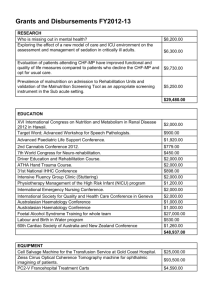
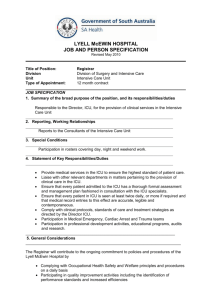
BHOPAL (M.P.) SUBJECT: - MEDICAL SURGICAL NURSING PROJECT WORK On INTENSIVE CARE UNIT SUBMITTED TO: SUBMITTED BY: Mrs. Jalpana Adhikar Professor hod of medical surgical nursing Ms. Veena Borkar M.Sc. Nursing Ist yr INTENSIVE CARE UNIT INTRODUCTION An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine. Intensive care units cater to patients with severe and life-threatening illnesses and injuries, which require constant, close monitoring and support from specialist equipment and medications in order to ensure normal bodily functions. They are staffed by highly trained doctors and nurses who specialize in caring for seriously ill patients. ICU's are also distinguished from normal hospital wards by a higher staff-to-patient ratio and access to advanced medical resources. Common conditions that are treated within ICUs include ARDS, trauma, multiple organ failure and sepsis DEFINITION An Intensive Care Unit (ICU) is a specially staffed and equipped, separate and selfcontained area of a hospital dedicated to the management of patients with lifethreatening illnesses, injuries and complications, and monitoring of potentially lifethreatening conditions. It provides special expertise and facilities for support of vital functions and uses the skills of medical, nursing and other personnel experienced in the management of these problems. In many units, ICU staff are required to provide services outside of the ICU such as emergency response (eg rapid response teams) and outreach services. Where applicable the hospital must provide adequate resources for these activities. CATEGORIES OF ORGAN SYSTEM MONITORING AND SUPPORT Advanced respiratory system monitoring / support is indicated by one of more of the following: Mechanical ventilatory support, excluding mask (CPAP) or non-invasive methods, e.g. mask ventilation • Extracorporeal respiratory support Basic respiratory system monitoring / support is indicated by one or more of the following: More than 50% oxygen by fixed performance mask The potential for deterioration to the point of needing advanced respiratory support Physiotherapy to clear secretions at least two hourly, whether via a trachesotomy, minitracheostomy, or in the absence of an artificial airway Patients recently extubated after a prolonged period of intubation and mechanical ventilation • Mask CPAP or non-invasive ventilation Patients who are intubated to protect the airway but needing no ventilatory support and who are otherwise stable. Circulatory system monitoring / support is indicated by one of more of the following: Vasoactive drugs to support arterial pressure or cardiac output Circulatory instability due to hypovolaemia from any cause Patients resuscitated after cardiac arrest where intensive care is considered clinically appropriate Intra aortic balloon pumping. Neurological system monitoring / support is indicated by one or more of the following: Central nervous system depression, from whatever cause, sufficient to prejudice the airway and protective reflexes Invasive neurological monitoring, e.g. ICP, jugular bulb sampling. Renal system monitoring / support is indicated by: Acute renal replacement therapy ( haemodialysis, haemofiltration etc.). GENERAL REQUIREMENTS FOR INTENSIVE CARE UNITS Depending upon the designated level, function, size, and case mix of the hospital and/ or region that it serves, an ICU may range from four to over 50 beds. Lager ICU should be divided into pods of 8-15 patients Staffing Medical staffing, including a director, with sufficient experience to provide for patient care, administration, teaching, research, audit, outreach…. Nursing staff: Australian College of Critical Care Nurses requires 1:1 for ventilated patients and 1:2 for lower acuity patients. Nurse in charge with post registration ICU qualification allied health and ancillary staff Medical staffing Director of the intensive care unit. The responsibility for the administrative and medical management of the unit is held by a physician, whose professional activities are devoted fulltime or at least 75% of the time to intensive care, who holds the position of director of the ICU. The head of the ICU has the sole administrative and medical responsibility for this unit and cannot hold top-level responsibilities in other departments or facilities of the hospital. The head of the ICU should be a senior accredited specialist in intensive care medicine as defined at country level, usually with a prior degree in anesthesiology, internal medicine, or surgery and have had a formal education, training, and experience in intensive care medicine as described by the ESICM guidelines Medical staff members. The head of the ICU is assisted by physicians qualified in intensive care medicine. The number of staff required will be calculated according to the number of beds in the unit, number of shifts per day, desired occupancy rate, extra manpower for holidays and illness, number of days each professional is working per week, and the level of care and as a function of clinical, research, and teaching workload. Extended work shifts have been shown to negatively impact the safety of patients as well as medical staff. The number of full time equivalent (FTE) physicians qualified in intensive care medicine per six to eight intensive care beds (at level of care II, see section ‘‘Activity Criteria’’) can be calculated (according to the European working hours directives) with the formula provided in paragraph 9 of the ESM . An experienced physician certified in intensive care medicine is on duty and available upon request at short notice in the hospital during ‘‘off duty hours.’’ The regular medical staff members of the ICU treat patients using state-ofthe-art techniques and may consult specialists in different medical, surgical, or diagnostic disciplines whenever necessary Nursing staff Organization and responsibilities. Intensive care medicine is the result of close cooperation among doctors, nurses, and allied health care professionals (AHCP). An efficient process of communication has to be organized between the medical and nursing staff of the ICU. Tasks and responsibilities have to be clearly defined. Head nurse. The nursing staff is managed by a dedicated, full-time head nurse, who is responsible for the functioning and quality of the nursing care. The head nurse should have extensive experience in intensive care nursing and should be supported by at least one deputy head nurse able to replace him (her). The head nurse should ensure the continuing education of the nursing staff. Head nurses and deputy head nurses should not normally be expected to participate in routine nursing activities. The head nurse works in collaboration with the medical director, and together they provide policies and protocols, and directives and support to the team. Allied health care personnel Physiotherapists. One physiotherapist with dedicated training and expertise in critically ill patients should be available per five beds for level III care on a 7 day/week basis. Technicians. Maintenance, calibration, and repair of technical equipment in the ICU must to be organized. This facility can be shared with other departments of the hospital but a 24-h availability has to be organized with priority for the ICU. Radiology technician. Should be on call around the clock. Interpretation of the medical imaging by the radiologist must be available at all times. Dietician. Should be on call during normal working hours. Speech and language therapist. Should be available to consult during normal working hours. Psychologist. Should be available to consult during normal working hours. Occupational therapist. Should be available to consult during normal working hours. Clinical pharmacist. Should be available to consult during normal working hours. A sufficient collaboration with pharmacy is of particular importance with respect to patient safety. Administrative personnel One medical secretary is required per 12 intensive care beds. Basic tasks are patient administration, external and internal communication exchange, and typing of reports and documents. One secretary per six beds may be desirable if she/he is also involved in arranging laboratory journals and medical files. Another approach is to calculate the number of medical secretarial assistants as one FTE per 500–700 admissions. Support for formal teaching activities may increase the need. Cleaning personnel A specialized group of cleaning personnel familiar with the ICU environment should be available for the ICU. They should be familiar with infection control, prevention protocols, and hazards of medical equipment. Cleaning and disinfection of the patient areas are performed under the nurse’s supervision. A checklist of the cleaning status must be kept. Regular updates should be provided to ensure cleaning protocols reflect best practice. Operational Documented educational programme agreed policies team approach surge capacity for emergencies documented procedures for audit peer review quality assurance Site separate unit appropriate access to ED, theatre, radiology Design Patient cubicles (> 20 m2), wash basin, service outlets, appropriate electrical standards, privacy Work areas, equipment and storage areas, staff facilities, seminar room, offices, relatives area Equipment: appropriate equipment and regular system for checking safety Monitoring equipment: for each patient, for unit (.eg. gas supply alarms), and for patient transport Criteria for a level I, II and III ICU and a PICU LEVELS OF INTENSIVE CARE UNITS LEVEL 1 should be capable of providing immediate resuscitation and short-term cardiorespiratory support for critically ill patients will also have a major role in monitoring and prevention of complications in “at risk” medical and surgical patients must be capable of providing mechanical ventilation and simple invasive cardiovascular monitoring for a period of at least several hours LEVEL II should be capable of providing a high standard of general intensive care, including complex multi-system life support, which supports the hospital’s delineated responsibilities minimum of 6 beds LEVEL III a tertiary referral unit for intensive care patients should be capable of providing comprehensive critical care including complex multisystem life support for an indefinite period should have a demonstrated commitment to academic education and research All patients admitted to the unit must be referred for management to the attending intensive care specialist all consultants are FCICMs may have over 50 beds, should include pods of 8-15 beds ORGANIZATION OF INTENSIVE CARE UNIT LOCATION Should be a geographically distinct area within the hospital, with controlled access. No through traffic to other departments should occur. Supply and professional traffic should be separated from public/visitor traffic. Location should be chosen so that the unit is adjacent to, or within direct elevator travel to and from, the Emergency Department, Operating Room, Intermediate care units, and the Radiology Department. Design of ICU There should be a single entry and exit. ICU must have areas and rooms for public reception, patient management and support services. Full commitment must be given from administration and a designated team to work on various tasks. There should be sufficient number of lifts available to carry these critically ill patients to different areas. The total design of the ICU must take into account the following areas; • P= Patient care • N= Nursing • E= Eating (clean area for food preparation and delivery) • U= Unclean (dirty linen, equipment) • M= Medication storage (drugs, I V fluids) • A= Administration (clerking, stationary) • T= Teaching • I= Infection elimination (sterilizing area) • C= Clean area (fresh linen, equipment) • S= Storage (back up equipment) • V= Visitors BED STRENGTH The number of ICU beds in a hospital ranges from 1 to 10 per 100 total hospital beds. Multidisciplinary requires more beds than single speciality. ICUs with fewer than 4 beds are not cost effective and over 20 beds are unmanageable. IDEALLY 8 TO 12 BEDS 1 ISOLATION BED FOR EVERY 10 ICU BEDS BED SPACE & BEDS 150 – 200 SQUARE FEET PER OPEN BED WITH 8 FEET IN BETWEEN BEDS. 225 – 250 SQUARE FEET PER BED IF IN A SINGLE ROOM. BEDS - ADJUSTABLE, NO HEAD BOARD, SIDE RAILS AND WITH WHEELS. Patient areas Single rooms are essential for isolation and privacy. The ratio of single room beds to open ward beds depends on the role and type of ICU. A central station will have the central monitor, drug cupboard, telephone, refrigerator and patient records. Nursing in ICU is always at the bedside. Sufficient hand wash areas should be provided. X-ray views are needed in multi-bed wards. Proper facilities for haemodialysis such as filtered water should be incorporated at the time of ICU planning. INFRASTRUCTURE Patients must be situated so that direct or indirect (e.g. by video monitor) visualization by healthcare providers is possible at all times. The preferred design is to allow a direct line of vision between the patient and the central nursing station. Modular design – sliding glass doors & partitions to facilitate visibility. ENVIRONMENT Signals & alarms – add to the sensory overload; need to be modulated. Floor coverings and ceiling with sound absorption properties. Doorways – offset to minimise sound transmission. light & soft music (except 10 pm to 6 am). Lighting – focussed & central lighting. Airconditioning (split / central) : 25 + or – 2 degrees centigrade. Cleaning – vacuum cleaning & wet mopping of the floor. fumigation is no longer recommended. Natural illumination and view - windows are an important aspect of sensory orientation; helps to reinforce day/night orientation. Window treatments should be durable and easy to clean, and a schedule for their cleaning must be established. Additional approaches to improving sensory orientation for patients may include the provision of a clock, calendar, bulletin board, and/or pillow speaker connected to radio and television ACCESSORIES 3 oxygen outlets, 3 suction outlets (gastric, tracheal & underwater seal), two compressed air outlets and 16 power outlets per bed. storage by each bedside (built in / alcove). hand rinse solution by each bedside. equipment shelf at the head end (mind the height of the care giver). hooks & devices to hang infusions / blood bags – suspended from the ceiling with a sliding rail to position. infusion pumps to be mounted on stands / poles. UTILITIES electrical – adequate sockets (5amps & 15 amps), generator supply & battery back up. medical gas & vacuum pipeline – colour coded and not interchangeable. water from a certified source especially if used for haemodialysis handwashing areas – uninterrupted water supply, disposable paper towels / hand drier. (no cloth towels please) telephones & computers for communication. sterilising area – large water boiler / geyser & exhaust fans. clean and a dirty utility with no interconnection. shelving & cabinets off the ground for storage. waste & sharps disposal work areas and storage for critical supplies should be located immediately adjacent to each icu. alcoves should provide for the storage and rapid retrieval of crash carts and portable monitor/defibrillators. there should be a separate medication area of at least 50 square feet containing a refrigerator for pharmaceuticals, a double locking safe for controlled substances, and a table top for preparation of drugs and infusions. EQUIPMENT 1. 2. 3. 4. 5. Monitoring Equipment Therapeutic Equipment Digital & Analogue Display Audio & Visual Alarms Battery Back Up & Charging Common equipment in an ICU includes: mechanical ventilator to assist breathing through an endotracheal tube or a tracheotomy opening; cardiac monitors including telemetry, external pacemakers, and defibrillators; dialysis equipment for renal problems; equipment for the constant monitoring of bodily functions; a web of intravenous lines, feeding tubes, nasogastric tubes, suction pumps, drains and catheters; a wide array of drugs to treat the main condition(s). Monitoring • Bed side and central monitors, 12 lead ECG recorders, intravascular and intracranial pressure monitoring devices • Cardiac output computer • Pulseoxymeter • Pulmonary function monitoring devices • Expired CO2 analyzers • EEG monitors • Patient/ bed weighers • Enzymatic blood glucose meters Radiology • X ray viewers • Portable x ray machine • Image intensifiers Respiratory therapy • Ventilators, bedside &portable • Humidifiers, oxygen therapy devices &airway circuits • Intubation trolley • Manual self inflating resuscitators • Fibre-optic bronchoscope • Anaesthetic machine Cardiovascular therapy • Cardiopulmonary resuscitation trolleys • Defibrillators • Temporary transvenous pacemaker • Intra-aortic balloon pump • Infusion pumps and syringes Dialytic therapy • Haemodialysis machine • Peritoneal dialysis equipment • Continuous arterio venous hemofiltration setts Laboratory • Blood gas analyzer • Selective ion electrode analyzers • Osmometer • Hematocrit centrifuge • microscope Hardware • Dressing trolleys • Drip stands • Bed restraints • Heating/ cooling blankets • Pressure distribution mattresses • Sterilizing equipments STORAGE AREAS/SERVICE AREAS Most ICUs lack storage space. They should have a total of 25-30% of all patient and central station areas for storage. Clean and dirty utility rooms should be separate each with its own access. Disposal of soiled linen and waste must be catered for. A lab, which estimates blood gases, electrolytes, haemoglobin, is a must. Good communication systems, staff lounge, food areas must be marked out. There should be an area to teach and train students. References 1. Ferdinande P (1997) Recommendations on minimal requirements for intensive care departments. Members of the Task Force of the European Society of Intensive Care Medicine. Intensive Care Med 23:226–232 2. Brilli RJ, Spevetz A, Branson RD, Campbell GM, Cohen H, Dasta JF, Harvey MA, Kelley MA, Kelly KM, Rudis MI, St Andre AC, Stone JR, Teres D, Weled BJ (2001) Critical care delivery in the intensive care unit: defining clinical roles and the best practice model. Crit Care Med 29:2007–2019 3. Morales IJ, Peters SG, Afessa B (2003) Hospital mortality rate and length of stay in patients admitted at night to the intensive care unit. Crit Care Med 31:858–86