their invasiveness. Repeated collections of plasma for cortisol
or melatonin (e.g., hourly) over a whole day/night cycle are
not often feasible, as they are too disruptive to the individuals’
lifestyle. Collections of saliva rather than venous samples have
increased the feasibility of such biochemical investigations as
they allow a greater degree of self-management of the process.
Currently, this is an evolving field of research in BD, although
findings on cortisol levels are reported in a recent metaanalysis in BD [103]. The use of measures of core temperature
with ingestible capsules is another way to investigate circadian
rhythms that are close to physiological processes [187], but
there are currently no available studies in BD during remission. All these measures can be used to assess circadian
rhythms but also can provide information about the external
validity of questionnaires and actigraphy that are of easier
use in clinical and research practices in large samples.
Human cells and animal models for screening
of new drugs
6.2
More recently, cellular models that can be used to assess
circadian rhythms have been developed in BD. To date, cultured cells derived from human skin biopsies, blood samples
or hair follicle cells have only been anecdotally used to test
transcriptomic and epigenetic aspects related to circadian
pathways in BD. The development of this research field is a
prerequisite to identify dysfunctional pathways that could be
targeted for drug development. Development of cellular
models is rendered easy by the use of peripheral blood
mononuclear cells or fibroblasts using skin biopsy. Induced
pluripotent stem-cell technology and study of differentiated
neuronal lineages from fibroblasts have not yet been
developed in the study of circadian rhythms in BD but their
use can help high-throughput pharmaceutical drug screening
and the study of expression and transcription profiles. Moreover, the modification of such profiles after incubation of cells
with lithium salts [188] (or other drugs to screen) can help
identify how drugs that are known or under development
can modify these profiles.
Postmortem tissues can also be used for methylomic and
RNA sequencing investigations and have provided promising
results in BD [189]. For example, the study of the brain
transcriptome identified dysregulation in circadian pathways
in BD [190].
A few animal models have been developed for BD, based
on sleep or circadian rhythm pathways such as the ClockD19
mice [191], transgenic mice overexpressing GSK3b, Per2 or
Per1 knock-out (KO) mice [192]. New animal models have
also been developed, which are not based on genetic manipulations, but on environmental paradigms that switch the
light--dark cycle [193]. They can extend the appraisal of broader
modifications of circadian pathways by environmental
challenges instead of focusing on one single gene (mutated
or KO mice). The development of new animal models could
be very useful to development of new drugs and would help
preclinical trials. Most of these animal models have used
Expert Opin. Ther. Targets (2015) 19(6)
9
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
F. Bellivier et al.
only lithium challenges but have not been used for larger
screening of compounds.
Both cellular models derived from human cells and animal
models can be used for the screening of compounds that are
likely to modify circadian rhythms. For example, preliminary
findings using 200,000 synthetic compounds on fibroblast
cells, suprachiasmatic nucleus and peripheral tissue explants
identified a few compounds that lengthen the period in
both central and peripheral clocks or shorten the period of
peripheral clocks [194], and identified cryptochrome inhibitors [195]. Animal model (CLOCK mutation) has been used
to test molecules that act as inhibitors of GSK-3b and attenuates the locomotor hyperactivity of this model of mania [196].
Such examples remain scarce and should lead to a more
generalized use of both cellular and animal models for the
screening of new drugs.
Large-scale pharmacogenetic studies
To date, pharmacogenetics of lithium response based on
sleep- and circadian-related genes is scarce. Although preliminary results have emerged regarding the implication of circadian genes in the response to lithium, the level of replication is
too weak to underlie a single gene within those associated
(ARNTL, TIMELESS, GSK3b and NR1D1) [132,148,197]. The
hypothesis that lithium could target these proteins and/or
act as a modifier of transcription of these genes shed some
light on potential specific mechanisms that are likely to support its mood stabilizer action and then be targeted by other
compounds. Such pharmacogenetic studies have been limited
by sample sizes, restriction to small sets of circadian genes and
unreplicated results. Large-scale pharmacogenetic studies such
as those planned within ConLiGen (the International
Consortium of Lithium Genetics) will offer new insight of
the genes involved in response to lithium and will determine
whether associated genes belong or are related to sleep and/
or circadian rhythm pathways. The goal of this collaboration
is to facilitate high-quality, well-powered analysis of lithium
treatment response data using data from GWAS. If positive
results in sleep or circadian pathways are generated by this
initiative, this will help focusing more precisely on a restricted
set of genes to be then used in cellular or animal models of
BD for the screening of new compounds.
6.3
Bioinformatics tools
Collecting large sets of data from different sources (clinical,
actigraphy, ‘omics’ approaches) over long or sequential
periods of time (months for actigraphy, incubated cells with
compounds assessed at different times) will obviously generate
an enormous volume of data (‘big data’ challenge). Bioinformatics tools will help to integrate and analyze such data.
One challenge is how to analyze phenotypic measures
recorded several times a day for weeks or months. This is
the case for actigraphy that generates a measure of activity
each minute. The relative disadvantage of such an assessment
of circadian rhythms on long periods of time is the generated
large amount of data (‘big data’) and, next the requirement of
complex mathematical modeling. Mathematical models could
achieve precise analysis of circadian rhythms of sleep or other
phenotypes (such as mood) that address time--frequency
methods such as discrete Fourier transform and continuous
or discrete wavelet transform analysis [198]. These methods
are useful in quantifying circadian (but also infradian and
ultradian) patterns in behavioral records. Combining
improved quality of data collection and mathematical analysis
will lead to a more precise characterization of circadian abnormalities in patients with BD that could be targeted when
studying drugs that are existing or in development.
A second challenge refers to ‘omics’ approaches that are
high-throughput molecular profiling techniques that produce
large data sets. Bioinformatics can help to extract relevant
biological information within specific pathways and study
connections between interconnected pathways. Advanced
computational strategies are developing rapidly to deal with
all these ‘omics’ layers.
More generally, from the pharmaceutical perspective, ‘big
data’ analyses have to face several challenges: i) volume of
data; ii) velocity (analytical speed); iii) variability of data;
and iv) complexity of data [199].
The data summarized in this review may represent a new
treatment paradigm for the development of a next generation
of drugs that target sleep and circadian rhythm pathways that
will be added to the pharmacological arsenal for maintenance
therapy in BD. However, this goal will be reached only if multidisciplinary and integrative approaches combine preclinical,
clinical, actigraphy, biochemistry and so-called ‘omics’ with
appropriate bioinformatics tools. This will lead to the identification of a circadian biosignature of BD used in humans,
cellular and animal models to screen new compounds.
Acknowledgment
We would like to acknowledge APBC Hospital F Widal,
Paris, for their technical support.
6.4
10
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest
in or financial conflict with the subject matter or materials
discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Expert Opin. Ther. Targets (2015) 19(6)
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
Bibliography
Papers of special note have been highlighted as
either of interest () or of considerable interest
() to readers.
1.
.
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
2.
.
3.
4.
.
5.
6.
7.
..
8.
.
9.
Scott J. Clinical parameters of circadian
rhythms in affective disorders.
Eur Neuropsychopharmacol
2011;21(Suppl 4):S671-5
This paper explores clinical parameters
representing direct or proxy measures
of disturbed circadian rhythms.
Gonzalez R. The relationship between
bipolar disorder and biological rhythms.
J Clin Psychiatry 2014;75(4):e323-31
A extensive rewiew of links between
BD and circadian rhythms.
Etain B, Milhiet V, Bellivier F, et al.
Genetics of circadian rhythms and mood
spectrum disorders.
Eur Neuropsychopharmacol
2011;21(Suppl 4):S676-82
Sylvia LG, Dupuy JM, Ostacher MJ,
et al. Sleep disturbance in euthymic
bipolar patients. J Psychopharmacol
2012;26(8):1108-12
Original research highlighting the
major need to treat sleep disturbances
during remission
Kaplan KA, Gruber J, Eidelman P, et al.
Hypersomnia in inter-episode bipolar
disorder: does it have prognostic
significance? J Affect Disord
2011;132(3):438-44
Grandin LD, Alloy LB, Abramson LY.
The social zeitgeber theory, circadian
rhythms, and mood disorders: review and
evaluation. Clin Psychol Rev
2006;26(6):679-94
Takahashi JS, Hong H-K, Ko CH, et al.
The genetics of mammalian circadian
order and disorder: implications for
physiology and disease. Nat Rev Genet
2008;9(10):764-75
Very complete review about the
genetics of circadian rhythms
and disorders.
Dardente H, Cermakian N. Molecular
circadian rhythms in central and
peripheral clocks in mammals.
Chronobiol Int 2007;24(2):195-213
Very complete review about the
molecular aspect of circadian rhythms.
Martinek S, Inonog S, Manoukian AS,
et al. A role for the segment polarity
gene shaggy/GSK-3 in the Drosophila
circadian clock. Cell 2001;105(6):769-79
10.
Yin L, Wang J, Klein PS, et al. Nuclear
receptor Rev-erbalpha is a critical
lithium-sensitive component of the
circadian clock. Science
2006;311(5763):1002-5
23.
Barassin S, Raison S, Saboureau M, et al.
Circadian tryptophan hydroxylase levels
and serotonin release in the
suprachiasmatic nucleus of the rat.
Eur J Neurosci 2002;15(5):833-40
11.
Bellet MM, Sassone-Corsi P.
Mammalian circadian clock and
metabolism - the epigenetic link.
J Cell Sci 2010;123(Pt 22):3837-48
24.
Shieh KR, Chu YS, Pan JT. Circadian
change of dopaminergic neuron activity:
effects of constant light and melatonin.
Neuroreport 1997;8(9-10):2283-7
12.
Bell-Pedersen D, Cassone VM,
Earnest DJ, et al. Circadian rhythms
from multiple oscillators: lessons from
diverse organisms. Nat Rev Genet
2005;6(7):544-56
25.
13.
Yamazaki S, Numano R, Abe M, et al.
Resetting central and peripheral circadian
oscillators in transgenic rats. Science
2000;288(5466):682-5
Khaldy H, León J, Escames G, et al.
Circadian rhythms of dopamine and
dihydroxyphenyl acetic acid in the mouse
striatum: effects of pinealectomy and of
melatonin treatment.
Neuroendocrinology 2002;75(3):201-8
26.
Castañeda TR, de Prado BM, Prieto D,
et al. Circadian rhythms of dopamine,
glutamate and GABA in the striatum and
nucleus accumbens of the awake rat:
modulation by light. J Pineal Res
2004;36(3):177-85
27.
Akhisaroglu M, Kurtuncu M, Manev H,
et al. Diurnal rhythms in quinpiroleinduced locomotor behaviors and striatal
D2/D3 receptor levels in mice.
Pharmacol Biochem Behav
2005;80(3):371-7
28.
Zeitzer JM, Dijk DJ, Kronauer R, et al.
Sensitivity of the human circadian
pacemaker to nocturnal light: melatonin
phase resetting and suppression. J Physiol
2000;526(Pt 3):695-702
Coon SL, McCune SK, Sugden D, et al.
Regulation of pineal alpha1B-adrenergic
receptor mRNA: day/night rhythm and
beta-adrenergic receptor/cyclic AMP
control. Mol Pharmacol
1997;51(4):551-7
29.
Benloucif S, Burgess HJ, Klerman EB,
et al. Measuring melatonin in humans.
J Clin Sleep Med 2008;4(1):66-9
Aston-Jones G, Chen S, Zhu Y, et al.
A neural circuit for circadian regulation
of arousal. Nat Neurosci 2001;4(7):732-8
30.
Morin LP. Serotonin and the regulation
of mammalian circadian rhythmicity.
Ann Med 1999;31(1):12-33
31.
Moore CM, Demopulos CM,
Henry ME, et al. Brain-to-serum lithium
ratio and age: an in vivo magnetic
resonance spectroscopy study.
Am J Psychiatry 2002;159(7):1240-2
32.
Hannibal J, Fahrenkrug J. Neuronal
input pathways to the brain’s biological
clock and their functional significance.
Adv Anat Embryol Cell Biol
2006;182:1-71
33.
Reghunandanan V, Reghunandanan R.
Neurotransmitters of the suprachiasmatic
nuclei. J Circadian Rhythms 2006;4:2
34.
Ying SW, Rusak B. Effects of
serotonergic agonists on firing rates of
photically responsive cells in the hamster
14.
Hastings M, O’Neill JS, Maywood ES.
Circadian clocks: regulators of endocrine
and metabolic rhythms. J Endocrinol
2007;195(2):187-98
15.
Panda S, Antoch MP, Miller BH, et al.
Coordinated transcription of key
pathways in the mouse by the circadian
clock. Cell 2002;109(3):307-20
16.
Lewy AJ, Wehr TA, Goodwin FK, et al.
Light suppresses melatonin secretion in
humans. Science 1980;210(4475):1267-9
17.
18.
19.
20.
Lewy AJ, Sack RL. The dim light
melatonin onset as a marker for circadian
phase position. Chronobiol Int
1989;6(1):93-102
Hofstra WA, de Weerd AW. How to
assess circadian rhythm in humans:
a review of literature. Epilepsy Behav
2008;13(3):438-44
21.
Wesemann W, Weiner N. Circadian
rhythm of serotonin binding in rat brain.
Prog Neurobiol 1990;35(6):405-28
22.
Weiner N, Clement HW, Gemsa D,
et al. Circadian and seasonal rhythms of
5-HT receptor subtypes, membrane
anisotropy and 5-HT release in
hippocampus and cortex of the rat.
Neurochem Int 1992;21(1):7-14
Expert Opin. Ther. Targets (2015) 19(6)
11
F. Bellivier et al.
suprachiasmatic nucleus. Brain Res
1994;651(1-2):37-46
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
35.
Rea MA, Barrera J, Glass JD, et al.
Serotonergic potentiation of photic phase
shifts of the circadian activity rhythm.
Neuroreport 1995;6(10):1417-20
47.
.
Milhiet V, Boudebesse C, Bellivier F,
et al. Circadian abnormalities as markers
of susceptibility in bipolar disorders.
Front Biosci (Schol Ed) 2014;6:120-37
Comprehensive review on circadian
biomarkers in BD.
salivary melatonin secretion. PLoS One
2008;3(8):e3055
59.
Randler C, Schaal S. Morningnesseveningness, habitual sleep-wake variables
and cortisol level. Biol Psychol
2010;85(1):14-18
60.
Caci H, Nadalet L, Staccini P, et al. The
composite scale of morningness: further
psychometric properties and temporal
stability. Eur Psychiatry
2000;15(4):278-81
61.
Greenwood KM. Long-term stability and
psychometric properties of the
Composite Scale of Morningness.
Ergonomics 1994;37(2):377-83
36.
Fite KV, Janusonis S, Foote W, et al.
Retinal afferents to the dorsal raphe
nucleus in rats and Mongolian gerbils.
J Comp Neurol 1999;414(4):469-84
48.
Horne JA, Ostberg O. A self-assessment
questionnaire to determine morningnesseveningness in human circadian rhythms.
Int J Chronobiol 1976;4(2):97-110
37.
Jiang ZG, Teshima K, Yang Y, et al.
Pre- and postsynaptic actions of
serotonin on rat suprachiasmatic nucleus
neurons. Brain Res
2000;866(1-2):247-56
49.
Smith CS, Reilly C, Midkiff K.
Evaluation of three circadian rhythm
questionnaires with suggestions for an
improved measure of morningness.
J Appl Psychol 1989;74(5):728-38
38.
Lambert GW, Reid C, Kaye DM, et al.
Effect of sunlight and season on
serotonin turnover in the brain. Lancet
2002;360(9348):1840-2
50.
62.
39.
Yuan Q, Lin F, Zheng X, et al.
Serotonin modulates circadian
entrainment in Drosophila. Neuron
2005;47(1):115-27
Zavada A, Gordijn MC, Beersma DG,
et al. Comparison of the munich
chronotype questionnaire with the horneostberg’s morningness-eveningness score.
Chronobiol Int 2005;22(2):267-78
Wood J, Birmaher B, Axelson D, et al.
Replicable differences in preferred
circadian phase between bipolar disorder
patients and control individuals.
Psychiatry Res 2009;166(2-3):201-9
51.
Vink JM, Groot AS, Kerkhof GA, et al.
Genetic analysis of morningness and
eveningness. Chronobiol Int
2001;18(5):809-22
63.
Ahn YM, Chang J, Joo YH, et al.
Chronotype distribution in bipolar I
disorder and schizophrenia in a Korean
sample. Bipolar Disord 2008;10(2):271-5
52.
Klei L, Reitz P, Miller M, et al.
Heritability of morningness-eveningness
and self-report sleep measures in a
family-based sample of 521 hutterites.
Chronobiol Int 2005;22(6):
1041-54
64.
Mansour HA, Wood J, Chowdari KV,
et al. Circadian phase variation in bipolar
I disorder. Chronobiol Int
2005;22(3):571-84
65.
Boudebesse C, Lajnef M, Geoffroy PA,
et al. Chronotypes of bipolar patients in
remission: validation of the French
version of the circadian type inventory in
the FACE-BD sample. Chronobiol Int
2013;30(8):1042-9
66.
Di Milia L, Smith PA, Folkard S.
A validation of the revised circadian type
inventory in a working sample.
Personal Individ Differ
2005;39(7):1293-305
67.
Chung JK, Lee KY, Kim SH, et al.
Circadian rhythm characteristics in mood
disorders: comparison among bipolar I
disorder, bipolar II disorder and
recurrent major depressive disorder.
Clin Psychopharmacol Neurosci
2012;10(2):110-16
68.
Ottoni GL, Antoniolli E, Lara DR.
Circadian preference is associated with
emotional and affective temperaments.
Chronobiol Int 2012;29(6):786-93
69.
Kaplan KA, Talbot LS, Gruber J, et al.
Evaluating sleep in bipolar disorder:
comparison between actigraphy,
polysomnography, and sleep diary.
Bipolar Disord 2012;14(8):870-9
Original study that used various
methodologies to measure sleep in BD.
40.
41.
Snyder SH, Borjigin J, Sassone-Corsi P.
Discovering light effects on the brain.
Am J Psychiatry 2006;163(5):771
Witkovsky P. Dopamine and retinal
function. Doc Ophthalmol
2004;108(1):17-40
42.
Monti JM, Monti D. The involvement
of dopamine in the modulation of sleep
and waking. Sleep Med Rev
2007;11(2):113-33
43.
Lima MM, Andersen ML, Reksidler AB,
et al. Blockage of dopaminergic D(2)
receptors produces decrease of REM but
not of slow wave sleep in rats after REM
sleep deprivation. Behav Brain Res
2008;188(2):406-11
44.
45.
46.
.
12
Yujnovsky I, Hirayama J, Doi M, et al.
Signaling mediated by the dopamine
D2 receptor potentiates circadian
regulation by CLOCK:BMAL1.
Proc Natl Acad Sci USA
2006;103(16):6386-91
Simonneaux V, Ribelayga C. Generation
of the melatonin endocrine message in
mammals: a review of the complex
regulation of melatonin synthesis by
norepinephrine, peptides, and other
pineal transmitters. Pharmacol Rev
2003;55(2):325-95
Murray G, Harvey A. Circadian rhythms
and sleep in bipolar disorder.
Bipolar Disord 2010;12(5):459-72
Interesting article examining sleep and
circadian rhythms abnormalities in BD.
53.
Koskenvuo M, Hublin C, Partinen M,
et al. Heritability of diurnal type:
a nationwide study of 8753 adult twin
pairs. J Sleep Res 2007;16(2):
156-62
54.
Barclay NL, Eley TC, Buysse DJ, et al.
Diurnal preference and sleep quality:
same genes? A study of young adult
twins. Chronobiol Int 2010;27(2):278-96
55.
Hakkarainen R, Johansson C,
Kieseppä T, et al. Seasonal changes, sleep
length and circadian preference among
twins with bipolar disorder.
BMC Psychiatry 2003;3:6
56.
Kerkhof GA, Van Dongen HP.
Morning-type and evening-type
individuals differ in the phase position of
their endogenous circadian oscillator.
Neurosci Lett 1996;218(3):153-6
57.
58.
Duffy JF, Rimmer DW, Czeisler CA.
Association of intrinsic circadian period
with morningness-eveningness, usual
wake time, and circadian phase.
Behav Neurosci 2001;115(4):
895-9
Burgess HJ, Fogg LF. Individual
differences in the amount and timing of
Expert Opin. Ther. Targets (2015) 19(6)
.
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
70.
71.
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
72.
.
73.
.
74.
.
75.
76.
77.
78.
.
Sitaram N, Nurnberger JI Jr,
Gershon ES, et al. Cholinergic regulation
of mood and REM sleep: potential
model and marker of vulnerability to
affective disorder. Am J Psychiatry
1982;139(5):571-6
Knowles JB, Cairns J, MacLean AW,
et al. The sleep of remitted bipolar
depressives: comparison with sex and agematched controls. Can J Psychiatry
1986;31(4):295-8
Geoffroy PA, Boudebesse C, Bellivier F,
et al. Sleep in remitted bipolar disorder:
a naturalistic case-control study using
actigraphy. J Affect Disord 2014;158:1-7
Original research that used actigraphy
by controlling for many confusion
factors, and that identified a
combination of markers to identify BD
patients from healthy subjects.
Gershon A, Thompson WK,
Eidelman P, et al. Restless pillow, ruffled
mind: sleep and affect coupling in
interepisode bipolar disorder.
J Abnorm Psychol 2012;121(4):863-73
Very interesting reports about patients
in remission.
Harvey AG, Schmidt DA, Scarna A,
et al. Sleep-related functioning in
euthymic patients with bipolar disorder,
patients with insomnia, and subjects
without sleep problems. Am J Psychiatry
2005;162(1):50-7
Very interesting study comparing three
groups of patients with BD, with
insomnia and healthy controls.
Jones SH, Hare DJ, Evershed K.
Actigraphic assessment of circadian
activity and sleep patterns in bipolar
disorder. Bipolar Disord
2005;7(2):176-86
Millar A, Espie CA, Scott J. The sleep of
remitted bipolar outpatients: a controlled
naturalistic study using actigraphy.
J Affect Disord 2004;80(2-3):145-53
Mullin BC, Harvey AG, Hinshaw SP.
A preliminary study of sleep in
adolescents with bipolar disorder,
ADHD, and non-patient controls.
Bipolar Disord 2011;13(4):425-32
Ritter PS, Marx C, Lewtschenko N,
et al. The characteristics of sleep in
patients with manifest bipolar disorder,
subjects at high risk of developing the
disease and healthy controls.
J Neural Transm 2012;119(10):1173-84
Original interesting report using
actigraphy in high-risk subjects.
79.
80.
81.
..
Salvatore P, Ghidini S, Zita G, et al.
Circadian activity rhythm abnormalities
in ill and recovered bipolar I disorder
patients. Bipolar Disord
2008;10(2):256-65
Ankers D, Jones SH. Objective
assessment of circadian activity and sleep
patterns in individuals at behavioural risk
of hypomania. J Clin Psychol
2009;65(10):1071-86
Geoffroy PA, Scott J, Boudebesse C,
et al. Sleep in patients with remitted
bipolar disorders: a meta-analysis of
actigraphy studies. Acta Psychiatr Scand
2014;131(2):89-99
Meta-analysis of all studies using
actigraphy in remitted patients
with BD.
82.
Robillard R, Naismith SL, Rogers NL,
et al. Delayed sleep phase in young
people with unipolar or bipolar affective
disorders. J Affect Disord
2013;145(2):260-3
83.
Jones SH, Tai S, Evershed K, et al. Early
detection of bipolar disorder: a pilot
familial high-risk study of parents with
bipolar disorder and their adolescent
children. Bipolar Disord
2006;8(4):362-72
84.
Hamet P, Tremblay J. Genetics of the
sleep-wake cycle and its disorders.
Metabolism 2006;55(10 Suppl 2):S7-12
85.
Dauvilliers Y, Maret S, Tafti M.
Genetics of normal and pathological
sleep in humans. Sleep Med Rev
2005;9(2):91-100
Interesting general review of sleep
mechanisms in humans.
..
86.
Janney CA, Fagiolini A, Swartz HA,
et al. Are adults with bipolar disorder
active? Objectively measured physical
activity and sedentary behavior using
accelerometry. J Affect Disord
2014;152-154:498-504
87.
Monk TH, Reynolds CF, Buysse DJ,
et al. The relationship between lifestyle
regularity and subjective sleep quality.
Chronobiol Int 2003;20(1):97-107
88.
Monk TH, Buysse DJ, Potts JM, et al.
Morningness-eveningness and lifestyle
regularity. Chronobiol Int
2004;21(3):435-43
89.
Sylvia LG, Alloy LB, Hafner JA, et al.
Life events and social rhythms in bipolar
.
spectrum disorders: a prospective study.
Behav Ther 2009;40(2):131-41
A prospective study identifying
poor outcomes.
90.
Giglio LM, Magalhães PV,
Andreazza AC, et al. Development and
use of a biological rhythm interview.
J Affect Disord 2009;118(1-3):161-5
91.
Meyer TD, Maier S. Is there evidence
for social rhythm instability in people at
risk for affective disorders? Psychiatry Res
2006;141(1):103-14
92.
Shen GH, Alloy LB, Abramson LY, et al.
Social rhythm regularity and the onset of
affective episodes in bipolar spectrum
individuals. Bipolar Disord
2008;10(4):520-9
93.
Malkoff-Schwartz S, Frank E,
Anderson B, et al. Stressful life events
and social rhythm disruption in the onset
of manic and depressive bipolar episodes:
a preliminary investigation.
Arch Gen Psychiatry 1998;55(8):702-7
94.
Cervantes P, Gelber S, Kin FN, et al.
Circadian secretion of cortisol in bipolar
disorder. J Psychiatry Neurosci
2001;26(5):411-16
95.
Deshauer D, Duffy A, Alda M, et al.
The cortisol awakening response in
bipolar illness: a pilot study.
Can J Psychiatry 2003;48(7):462-6
96.
Bartels M, Van den Berg M, Sluyter F,
et al. Heritability of cortisol levels: review
and simultaneous analysis of twin studies.
Psychoneuroendocrinology
2003;28(2):121-37
97.
Kupper N, de Geus EJC,
van den Berg M, et al. Familial
influences on basal salivary cortisol in an
adult population.
Psychoneuroendocrinology
2005;30(9):857-68
98.
Franz CE, York TP, Eaves LJ, et al.
Genetic and environmental influences on
cortisol regulation across days and
contexts in middle-aged men.
Behav Genet 2010;40(4):467-79
99.
Vinberg M, Bennike B, Kyvik KO, et al.
Salivary cortisol in unaffected twins
discordant for affective disorder.
Psychiatry Res 2008;161(3):292-301
100. Wüst S, Wolf J, Hellhammer DH, et al.
The cortisol awakening response normal values and confounds.
Noise Health 2000;2(7):79-88
101. Ellenbogen MA, Santo JB, Linnen A-M,
et al. High cortisol levels in the offspring
Expert Opin. Ther. Targets (2015) 19(6)
13
F. Bellivier et al.
of parents with bipolar disorder during
two weeks of daily sampling.
Bipolar Disord 2010;12(1):77-86
102. Deshauer D, Duffy A, Meaney M, et al.
Salivary cortisol secretion in remitted
bipolar patients and offspring of bipolar
parents. Bipolar Disord 2006;8(4):345-9
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
103. Girshkin L, Matheson SL, Shepherd AM,
et al. Morning cortisol levels in
schizophrenia and bipolar disorder:
a meta-analysis.
Psychoneuroendocrinology
2014;49:187-206
104. Lewy AJ, Nurnberger JI, Wehr TA, et al.
Supersensitivity to light: possible trait
marker for manic-depressive illness.
Am J Psychiatry 1985;142(6):725-7
.
Major discovery in aptients with BD.
105. Nathan PJ, Burrows GD, Norman TR.
Melatonin sensitivity to dim white light
in affective disorders.
Neuropsychopharmacology
1999;21(3):408-13
106. Lam RW, Berkowitz AL, Berga SL, et al.
Melatonin suppression in bipolar and
unipolar mood disorders. Psychiatry Res
1990;33(2):129-34
107. Whalley LJ, Perini T, Shering A, et al.
Melatonin response to bright light in
recovered, drug-free, bipolar patients.
Psychiatry Res 1991;38(1):13-19
108. Nurnberger JI Jr, Adkins S, Lahiri DK,
et al. Melatonin suppression by light in
euthymic bipolar and unipolar patients.
Arch Gen Psychiatry 2000;57(6):
572-9
.
Interesting original report.
109. Kennedy SH, Kutcher SP, Ralevski E,
et al. Nocturnal melatonin and 24-hour
6-sulphatoxymelatonin levels in various
phases of bipolar affective disorder.
Psychiatry Res 1996;63(2-3):219-22
110. Nováková M, Praško J, Látalová K, et al.
The circadian system of patients with
bipolar disorder differs in episodes of
mania and depression. Bipolar Disord
2014. [Epub ahead of print]
111. Robillard R, Naismith SL, Rogers NL,
et al. Sleep-wake cycle and melatonin
rhythms in adolescents and young adults
with mood disorders: comparison of
unipolar and bipolar phenotypes.
Eur Psychiatry 2013;28(7):412-16
.
Original comparison between unipolar
and bipolar patients.
112. Hallam KT, Olver JS, Chambers V,
et al. The heritability of melatonin
14
.
secretion and sensitivity to bright
nocturnal light in twins.
Psychoneuroendocrinology
2006;31(7):867-75
Original report about the heritability
of melatonin mechanisms.
113. Nurnberger JI Jr, Berrettini W,
Tamarkin L, et al. Supersensitivity to
melatonin suppression by light in young
people at high risk for affective disorder.
A preliminary report.
Neuropsychopharmacology
1988;1(3):217-23
114. Sarrazin S, Etain B, Vederine F-E, et al.
MRI exploration of pineal volume in
bipolar disorder. J Affect Disord
2011;135(1-3):377-9
115. Byrne EM, Heath AC, Madden PA,
et al. Testing the role of circadian genes
in conferring risk for psychiatric
disorders. Am J Med Genet Part B
Neuropsychiatr Genet
2014;165(3):254-60
116. Lee KY, Ahn YM, Joo E-J, et al. No
association of two common SNPs at
position -1727 A/T, -50 C/T of GSK-3
beta polymorphisms with schizophrenia
and bipolar disorder of Korean
population. Neurosci Lett
2006;395(2):175-88
117. Nievergelt CM, Kripke DF, Barrett TB,
et al. Suggestive evidence for association
of the circadian genes PERIOD3 and
ARNTL with bipolar disorder. Am J
Med Genet Part B Neuropsychiatr Genet
2006;141B(3):234-41
118. Kripke DF, Nievergelt CM, Joo E, et al.
Circadian polymorphisms associated with
affective disorders. J Circadian Rhythms
2009;7:2
119. Lachman HM, Pedrosa E, Petruolo OA,
et al. Increase in GSK3beta gene copy
number variation in bipolar disorder.
Am J Med Genet Part B
Neuropsychiatr Genet
2007;144B(3):259-65
120. Brown SA, Fleury-Olela F, Nagoshi E,
et al. The period length of fibroblast
circadian gene expression varies widely
among human individuals. PLoS Biol
2005;3(10):e338
121. Akashi M, Soma H, Yamamoto T, et al.
Noninvasive method for assessing the
human circadian clock using hair follicle
cells. Proc Natl Acad Sci USA
2010;107(35):15643-8
.
Very interesting study.
Expert Opin. Ther. Targets (2015) 19(6)
122. Brown SA, Kunz D, Dumas A, et al.
Molecular insights into human daily
behavior. Proc Natl Acad Sci USA
2008;105(5):1602-7
123. Yang S, Van Dongen HP, Wang K,
et al. Assessment of circadian function in
fibroblasts of patients with bipolar
disorder. Mol Psychiatry
2009;14(2):143-55
..
Original in-vitro study
examining fibroblasts.
124. Coyle JT. What can a clock mutation in
mice tell us about bipolar disorder?
Proc Natl Acad Sci USA
2007;104(15):6097-8
125. Roybal K, Theobold D, Graham A, et al.
Mania-like behavior induced by
disruption of CLOCK. Proc Natl Acad
Sci USA 2007;104(15):6406-11
.
Animal model of mania induced by
disruption of a circadian gene.
126. Prickaerts J, Moechars D, Cryns K, et al.
Transgenic mice overexpressing glycogen
synthase kinase 3beta: a putative model
of hyperactivity and mania. J Neurosci
2006;26(35):9022-9
.
Another animal model of mania
induced by disruption of a
circadian gene.
127. Le-Niculescu H, Patel SD, Bhat M, et al.
Convergent functional genomics of
genome-wide association data for bipolar
disorder: comprehensive identification of
candidate genes, pathways and
mechanisms. Am J Med Genet Part B
Neuropsychiatr Genet
2009;150B(2):155-81
128. Patel SD, Le-Niculescu H, Koller DL,
et al. Coming to grips with complex
disorders: genetic risk prediction in
bipolar disorder using panels of genes
identified through convergent functional
genomics. Am J Med Genet Part B
Neuropsychiatr Genet
2010;153B(4):850-77
129. Benedetti F, Serretti A, Colombo C,
et al. A glycogen synthase kinase 3-beta
promoter gene single nucleotide
polymorphism is associated with age at
onset and response to total sleep
deprivation in bipolar depression.
Neurosci Lett 2004;368(2):
123-6
130. Benedetti F, Bernasconi A, Lorenzi C,
et al. A single nucleotide polymorphism
in glycogen synthase kinase 3-beta
promoter gene influences onset of illness
in patients affected by bipolar disorder.
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
Neurosci Lett 2004;355(1-2):
37-40
131.
132.
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
133.
134.
135.
136.
.
137.
.
138.
139.
Benedetti F, Dallaspezia S, Colombo C,
et al. A length polymorphism in the
circadian clock gene Per3 influences age
at onset of bipolar disorder.
Neurosci Lett 2008;445(2):184-7
Benedetti F, Serretti A, Pontiggia A,
et al. Long-term response to lithium salts
in bipolar illness is influenced by the
glycogen synthase kinase 3-beta -50 T/C
SNP. Neurosci Lett 2005;376(1):
51-5
Severino G, Manchia M, Contu P, et al.
Association study in a Sardinian sample
between bipolar disorder and the nuclear
receptor REV-ERBalpha gene, a critical
component of the circadian clock system.
Bipolar Disord 2009;11(2):215-20
Benedetti F, Serretti A, Colombo C,
et al. Influence of CLOCK gene
polymorphism on circadian mood
fluctuation and illness recurrence in
bipolar depression. Am J Med Genet
Part B Neuropsychiatr Genet
2003;123B(1):23-6
Shi J, Wittke-Thompson JK, Badner JA,
et al. Clock genes may influence bipolar
disorder susceptibility and dysfunctional
circadian rhythm. Am J Med Genet Part
B Neuropsychiatr Genet
2008;147B(7):1047-55
Lee KY, Song JY, Kim SH, et al.
Association between CLOCK 3111T/C
and preferred circadian phase in Korean
patients with bipolar disorder.
Prog Neuropsychopharmacol
Biol Psychiatry 2010;34(7):1196-201
Study associating a clock variant with
a circadian phase.
Etain B, Jamain S, Milhiet V, et al.
Association between circadian genes,
bipolar disorders and chronotypes.
Chronobiol Int 2014;31(7):807-14
Study associating circadian genetic
variants, at-risk for BD,
to chronotypes.
Etain B, Dumaine A, Bellivier F, et al.
Genetic and functional abnormalities of
the melatonin biosynthesis pathway in
patients with bipolar disorder.
Hum Mol Genet 2012;21(18):4030-7
Geoffroy PA, Boudebesse C, Henrion A,
et al. An ASMT variant associated with
bipolar disorder influences sleep and
circadian rhythms: a pilot study.
Genes Brain Behav 2014;13(3):299-304
140.
Kripke DF, Klimecki WT,
Nievergelt CM, et al. Circadian
polymorphisms in night owls, in
bipolars, and in non-24-hour sleep
cycles. Psychiatry Investig
2014;11(4):345-62
141.
Geoffroy P, Bellivier F, Leboyer M, et al.
Can the response to mood stabilizers be
predicted in bipolar disorder?
Front Biosci(Elite Ed) 2014;6:120-38
142.
Geoffroy PA, Etain B, Sportiche S, et al.
Circadian biomarkers in patients with
bipolar disorder: promising putative
predictors of lithium response. Int J
Bipolar Disord 2014;2(1):5
143.
Freland L, Beaulieu J-M. Inhibition of
GSK3 by lithium, from single molecules
to signaling networks.
Front Mol Neurosci 2012;5:14
144.
Szczepankiewicz A, Rybakowski JK,
Suwalska A, et al. Association study of
the glycogen synthase kinase-3beta gene
polymorphism with prophylactic lithium
response in bipolar patients. World J
Biol Psychiatry 2006;7(3):158-61
Well-conducted pharmacogenetic study
of Lithium.
.
145.
.
146.
Michelon L, Meira-Lima I, Cordeiro Q,
et al. Association study of the INPP1,
5HTT, BDNF, AP-2beta and GSK3beta GENE variants and restrospectively
scored response to lithium prophylaxis in
bipolar disorder. Neurosci Lett
2006;403(3):288-93
Interesting pharmacogenetic study
of lithium.
receptor polymorphism is associated with
lithium response in bipolar patients.
Neuro Endocrinol Lett
2011;32(4):545-51
150. Bunney BG, Bunney WE. Mechanisms
of rapid antidepressant effects of sleep
deprivation therapy: clock genes and
circadian rhythms. Biol Psychiatry
2013;73(12):1164-71
151. Golden RN, Gaynes BN, Ekstrom RD,
et al. The efficacy of light therapy in the
treatment of mood disorders: a review
and meta-analysis of the evidence.
Am J Psychiatry 2005;162(4):656-62
152. Colombo C, Lucca A, Benedetti F, et al.
Total sleep deprivation combined with
lithium and light therapy in the
treatment of bipolar depression:
replication of main effects and
interaction. Psychiatry Res
2000;95(1):43-53
153. Altshuler LL, Frye MA, Gitlin MJ.
Acceleration and augmentation strategies
for treating bipolar depression.
Biol Psychiatry 2003;53(8):
691-700
154. Benedetti F, Barbini B, Fulgosi MC,
et al. Combined total sleep deprivation
and light therapy in the treatment of
drug-resistant bipolar depression: acute
response and long-term remission rates.
J Clin Psychiatry 2005;66(12):
1535-40
155. Leibenluft E, Turner EH,
Feldman-Naim S, et al. Light therapy in
patients with rapid cycling bipolar
disorder: preliminary results.
Psychopharmacol Bull
1995;31(4):705-10
.
Study about luminotherapy in BD.
Manchia M, Squassina A, Congiu D,
et al. Interacting genes in lithium
prophylaxis: preliminary results of an
exploratory analysis on the role of
DGKH and NR1D1 gene
polymorphisms in 199 Sardinian bipolar
patients. Neurosci Lett
2009;467(2):67-71
156. Sit D, Wisner KL, Hanusa BH, et al.
Light therapy for bipolar disorder: a case
series in women. Bipolar Disord
2007;9(8):918-27
147.
Campos-de-Sousa S, Guindalini C,
Tondo L, et al. Nuclear receptor rev-erb{alpha} circadian gene variants and
lithium carbonate prophylaxis in bipolar
affective disorder. J Biol Rhythms
2010;25(2):132-7
157. Wu JC, Kelsoe JR, Schachat C, et al.
Rapid and sustained antidepressant
response with sleep deprivation and
chronotherapy in bipolar disorder.
Biol Psychiatry 2009;66(3):
298-301
148.
McCarthy MJ, Nievergelt CM,
Shekhtman T, et al. Functional genetic
variation in the Rev-Erbalpha pathway
and lithium response in the treatment of
bipolar disorder. Genes Brain Behav
2011;10(8):852-61
149.
Szczepankiewicz A, Rybakowski JK,
Suwalska A, et al. Glucocorticoid
158. Wehr TA, Turner EH, Shimada JM,
et al. Treatment of rapidly cycling
bipolar patient by using extended bed
rest and darkness to stabilize the timing
and duration of sleep. Biol Psychiatry
1998;43(11):822-8
.
Original study of extended bed rest
and darkness treatment.
Expert Opin. Ther. Targets (2015) 19(6)
15
F. Bellivier et al.
159. Barbini B, Benedetti F, Colombo C,
et al. Dark therapy for mania: a pilot
study. Bipolar Disord 2005;7(1):
98-101
160. Phelps J. Dark therapy for bipolar
disorder using amber lenses for blue light
blockade. Med Hypotheses
2008;70(2):224-9
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
161. Kaplan KA, Harvey AG. Behavioral
treatment of insomnia in bipolar
disorder. Am J Psychiatry
2013;170(7):716-20
162. Steinan MK, Krane-Gartiser K,
Langsrud K, et al. Cognitive behavioral
therapy for insomnia in euthymic bipolar
disorder: study protocol for a randomized
controlled trial. Trials 2014;15:24
163. Miklowitz DJ, Scott J. Psychosocial
treatments for bipolar disorder: costeffectiveness, mediating mechanisms, and
future directions. Bipolar Disord
2009;11(Suppl 2):110-22
.
Interesting overview about
psychosocial treatments for BD.
164. Frank E, Kupfer DJ, Thase ME, et al.
Two-year outcomes for interpersonal and
social rhythm therapy in individuals with
bipolar I disorder. Arch Gen Psychiatry
2005;62(9):996-1004
.
Interesting study about interpersonal
and social rhythm therapy.
165. Reinares M, Sánchez-Moreno J,
Fountoulakis KN. Psychosocial
interventions in bipolar disorder: what,
for whom, and when. J Affect Disord
2014;156:46-55
166. McClung CA. Circadian genes, rhythms
and the biology of mood disorders.
Pharmacol Ther 2007;114(2):222-32
..
Very interesting review.
167. Abe M, Herzog ED, Block GD. Lithium
lengthens the circadian period of
individual suprachiasmatic nucleus
neurons. Neuroreport
2000;11(14):3261-4
168. Li J, Lu W-Q, Beesley S, et al. Lithium
impacts on the amplitude and period of
the molecular circadian clockwork.
PLoS One 2012;7(3):e33292
169. Hallam KT, Olver JS, Horgan JE, et al.
Low doses of lithium carbonate reduce
melatonin light sensitivity in healthy
volunteers. Int J Neuropsychopharmacol
2005;8(2):255-9
170. Hallam KT, Olver JS, Norman TR.
Effect of sodium valproate on nocturnal
melatonin sensitivity to light in healthy
16
volunteers. Neuropsychopharmacology
2005;30(7):1400-4
171. Castro LMR, Gallant M, Niles LP.
Novel targets for valproic acid: upregulation of melatonin receptors and
neurotrophic factors in C6 glioma cells.
J Neurochem 2005;95(5):1227-36
172. Ogden CA, Rich ME, Schork NJ, et al.
Candidate genes, pathways and
mechanisms for bipolar (manicdepressive) and related disorders:
an expanded convergent functional
genomics approach. Mol Psychiatry
2004;9(11):1007-29
173. Leibenluft E, Feldman-Naim S,
Turner EH, et al. Effects of exogenous
melatonin administration and withdrawal
in five patients with rapid-cycling bipolar
disorder. J Clin Psychiatry
1997;58(9):383-8
174. Robertson JM, Tanguay PE. Case study:
the use of melatonin in a boy with
refractory bipolar disorder. J Am Acad
Child Adolesc Psychiatry
1997;36(6):822-5
175. Bersani G, Garavini A. Melatonin addon in manic patients with treatment
resistant insomnia.
Prog Neuropsychopharmacol
Biol Psychiatry 2000;24(2):185-91
176. Nierenberg AA. Low-dose buspirone,
melatonin and low-dose bupropion
added to mood stabilizers for severe
treatment-resistant bipolar depression.
Psychother Psychosom 2009;78(6):391-3
177. Norris ER, Karen Burke Correll JR,
et al. A double-blind, randomized,
placebo-controlled trial of adjunctive
ramelteon for the treatment of insomnia
and mood stability in patients with
euthymic bipolar disorder.
J Affect Disord 2013;144(1-2):141-7
178. De Bodinat C, Guardiola-Lemaitre B,
Mocaër E, et al. Agomelatine, the first
melatonergic antidepressant: discovery,
characterization and development.
Nat Rev Drug Discov 2010;9(8):628-42
179. Calabrese JR, Guelfi JD,
Perdrizet-Chevallier C; Agomelatine
Bipolar Study Group. Agomelatine
adjunctive therapy for acute bipolar
depression: preliminary open data.
Bipolar Disord 2007;9(6):628-35
180. Eppel AB. Agomelatine adjunctive
therapy for acute bipolar depression:
preliminary open data. Bipolar Disord
2008;10(6):749-50; author reply 750-1
Expert Opin. Ther. Targets (2015) 19(6)
181. Fornaro M, McCarthy MJ,
De Berardis D, et al. Adjunctive
agomelatine therapy in the treatment of
acute bipolar II depression: a preliminary
open label study.
Neuropsychiatr Dis Treat 2013;9:243-51
182. Boudebesse C, Geoffroy PA, Bellivier F,
et al. Correlations between objective and
subjective sleep and circadian markers in
bipolar disorder. Chronobiol Int
2014;31(5):698-704
.
Study demonstrating good correlation
between some subjective and objective
sleep and circadian measures.
183. Ng TH, Chung K-F, Ho FY, et al.
Sleep-wake disturbance in interepisode
bipolar disorder and high-risk
individuals: A systematic review and
meta-analysis. Sleep Med Rev
2014;20C:46-58
.
Interesting review and meta-analyses
about several aspects of sleep
disturbances in remitted BD.
184. Bauer M, Grof P, Gyulai L, et al. Using
technology to improve longitudinal
studies: self-reporting with
ChronoRecord in bipolar disorder.
Bipolar Disord 2004;6(1):67-74
185. Bauer M, Glenn T, Grof P, et al.
Self-reported data from patients with
bipolar disorder: frequency of brief
depression. J Affect Disord
2007;101(1-3):227-33
186. Glenn T, Monteith S. New measures of
mental state and behavior based on data
collected from sensors, smartphones, and
the Internet. Curr Psychiatry Rep
2014;16(12):523
187. Darwent D, Zhou X, van den Heuvel C,
et al. The validity of temperaturesensitive ingestible capsules for measuring
core body temperature in laboratory
protocols. Chronobiol Int
2011;28(8):719-26
188. McCarthy MJ, Wei H, Marnoy Z, et al.
Genetic and clinical factors predict
lithium’s effects on PER2 gene
expression rhythms in cells from bipolar
disorder patients. Transl Psychiatry
2013;3:e318
189. Xiao Y, Camarillo C, Ping Y, et al. The
DNA methylome and transcriptome of
different brain regions in schizophrenia
and bipolar disorder. PLoS One
2014;9(4):e95875
190. Akula N, Barb J, Jiang X, et al.
RNA-sequencing of the brain
transcriptome implicates dysregulation of
Sleep- and circadian rhythm--associated pathways as therapeutic targets in bipolar disorder
neuroplasticity, circadian rhythms and
GTPase binding in bipolar disorder.
Mol Psychiatry 2014;19(11):
1179-85
191.
Expert Opin. Ther. Targets Downloaded from informahealthcare.com by INSERM on 03/03/15
For personal use only.
192.
193.
194.
Van Enkhuizen J, Minassian A,
Young JW. Further evidence for
Clockdelta19 mice as a model for bipolar
disorder mania using cross-species tests of
exploration and sensorimotor gating.
Behav Brain Res 2013;249:44-54
McClung CA. Circadian rhythms and
mood regulation: insights from preclinical models.
Eur Neuropsychopharmacol
2011;21(Suppl 4):S683-93
Jung SH, Park J-M, Moon E, et al.
Delay in the recovery of normal sleepwake cycle after disruption of the lightdark cycle in mice: a bipolar disorderprone animal model? Psychiatry Investig
2014;11(4):487-91
Chen Z, Yoo S-H, Park Y-S, et al.
Identification of diverse modulators of
central and peripheral circadian clocks by
high-throughput chemical screening.
Proc Natl Acad Sci USA
2012;109(1):101-6
195.
Chun SK, Jang J, Chung S, et al.
Identification and validation of
cryptochrome inhibitors that modulate
the molecular circadian clock.
ACS Chem Biol 2014;9(3):
703-10
196.
Kozikowski AP, Gunosewoyo H, Guo S,
et al. Identification of a glycogen
synthase kinase-3beta inhibitor that
attenuates hyperactivity in CLOCK
mutant mice. ChemMedChem
2011;6(9):1593-602
197.
Rybakowski JK, Dmitrzak-Weglar M,
Kliwicki S, et al. Polymorphism of
circadian clock genes and prophylactic
lithium response. Bipolar Disord
2014;16(2):151-8
198.
Leise TL. Wavelet analysis of circadian
and ultradian behavioral rhythms.
J Circadian Rhythms 2013;11(1):5
199.
May M. Life science technologies: Big
biological impacts from big data. Science
2014;344:1298-300.
doi: 10.1126/science.344.6189.1298
Expert Opin. Ther. Targets (2015) 19(6)
Affiliation
Frank Bellivier†1,2,3,4, MD PhD,
Pierre-Alexis Geoffroy1,2,3,4, MD,
Bruno Etain4,5,6 MD PhD &
Jan Scott7,8 MBBS PhD
†
Author for correspondence
1
Inserm, U1144, Paris, F-75006, France
2
Universite Paris Diderot, UMR-S 1144, Paris,
F-75013, France
3
AP-HP, GH Saint-Louis - Lariboisière - Fernand
Widal, Pôle Neurosciences, 75475 Paris
Cedex 10, France
Tel: +33 1 40 05 48 69;
Fax: +33 1 40 05 49 33;
E-mail: frank.bellivier@inserm.fr
4
Fondation FondaMental, Creteil, 94000, France
5
INSERM, Unite 955, IMRB, Equipe de
Psychiatrie Genetique, Creteil, F-94000, France
6
AP-HP, Hopitaux Universitaires Henri Mondor,
DHU PePsy, Pôle de Psychiatrie, Creteil,
F-94000, France
7
Newcastle University, Institute of Neuroscience,
Academic Psychiatry, Newcastle, UK
8
Institute of Psychiatry, Centre for Affective
Disorders, London, UK
17