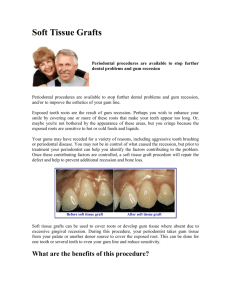
Gingival Recessions Definition Gingival recession is defined as the displacement of marginal gingiva apical to the cementoenamel junction (CEJ); thereby exposing the root surface to the oral environmentwhich causes poor esthetic appearance and in some cases root hypersensitivity.The distance between the CEJ and gingival margin gives the level of recession. It can occur in patients with good standards of oral hygiene as well as those with poor oral hygiene and periodontal disease. Recession may also be associated with cervical lesions such as abrasive class V cavities or root caries.Gingival recession along with the inadequate width of attached gingiva and inadequate vestibular depth are very common clinical finding in the front region of the lower jaw. Prevalence of Recessions The prevalence of gingival recession has been shown to increase with age.According to the US National Survey, 88% of seniors (age 65 and over) and 50% of adults (18 to 64) present recession in one or more sites; progressive increase in frequency and extent of recession is observed with increase in age. In the younger age cohort (30 to 39 years), the prevalence of recession was 37.8%. Etiology of Recession For decades, it was believed that gingival recession was a part of human aging processes; however, there is not strong evidence supporting such a statement. Aging might increase the possibility for the causes of gingival recession to act, but that does not mean they are inherent to aging. One of the main reason of gingival recession is resorption of underlying alveolar bone. Over timein lack of support, normal or inflamed gingival soft tissues tend to keep up with cervical bone levels; therefore, gingival recession is established. The etiology of recessions is multifactorial. Factors are below; one or more factor may be presented: Aggressive tooth brushing Periodontal disease and periodontal treatment Occlusal trauma Iatrogenic damage Aberrant frenal attachments Aggressive tooth brushing.It is known that inappropriate daily brushing may physically wounds gingival tissues. Traumatically using the toothbrush as well as other oral hygiene agents over delicate gingival margins on a daily basis might gradually and slowly lead to gingival recession over the years. In general, those cases are presented in combination with cervical wear as a result of abrasion caused by the same agents. Periodontal disease and periodontal treatment. Tissue destruction resulting from periodontal disease encompasses gradual bone loss which might lead to apical gingival migration and root exposure. At first, tissue loss is apparently compensated by gingival swelling. After periodontal treatment swelling decreases and retraction of gingival tissue volume occurs. Thus, root will become exposed to the oral environment, which esthetically, might be considered strange by the patient, even though periodontal tissues are perfectly healthy at this point. Ideally patient should be informed about this fact before periodontal treatment. Occlusal trauma. Due to the increase in functional demand, alveolar bone resorption may occur. In those cases, vertical bone loss is radiographically noticeable. On buccal surface, depending on cortical plate thickness, vertical bone loss results in bone dehiscence over the affected root - a Vshaped cavity in the bone contour, thereby gingival bone support decreases. Gingival contour will keep up with buccal bone contour, which results in V-shaped or angled gingival recession in teeth affected by occlusal trauma and bone dehiscence. It should be once again highlighted that this process is not associated with local dental plaque buildup and consequent chronic inflammatory periodontal disease. Iatrogenic damage caused by: 1. Restorative treatmentmay be a reason of recession. Restorative treatment, which involves placement of subgingival margins of restorations, can directly impinge on the biologic width. To re-establish the biologic width there may be some bone loss and apical migration of the gingival tissues. Subgingival restoration margins increase the plaque accumulation, gingival inflammation, and alveolar bone loss.Crowns, veneers and Class V restorations should have enough prominence of vestibular contour to prevent trauma of gingiva by food, such trauma also may cause recession. 2. Orthodontic treatment. Orthodontic tooth movement should not be considered as the primary cause of gingival recession. Induced tooth movement does not cause any damage to gingival tissues; however, during orthodontic treatment, the following might occur in a few patients. In those cases, before gingival recession occurs, orthodontic movement had induced dehiscence at the bone crest, as a result of moving a tooth towards an area with extremely thin bone. Induced tooth movement should be carried out only at the alveolar bone trabeculae space; however, during certain types of movement, teeth are also displaced at the expenses of the outer cortical plate. In such cases dehiscence and fenestration may occur. The latter are defects found in the outer cortical plate and act as "predisposing factors" of gingival retraction. A potential means to avoid dehiscence and recession during orthodontic treatment is to apply light, well-balanced forces to sets of teeth rather than to a single tooth. Movement should be carefully planned 3. Aberrant frenal attachments have been mentioned as a cause of recession due to an apical pull on the gingival tissues.Also high frenal attachments (close to the gingival margin) may make oral hygiene difficult therefore leading to a localized periodontal problem and subsequent recession. Abberant frenal attachment Short thick frenula of a lip in oral vestibule cause local trauma of soft tissues because of mechanical pulling gingiva out from teeth and alveolar bone during speaking and chewing. It cause ischemia of area of frenula attachment and may lead to encroach on the marginal gingiva, pull the gingival sulcus, fostering plaque accumulation, bone resorption, gingival recessions and diastema. These are actual also for buccal frenula. Classification of Recessions Various classifications have been proposed to classify gingival recession. 1. According to distribution: Localized Generalized or horizontal form is associated with chronic inflammatory destructive periodontal disease. Loss of periodontal support in proximal areas results in apical displacement of gingiva, including interdental papillae. 2. According to shape: V–shaped recession is associated with teeth subjected to occlusal trauma, especially in patients with bruxism and clenching habits. In cases of severe apical migration, V-shaped recession is known as Stillman's cleft. At the corresponding enamel, it is common to find abfraction; while on the occlusal surface, wear facets caused by attrition are commonly found, as being part of a lesion caused by occlusal trauma. U–shaped recession is generally associated with chronic inflammatory periodontal disease, inadequate tooth brushing or inadequate frenulum insertion. U-shaped gingival recession associated with inadequate traumatic brushing is surrounded by healthy gingiva and is usually associated with abrasion, with a smooth, polished surface. There are cases of U-shaped recession in which the area of root exposure is surrounded by a peripheral festoon made up of swollen, inflamed gingival tissue resulting from local dental plaque buildup. A few classical studies found in Periodontology literature refer to the aforementioned condition as McCall's festoon. 3. According to loss of attached tissue: with loss of dentogingival junction and attached tissue (e.g. in case of periodontal diseases) without loss of dentogingival junction and attached tissue (e.g. in case of occlusal trauma) 4. One of the most widely followed classification is Miller's classification (proposed in 1985) of gingival recession. Miller has primarily based his classification on following aspects: Extent of gingival recession defects Extent of hard and soft tissue loss in interdental areas surrounding the gingival recession defects. Miller’s classification is useful in predicting the final amount of root coverage following a free gingival graft procedure. Miller’s Classification of Recessions Class I (Fig. 1): Recession does not extend to the mucogingival junction (MGJ). There is no periodontal loss (bone or soft tissue) in the interdental area, and 100% root coverage can be anticipated. Figure 1. Recession Class I by Miller, MGJ – mucogingival junction Class II (Fig. 2): Recession extends to or beyond the MGJ. There is no periodontal loss (bone or soft tissue) in the interdental area, and 100% root coverage can be anticipated. A B Figure 2. (A) Scheme of recessions Class II by Miller; (B) Clinical view of wide multiple recessions Class II by Miller. MGJ – mucogingival junction Class III (Fig. 3): Recession extends to or beyond the MGJ. Bone or soft tissue loss in the interdental area is present or there is a malpositioning of the teeth, which prevents the attempting of 100% of root coverage. Partial root coverage can be anticipated. A B Figure 3. Scheme of recessions Class III by Miller: recession extends beyond the mucogingival junction (MGJ), bone or soft tissue loss in the interdental area is present (A) or there is a malpositioning of the teeth (B) Class IV (Fig. 4): Recession extends to or beyond the MGJ. The bone or soft tissue loss in the interdental area and/or malpositioning of teeth is so severe that root coverage cannot be anticipated. A B С Figure 4. Gingival recessions class IV by Miller (A) scheme, MGJ – mucogingival junction; (B)intraoral view of vestibular surfaces; (C)view of lingual surfaces of lower frontal teeth Complaints Patients tend to present with three main concerns, which are poor aesthetics, worry about potential tooth loss and dentine hypersensitivity due to the exposed root surface following gingival recession. Clinical Features The following clinical parameters should be taking to examine a recession at the mid-buccal aspect of tooth with recession: Probing pocket depth (PD) was measured with a standard periodontal probe to the nearest millimeter from the gingival margin to the bottom of sulcus Clinical attachment level (CAL) was measured from the cemento-enamel junction (CEJ) to the bottom of the sulcus Recession depth (RD) measured from CEJ to the gingival margin Recession width (RW) measured across the buccal surface at the CEJ level The width of keratinized gingiva (WKG). Gingival recession may be accompanied with cervical caries (Fig. 5), erosions, wedge-shaped defects. Figure 5. Recessions and cervical caries in teeth 13,14, before filling (left) and after filling (right) Treatment of Gingival Recessions First aim for treatment of recessions is to reveal and to remove etiological factors to control progression.Recessions do not require treatment if: they are not large and do not progress esthetic concerns not a problem for patient hypersensetivity of exposed roots is controlled with desensitizers or absent There are surgical and non-surgical methods for recession treatment. 1.Non-surgical methods: Crowns, veneers, restoration. Crowns may be placed to widen the clinical crown which may camouflage the exposed root surface Construction of gingival mask. Patients who have several teeth with recession may have unaesthetic appearance because of black triangles. In these cases, where surgical procedure is not appropriate, silicone flexible gingival veneer or mask may be used. Application of desensitizers on exposed roots. 2. Surgical methods. Surgical methods of recession treatment are among of mucogingival surgery procedures. Aim of surgical methods is to close exposed root surface with either graft or flap to repair esthetic and decrease root hypersensitivity. Mucogingival Surgery Terminology and Definition The term mucogingival surgery was initially introduced in the literature by Friedman (1957). It is applied to surgical procedures utilized to resolve problems involving the interrelationship between gingiva and alveolar mucosa with reference to next problems: increasing of width and thickness of attached gingiva gingival recessions shallow vestibule aberrant frenal attachment. This term is distinguished from periodontal surgery wherein alveolar mucosa is not handle. With the advancement of periodontal surgical techniques, the scope of non-pocket surgical procedures has increased, now encompassing a multitude of areas that were not addressed in the past. Recognizing this, the 1996 World Workshop in Clinical Periodontics renamed mucogingival surgery as periodontal plastic surgery, a term originally proposed by Miller in 1993. Periodontal plastic surgery is defined as the surgical procedures performed to correct or eliminate anatomic, developmental, or traumatic deformities of the gingiva or alveolar mucosa. Several surgical techniques have been developed for the management of shallow vestibule, gingival recession, the inadequate width of attached gingiva and aberrant frenal attachment which set out mucogingival problems. Mucogingival Surgery Procedures There are many modifications of mucogingival surgical procedures; the basic procedures are: Free gingival graft Connective tissue graft Coronally advanced flap Pedicle flap Deepen of vestibule Frenectomy Guided tissue regeneration for root coverage Preparation of the exposed root surface. Before any surgical technique root surfaces are mechanically prepared prior to any mucogingival procedure to allow biological attachment of the grafted tissue to it. The root surface is thoroughly debrided and irrigated with sterile saline. At the day of surgery the site should presented a healthy periodontium with the gingiva exhibiting no evidence of bleeding on probing. If the plan is to obtain root coverage over existing caries or class V restoration, the caries and restoration must be completely removed (gingiva will not attach to artificial restorative material). Significant convexity of the root may be reduced with diamond burs on high speed.Historically, chemical root surface modifiers such as citric acid, tetracycline, or EDTA had been used to demineralize and decontaminate the root surface to expose the collagen fibers. The theory is this will facilitate attachment of gingival fibers to the root surface. However, recent evidence demonstrates that the use of these chemical modifiers provides no benefit of clinical significance. Postoperative care are the same for all types of mucogingival surgical procedures. Immediately following surgery, use of icepacks was recommended intermittently for three hours. The patient is advised not to brush the treated site for 2 weeks. After 1 week toothbrushing of treated site should be carried out gently with ultrasoft toothbrush. 0.12% chlorhexidine mouth rinse is prescribed twice a day for 2 weeks. Systemic antibiotics were prescribed (Amoxicillin-500 mg, three times daily for five days) along with analgesics. Sutures should be removed 7-10 days after surgery. Patient should be examined weekly for the 1st month. Free Gingival Graft Free gingival graft is soft tissue graft comprising epithelium and thin layer of underlying connective tissue that are completely detached from one site (donor site) and transferred to a remote site (recipient site). Most common donor site for free gingival graft is hard palate. The palatal masticatory mucosa is widely used as a connective tissue donor site in gingival recession treatment. However, concern has been raised regarding the potential risk of damaging the greater palatine artery during harvesting of graft due to anatomical variations in the palatal vault. This technique allows: 1. To increase the zone of attached gingiva 2. To augment the thickness of attached gingiva 3. To repair gingival recession Free gingival graft technique: 1. Preparation of the recipient bed.The recipient site should beprepared as split-thickness flap (periosteum should not be detached from bone) and extend at least 3 mm laterally and apically to the recession defect, as this will be the only nutrient supply to the graft during the initial healing phase. Any muscle or frenal insertions should be removed by sharp dissection to ensure that the graft lies passively with no movement occurring during function. 2. Harvesting of the graft. Graft should be harvested from donor site and the size should be adapted. Proper thickness 1.0–1.5 mm is an important factor for survival of the graft because nutrition of graft first time after surgery will be due to diffusion of nutrients from the recipient site. If graft is too thick, central part will not have enough nutrition and will become necrotic. Good adaptation of the graft to the recipient site is essential for adequate diffusion, so care must be taken on preparing the recipient site the graft to the exact same size to ensure a good fit. 3. Transfer and suturing of the graft.Graft is applied on recipient site, sutured into position and pressed by finger for several minutes for better adaptation. Connective Tissue Graft The connective tissue autograft technique was originally described by Edel and is based on the fact that the connective tissue carries the genetic message for the overlying epithelium to become keratinized.Therefore only connective tissue from beneath a keratinized zone can be used as a graft. The Connective Tissue Graft (CTG) technique is considered as the gold standard in the management of recession defects. It is also used in combination with coronally advanced flap. Terminology: connective tissue graft = free connective tissue graft = subepithelial connective tissue graft. The free connective tissue graft (CTG) is differ with the free gingival graft is that the donor tissue is connective tissue only with no epithelium on it. Donor site may be hard palate, tuber of maxilla, retromolar region. Advantages: double blood supply of graft at the recipient site from the underlying connective tissue base and the overlying recipient flap. donor site is a closed wound, which produces less postoperative discomfort excellent color blend can be achieved Minimal palatal denudation, less invasive, less prone to hemorrhage, more rapid healing. The connective tissue graft results in two sutured closed wound sites, while the free gingival graft results in two open exposed wounds. Free connective tissue graft technique: 1. Preparation of the recipient bed. The recipient bed is prepared to accommodate the connective tissue graft. Divergent vertical incisions are made at the line angles of the tooth to be covered. A split thickness flap is performed where the periosteum remains attached to the underlyingbone. The split thickness flap is prepared by sharp dissection and the presence of any muscle fibers or attachment is eliminated. The flap should be mobile so that it can be repositioned to at least 5 mm apical to the receded area.Suture the apical mucosal border to the periosteum using a gut suture. 2. Harvesting of the graft.The connective tissue graft is harvested from the hard palate. The ideal location is 5–6 mm apical to the gingival margin of the palatal aspects of the maxillary premolars and the mesial half of the maxillary first molar. The ideal thickness of the graft should be 1–1.5 mm thick. The donor site is sutured after the graft is removed.During harvesting the connective tissue, the vital structure that needs to be avoided is the greater palatine artery. Depending on the depth of the palatal vault, typically, the artery is about 12 mm apical to the gingival margin. 3. Transfer and suturingof the graft.The harvested connective tissue graft is immediately placed in the recipient site and secure into position with sutures to the periosteum. Good stability of the graft must be attained with adequate sutures. Optimized healing requires the graft to be in intimate contact with the recipient bed with the absence of any dead space. 6. Covering of the graft. Cover the grafted site with dry aluminum foil and periodontal dressing. Coronal Advanced Flap The coronally advanced flap is commonly used to treat the Miller Classes I and II recession defects.Various modifications of the coronally advanced flap (CAF) have been proposed with the attempt of treating gingival recession. Coronal advanced flap technique: 1. Horizontal and vertical incisions. Make a horizontal internal bevel incision from the gingival margin to the bottom of the pocket to eliminate the diseased pocket wall. It is made at the recession and extended with two vertical releasing incision in correspondence to the line angles. Vertical incisions should go beyond the mucogingival junction. 2. Management of papilla. The interdental papilla is preserved as much as possible. Their facial portion is deepithelialized to create a connective tissue bed. 3. Flap elevation. Full thickness flap is elevated. Horizontal incision in periosteum is placed at the base of the flap to ensure tension free coronal displacement of the flap. 4. Flap repositioning. The flap is then coronally positioned to completely cover the defect and secured using continuous sling suture. 5. Suturing of vertical incisions. Vertical releasing incisions are secured using interrupted suture technique. Pedicle Flap There are many variations of pedicle flap, one of them laterally displaced pedicle flap. The laterally positioned flap can be used to cover isolated, denuded root surfaces that have adequate donor tissue laterally, adjacent to the gingival recession. Laterally displaced pedicle flap technique 1. Preparation of the recipient site. Epithelium is removed around the denuded root surface. The exposed connective tissue will be the recipient site for the laterally displaced flap. The root surface will be thoroughly scaled and root planed. 2. Preparation of the flap. The periodontium of the donor site should have a satisfactory width of attached gingiva and minimal loss of bone, without dehiscence or fenestration. A partialthickness flap is used. Prepare vertical incision from the gingival margin to outline a flap adjacent to the recipient site. Extend the incision into the oral mucosa to the level of the base of the recipient site. The flap should be sufficiently wider than the recipient site to cover the root and provide a broad margin for attachment to the connective tissue border around the root. Separate a flap consisting of epithelium and a thin layer of connective tissue, leaving the periosteum on the bone. A releasing incision is sometimes needed to avoid tension on the base of the flap, 3.Transfer the flap. Slide the flap laterally onto the adjacent root, making sure that it lies flat and firm without excess tension on the base. 4. Suturing of a flap.Fix the flap to the adjacent gingiva and alveolar mucosa with interrupted sutures. Deepen the Vestibule Among mucogingival problems, shallow vestibule and gingival recessions which cause an esthetic as well as a functional problem are very common finding in lower front teeth. The presence of adequate vestibular depth is important for both oral hygiene and retention of prosthetic appliances. Numerous surgical techniques have been proposed to accomplish the objective of deepening the vestibule. The aim of this vestibular extension procedure is to increase the depth of vestibule and the width of attached gingival in a single visit. Predictable deepening of the vestibule can only be accomplished by the use of free autogenous graft techniques and their variants. The important clinical aspect in deepening the vestibule is the proper preparation of the recipient site. The recipient site must be covered by immobile periosteal tissue. The donor tissue may be either free gingival or connective tissue, but it must be placed over a nonmobile recipient site. Clinical view of procedure is presented on figure 6. А C B D Figure 6. Deepen the vestibule. (A) shallow vestibule of oral cavity and recessions; (B) incision (C) cutting of muscle and connective tissue strands; (D) clinical view after healing Frenectomy When the recession is caused by frenal pull in those cases, frenectomy is advised. If appropriate hygiene aids do not enable the patient to maintain the area plaque free, then frenectomy is advised to give ease to entrance to the site. Indication to frenectomy: when place a probe to the lowest part of free gingival grooves of central incisors, frenum attachment should be lower than this line showing with the probe. If frenum attachment is above probe line – frenectomy is indicated (Fig. 7). This rule is actual for both upper and lower jaw, but in upper jaw normal frenum attachment should be above probe line. Figure 7. Frenum attachment is a little bit higher than probe line. Guided Tissue Regeneration Technique for Root Coverage Guided tissue regeneration (GTR) should result in reconstruction of the attachment apparatus, along with coverage of the denuded root surface. Guided tissue regeneration technique for root coverage: 1. A full-thickness flap is reflected to the mucogingival junction, continuing as a partialthickness flap 8 mm apical to the mucogingival junction. 2. A resorable membrane is placed over the denuded root surface and the adjacent tissue. It is trimmed and adapted to the root surface and covers at least 2 mm of marginal periosteum. 3. A suture is passed through the portion of the membrane that will cover the bone. 4. The flap is then positioned coronally and sutured.