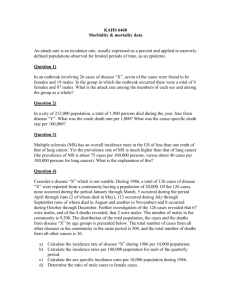
THE LITERATURE OF MEDICINE Medical Usage and Abusage: "Prevalence" and "Incidence" GARY D. FRIEDMAN, M.D., S.M. in Hyg., F.A.C.P., Oakland, California In view of the frequent misuse of the term "incidence/' the concepts of incidence, prevalence, and period prevalence are defined and illustrated. The importance of restricting "incidence" to the rate of development of new events in a population or a group of patients, per unit of time, is stressed. Clearly distinguishing incidence from prevalence or simple proportion can help both in the understanding and the communication of findings in patient groups. I T HAS BEEN SAID that the easiest way to distinguish a clinician from an epidemiologist is by the clinician's incorrect use of the term "incidence." Ignoring the highly useful distinction between the concepts described by "prevalence" and "incidence" is, however, not restricted to clinicians. A forceful example of this problem came to me in a set of galley proofs from the Annals of Internal Medicine. The copy editor had changed "prevalence" to "incidence" wherever it appeared in the paper. Thus, even this presumed expert in grammar and usage, whose job is to make sure that physician-authors use the English language correctly and effectively, had erred about "incidence." This copy editor may have read too many clinical manuscripts with misuse of "incidence." Soon after this occurred, Dr. Huth, the Editor, asked me to write a brief note reviewing the correct definitions of these measures of relative frequency. After some years of reading thousands of manuscripts, he had concluded that the imprecise use of "incidence" and "prevalence" was probably the most frequent error in vocabulary among physician-authors, although it might be rivaled by confusion between "case" and "patient." Apparently the repeated presentation of these concepts in courses in preventive medicine and the pleas by epidemiologists and an expert World Health Organization committee (1) have not had much effect. To verify this impression, I sampled the use of "incidence" in the latest edition of a widely used textbook of medicine. On every tenth page I looked for subsections headed "Incidence" or "Prevalence" in relation to specific diseases. Within the six subsections found, "incidence" was • From the Department of Medical Methods Research, Kaiser-Permanente Medical Care Program, Oakland, California. 502 Downloaded From: https://annals.org/ by a University of Texas User on 10/12/2018 used correctly in one, was used probably to mean prevalence in one, was used to mean proportion of hospital admissions in one, and was not used in the text in the other three. Where "incidence" was not used in the text, its use in the subheading seemed to refer to a discussion of some aspects of the distribution of occurrence of the disease in the population—for example, "occurs at any age" or "is common in most wars." In epidemiology, "incidence" has a very specific meaning, pertaining to the development of new cases of a disease in a population free of the disease. Thus, an incidence rate is the fraction of the population at risk who develop or acquire the disease per unit of time (hours, days, months, years, or whatever period is most convenient). Or, put in terms of an equation: Incidence rate = number of new cases of a disease per unit of time total population at risk If a person already has the disease, he should obviously not be included in the denominator population at risk. In contrast to the process of disease development as represented by "incidence," "prevalence" (or "point prevalence") refers to a static picture or "snapshot" of the number of persons who have a disease in a population at one point in time, such as a certain day when a survey is made. This point does not have to be in calendar time but can be at an event in people's lives, such as at birth, or at a special screening examination, or at autopsy, each of which occurs for different members of a population at different points in calendar time. The prevalence rate (sometimes called the prevalence ratio) is merely the number of persons with the disease divided by the number in the population under consideration. It is a simple fraction or proportion: number of existing cases Prevalence rate = ——: =—; It may not be strictly correct total to refer population to this simple proportion as either a "rate" or a "ratio" but "prevalence rate" seems currently to be the most commonly used term (2). The concept of "period prevalence" is somewhat different. If the ascertainment of existing cases spans a long period, such as a year, the cases detected will include those prevalent at the beginning of the period plus those new "incidence cases" developing during the period. When period prevalence is used, the time period (for example, Annals of Internal Medicine 84:502-504,1976 one year, 10 years) should be specified, for example: all cases existing during the year 1-year period prevalence = — ; ;—: total population If the period is long and the population denominator changes in size during that time it is customary to use the actual or estimated population size at the midpoint of the interval. This applies also to determinations of incidence over long time periods. Now, it so happens that clinicians (and pathologists) have other important groups to talk about beside populations, which are the chief concern of the epidemiologist. Examples of such groups may be patients with a particular disease, or patients treated with a certain drug, or all persons seen in a clinic during a certain year, or patients who come to the emergency room on Monday mornings, or all patients in a particular hospital who had postmortem examinations in the past 20 years. In describing such groups it is frequently desired to refer to a proportion or fraction who have a particular characteristic, who developed it over a period of time or who are going to develop it in the future. Here, the indiscriminate use of the word "incidence" in referring to all these proportions is inappropriate. It would be helpful to the clinician to adopt the epidemiologist's distinction and reserve "incidence" for the rate of development per unit of time and "prevalence" for describing that fraction of the group with the characteristic at a particular point in time. Let us apply these concepts to a clinical situation. Suppose a physician has been following up 150 women with asymptomatic bacteriuria detected during a health checkup. He first obtained further information and ordered additional studies on these women. Forty had had previous episodes of symptomatic cystitis. Intravenous pyelography showed that 20 women had congenital anomalies of the urinary tract, such as double ureters. Creatinine clearance tests showed that 10 women (including 5 of those with urinary tract anomalies) had normally low values. For simplicity let us assume that all women were not treated initially but were carefully followed up at regular intervals for 2 years to assess the development of complications and changes in renal function. During the 2 years, 30 women had one or more episodes of frank symptomatic urinary tract infection, which were treated. There were 40 episodes in all—1 each among 20 of the women and 2 each among the other 10. At the end of the 2 years, abnormally low creatinine clearance values were found in 15 women. Of those, 8 were among the 10 with low values originally, and 7 were previously normal. Two of the 10 with low values originally were now normal. With the present widespread indiscriminate use of "incidence," this physician in reporting his findings at a conference is likely to stand up and state that, "Among this group of women with asymptomatic bacteriuria, the incidence of congenital anomalies of the urinary tract was . . . and so forth and so on." How should these data be summarized? Table 1 shows how these observations can be described, the numbers to be used, and correct terminology for the findings. Even though prevalence or incidence is being presented, it is not always necessary to use either term. As will be seen in some of the examples in Table 1, it may be simpler and less clumsy to refer merely to a fraction, proportion, percentage, or a rate that is explicitly described. If, as often happens, follow-up durations for members of a study group are not the same, the investigator can take advantage of all available follow-up data and compute incidence rates using person-years or person-months in the denominator instead of persons ( 3 ) . It should be stressed that the time unit is an essential component of the incidence rate. Without specification of the time period covered the use of "incidence" to refer merely to a fraction of patients who develop an episode or finding has little meaning and can be quite misleading. For example, a paper on implantation of prosthetic cardiac valves may report this observation: "Among patients who survived through the first 2 postoperative weeks, the incidence of bacterial endocarditis was 2 % . " Without a statement as to the time through which this observation was made, we cannot evaluate this rate or compare it to the findings of others. Two cases of endocarditis per hundred patients in 2 months would be a relatively high incidence rate—12 cases per hundred patients per year, on an annual basis; whereas 2 cases per hundred patients in 2 years would be a relatively low incidence rate—only 1 case per hundred per year. If it is necessary to report such clinical observations without reference to a period of time the facts should be stated simply without using the word "incidence," to avoid implying that a rate per unit of time has actually been measured. A more accurate version of the above statement would be: "Among patients who survived through the first 2 postoperative weeks, 2 % later developed bacterial endocarditis." If an author or speaker would make careful distinctions among "incidence," "prevalence," and related measures of relative frequency, this would not only improve communiction with others, but would help assure his own full understanding of exactly what it is he is trying to say. ACKNOWLEDGMENTS: Received 26 September 1975; revision accepted 12 January 1976. • Requests for reprints should be addressed to Gary D. Friedman, M.D., 3779 Piedmont Avenue, Oakland, CA 94611. References 1. Terminology and nomenclature: prevalence and incidence. Bull WHO 35:783-784, 1966 2. ELANDT-JOHNSON RC: Definitions of rates: some remarks on their use and misuse. Am J Epidemiol 102:261-21 \y 1975 3. FRIEDMAN GD: Primer of Epidemiology. New York, McGrawHill, 1974, pp. 107-108, 116 Friedman • Literature of Medicine Downloaded From: https://annals.org/ by a University of Texas User on 10/12/2018 503 Table 1 . Measurements of Relative Frequency from the Hypothetical Study of Women with Asymptomatic Bacteriuria Described in Text Type of Measurement Numbers to be Used Past history of cystitis Prevalence 40 with positive history _ Q 27 o r 21°/ 150 women Twenty-seven percent gave a history of symptomatic cystitis. Congenital urinary anomalies Prevalence 20 with anomalies n . . -~ — = 0.13 or 13% 150 women The prevalence of congenital anomalies was 13%. Or 13% had congenital anomalies. Diminished renal function initially among all the women Prevalence 10 with low creatinine The prevalence of abnormally low creatinine clearance was 7%. Or 7% had abnormally low creatinine clearance. Diminished renal function initially among women without congenital anomalies Prevalence Women developing symptomatic urinary tract infection Incidence Development of episodes of symptomatic urinary tract infection Incidence 40 episodes . —^ in 2 years 150 women = 27 episodes/100 women in 2 years or 13.5/100 per year The incidence of episodes of urinary tract infection was 13.5 episodes per 100 women per year. (Note that episodes are not a fraction or proportion of women and that there can be more episodes than women.) Development of diminished renal function Incidence 7 women with normal creatinine clearance initially and low values at the end of follow-up 140 women with normal creatinine clearance initially (and at risk for developing a low value) Among women with normal renal function initially, the incidence of abnormally low renal function was 5% in 2 years or 2.5% per year. Area of Concern clearance Suitable Description of Results 0.07 or 7% 150 women 5 with low creatinine clearance and without congenital anomalies 130 women without congenital anomalies 30 women developing 1 or more episodes 150 women = 0 04 0 r 4 ^ „ —u.z or MV ye m 2 years or 10% per year Of the women with asymptomatic bacteriuria and no congenital anomalies, 4% had low creatinine clearance. One or more episodes of symptomatic urinary tract infection occurred in 20% of the women in the 2-year period for an incidence rate of 10% per year. — 0.05 or 5% in 2 years or 2.5% per year Improvement of diminished renal function to normal Incidence 2 women with low creatinine clearance initially and normal values at the end of follow-up 10 women with low creatinine clearance initially (and at risk for developing a. normal value) - 0.2 or 20% in 2 years or 10% per year Of the women with diminished renal function initially, 20% improved to normal levels in 2 years. The rate of return to normal was 10% per year. Presence of diminished renal function at any time during the 2-year period Period prevalence 17 women with low creatinine clearance (10 initially plus Of all the women, 11% showed evidence of diminished renal function at some time during the 2-year period. ,7newcases) 150 women 0.11 or 11% (Note that this cannot be divided by two to give the 1-year period prevalence because the prevalence at the beginning of the period was already 7%.) 504 Apr//1976 • Annals of Internal Medicine • Volume 84 • Number 4 Downloaded From: https://annals.org/ by a University of Texas User on 10/12/2018