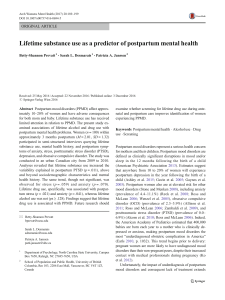
Postpartum Complications CH 21 Julie Vavrek MSN, BA, RN, CPNP Postpartum Hemorrhage Leading cause of maternal death worldwide PPH traditionally defined as loss of more than: •500 ml of blood after vaginal birth •1000 ml after cesarean birth Life-threatening with little warning Often unrecognized until profound symptoms Etiology and Risk Factors Uterine atony •Marked hypotonia of uterus Lacerations of genital tract Hematomas Retained placenta •Nonadherent retained placenta •Adherent retained placenta Inversion and Subinvolution Inversion of uterus •Turning inside out of uterus •Potentially life threatening •1 in 3000 births Subinvolution of uterus •Late postpartum bleeding •Retained placental fragment and pelvic infection Medical Management Early recognition is critical •Evaluate of contractility of uterus Firm massage of fundus Management is directed toward increasing contractility and minimizing blood loss Medications Nursing interventions Hemorrhagic (Hypovolemic) Shock Medical management Nursing interventions Fluid or blood replacement therapy *Legal– standard of care for bleeding emergencies allows for provisions to be made for nurses to initiate actions independently Coagulopathies Idiopathic thrombocytopenic purpura (ITP) von Willebrand disease—type of hemophilia Disseminated intravascular coagulation -Consumptive coagulopathy -Consumes large amounts of clotting factors -Widespread external bleeding, internal bleeding, or both Thromboembolic Disorders Results from blood clot caused by inflammation or partial obstruction of vessel Superficial venous thrombosis Deep venous thrombosis Pulmonary embolism Incidence and etiology Clinical manifestations Medical management Nursing interventions Postpartum Infections Puerperal infection: any infection of genital tract within 28 days after miscarriage, induced abortion, or birth Most common infecting agents are numerous streptococcal and anaerobic organisms Endometritis Wound infections Urinary tract infections Mastitis Perinatal Mood Disorders A set of mood disorders that occur any time during pregnancy or the first year postpartum •Depression •Anxiety •OCD •PTSD •Postpartum psychosis Depression Depression during pregnancy is a major risk factor for PPD Maternal suicide •20% of postpartum deaths Negatively affects infant’s cognitive, neurologic, and motor skill development Affect the well-being of the mother, baby, and family Can interfere with attachment Baby Blues Up to 85% of women experience a ”mild depression” Functioning is not impaired Mood swings, sadness, crying, difficulty sleeping, loss of appetite Symptoms resolve in a few days Postpartum Depression Onset in pregnancy or within 4 weeks of birth Hormone fluctuations, nutritional deficiencies (folate, B12) Risks •History of anxiety or depression •Younger age •Unintended pregnancy •Family history •Unmarried, lack of social support •Lower education Paternal Postpartum Depression 10-50% of fathers experience PPD as well Partner with PPD major risk factor Fatigue, frustration, anger irritable withdrawn Treatment Early recognition of symptoms Education Screening Referrals Provide safety Psychiatric hospitalization Medications Medications for non-lactating •TCAs, SSRIs, SNRIs, MAOIs, mood stabilizers, antipsychotics •Educate about side effects •Lithium is not used with breastfeeding Medications for lactating •Benefits outweigh risks •Avoid feeding during peak medication times •SSRIs used most commonly – Paxil, Zoloft, Pamelor •Do pass through milk but no untoward effects to baby Monitor infant for irritability, poor feeding, altered sleep Loss and Grief Situational life crises superimposed on childbearing •Infertility •Premature labor or birth •Cesarean birth •Gender of infant not desired •Birth of child with handicap •Maternal death • Fetal or neonatal death