Frankfurt Plane in VP Shunt: Gravitational Unit Implantation
advertisement

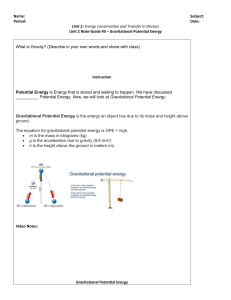
Acta Neurochir (2014) 156:1351–1356 DOI 10.1007/s00701-014-2076-y CLINICAL ARTICLE - PEDIATRICS The Frankfurt horizontal plane as a reference for the implantation of gravitational units: a series of 376 adult patients Florian Baptist Freimann & Marie-Luise Luhdo & Veit Rohde & Peter Vajkoczy & Stefan Wolf & Christian Sprung Received: 15 January 2014 / Accepted: 19 March 2014 / Published online: 4 May 2014 # Springer-Verlag Wien 2014 Abstract Background The in-line combination of adjustable differential pressure valves with fixed gravitational units is increasingly recommended in the literature. The spatial positioning of the gravitational unit is thereby decisive for the valve opening pressure. We aimed at providing data on factors contributing to primary overdrainage and underdrainage of cerebrospinal fluid (CSF), with special attention paid to the implantation angle of the gravitational unit. Methods Weretrospectively analyzed the postoperative course of 376 consecutive patients who received a ventriculoperitoneal shunt with a proGAV valve. The incidence of both primary CSF overdrainage and underdrainage was correlated with the implantation angle of the gravitational unit in regard to the Frankfurt horizontal plane and the patients’ general parameters. Results Primary overdrainage was found in 41 (10.9 %) patients. Primary underdrainage was found in 113 (30.1 %) patients. A mean deviation of 10° (±7.8) for the gravitational unit in regard to the vertical line to the Frankfurt horizontal plane was found. In 95 % of the cases the deviation was less than 25°. No significant correlation between the implantation angle and the incidence of overdrainage or underdrainage of CSF was found. The patients’ age and having single hydrocephalus entities were identified as factors significantly predisposing patients to overdrainage or underdrainage. F. B. Freimann (*) : V. Rohde Department of Neurosurgery, Universitätsmedizin Göttingen, Georg-August-Universität Göttingen, Germany, 37099 Göttingen, Germany e-mail: florian.freimann@med.uni-goettingen.de F. B. Freimann : M.<L. Luhdo : P. Vajkoczy : S. Wolf : C. Sprung Department of Neurosurgery, Charité - Universitätsmedizin Berlin, Germany, Berlin, Germany Conclusion The implantation of the gravitational unit of the proGAV valve within a range of at least 10° in regard to the vertical line to the Frankfurt horizontal plane does not seem to predispose patients to primary overdrainage or underdrainage in ventriculoperitoneal shunting. The plane may serve as a useful reference for the surgeon’s orientation. Keywords Frankfurt horizontal plane . Gravitational unit . Hydrocephalus . Ventriculoperitoneal shunt Introduction Ventriculoperitoneal shunting is accompanied by risks such as surgical complications, shunt infections, or dislocations of the ventricular or peritoneal catheter. Those hazards are not related to the shunt valve. Another non-valve-related shunt malfunction is the underdrainage of cerebrospinal fluid (CSF) due to mechanical obstacles like kinking of the catheter, catheter occlusion, or abdominal pseudocysts [3, 4]. In contrast, an unsatisfying clinical result after shunt implantation without an obstruction of the catheter may represent a functional underdrainage of CSF [18]. The functional underdrainage and the overdrainage of CSF are valve-related issues. The overdrainage of CSF may lead to orthostatic headache, slitlike ventricles, or subdural effusions. A surgical revision with a ligation of the shunt, a change of the valve, or the surgical decompression of subdural hematoma may be necessary. However, the flow resistance within the shunt system is mainly controlled by the opening pressure of the valve. Both CSF overdrainage and functional underdrainage can be treated to a certain extent by valve adjustments. This was demonstrated especially for modern adjustable and gravity-assisted valves such as the proGAV valve (Miethke, Potsdam, Germany), which consists of an adjustable differential pressure (DP) 1352 valve and a gravitational unit with a fixed opening pressure [6, 7, 9, 11, 12, 20]. It has been stated that the gravitational unit of the proGAV valve is mainly responsible for those beneficial effects. This device consists of a cylindrical titanium housing in which a tantalum ball blocks the CSF flow through the device gradually via a position-dependent mechanism [1]. The implantation angle of the gravitational unit is therefore important for the amount of CSF drainage. Ideally it should be in a vertical position when the patient is standing upright and in a horizontal position when the patient is lying flat [19]. If the gravitational unit position is suboptimal, in theory, overdrainage or underdrainage of CSF may occur. A deviation from the vertical body axis of <10° was suggested as acceptable [21]. However, the question of to what degree the implantation angle of gravitational units is of clinical relevance has not yet been answered entirely. Furthermore, an ideal reference plane for the implantation of gravitational units is, to our knowledge, not defined in the literature. The Frankfurt horizontal plane (FHP) is defined as a plane passing through the inferior margin of the orbit and the upper margin of the external auditory meatus. It is described as a plane that is the nearest match to the gravity horizontal line (GHL) [2, 14]. We hypothesize that the FHP is useful to serve as a reference for the surgeon to identify the optimal angle for implantation of the gravitational unit. The purpose of the current study was to investigate the factors contributing to primary CSF overdrainage and underdrainage with special attention to the spatial relationship of the gravitational unit to the FHP. Patients & methods Study group We retrospectively analyzed the postoperative course of 376 consecutive adult patients treated for different entities of hydrocephalus between February 2004 and December 2011. All patients received a ventriculoperitoneal shunt with a proGAV valve. The patients’ general parameters such as age, gender, body weight, body height, and mobility were evaluated. The implantation site of the gravitational unit and perioperative complications were included in this analysis. The various hydrocephalus entities were defined as primary normal pressure hydrocephalus (pNPH), secondary NPH with a history of more than 3 months between causative event and development of hydrocephalus (sNPH), malresorptive hydrocephalus (MH), hypertensive hydrocephalus (HH), pseudotumor cerebri (PC), and congenital hydrocephalus (CH) with shunt dependency since early childhood. The latter patients received the proGAV valve at an adult age in a revision surgery. Acta Neurochir (2014) 156:1351–1356 Overdrainage and underdrainage The initial setting of the valve opening pressure and all documented first valve adjustments were analyzed. An unsatisfying clinical result with no significant reduction of the ventricular size in postoperative imaging and no evidence of a mechanical obstruction in the shunt system resulted in an initial decrease of the valve opening pressure and was considered to be a primary functional underdrainage. If signs and symptoms like orthostatic headaches and slit-like ventricles, subdural hygroma, or hematoma were detected in cranial imaging, an increase of the valve opening pressure was carried out, and a primary overdrainage of CSF was assumed. Valve implantation angle The FHP and the gravitational unit (SA) were identified on the lateral scout view of computed tomography (CT) scans conducted subsequent to the implantation of the new shunt system in all cases. A line was drawn vertical to the FHP (VL), and another line along the implantation axis of the gravitational unit. The angle between VL and the axis of the gravitational unit was measured. A deviation of the gravitational unit from VL in the anterior direction above the FHP was defined as an inclination of the gravitational unit. A deviation in the posterior direction above the FHP was defined as a reclination of the gravitational unit (Figure 1). Statistical analysis All statistical analysis was performed using the statistical environment R 3.0.1 (R Software Foundation, Vienna, Austria, www.r-project.org). Summary data is presented as mean and standard deviation, or median (25 %/75 % quartile), whichever is appropriate. Univariate comparisons were performed with the Wilcoxon test. Multivariate assessment was modeled with generalized linear models, with all demographic factors being initially included. To achieve the most parsimonious model, a step-down approach was used and the least significant term excluded until only factors significant at p<0.05 remained in the final model. Results General parameters We included 200 female (53.2 %) and 176 male (46.8 %) consecutive patients in our analysis. All patients received a ventriculoperitoneal shunt for different hydrocephalus entities (99 pNPH, 57 sNPH, 133 MH, 37 HH, 16 PC, and 27 CH) with a retroauricularly implanted proGAV valve. The opening pressure of the gravitational unit was +20 cm H2O in the vast Acta Neurochir (2014) 156:1351–1356 1353 Fig. 1 Lateral scout view of the postoperative CT imaging of three different patients with (a) reclined, (b) vertical, and (c) inclined implantation angles of the gravitational unit (SA) in relation to the vertical line (VL) to the Frankfurt horizontal plane (FHP) majority of cases. The mean age at shunt implantation was 55.6 (±18.2) years. The mean body weight was 75 (±16) kg, while the body height was 170 (±11) cm. We considered 304 (80.9 %) patients of the study population to be “mobile”, while 72 (19.1 %) patients were “bedridden” due to various neurological disorders. The median follow-up period of the analysis was 20 (15/30 quartile) months (Table 1). Surgical revisions A total of 61 shunt revisions were carried out during the study period. In 48 cases (12.8 %), revision surgery was indicated due to non-valve-related reasons. We observed 14 shunt infections with explantation of the shunt (3.7 %), 10 superficial wound infections (2.7 %), 7 revisions of the ventricular catheter (1.9 %), 12 revisions of the abdominal catheter (3.2 %), 2 mechanical obstructions of the catheter (0.5 %), and 2 secondary disconnections (0.5 %). An injury of the intestines occurred during the placement of the abdominal catheter in one case (0.3 %). In 13 cases (3.5 %), revision surgery was indicated for valve-related reasons. A functional underdrainage led in 12 cases (3.2 %) after a stepwise downregulation of the opening pressure to 0 cm H2O to the assumption of presence of a dysfunction and surgical revision of the valve. In six of these cases (1.6 %), the gravitational unit was removed. One patient suffering from MH after posttraumatic bilateral cranial decompression developed a subdural hematoma subsequent to the shunt implantation and reimplantation of a bone flap in a combined procedure. The hematoma was evacuated and the shunt was ligated transiently. Overdrainage and underdrainage The opening pressure of the DP unit of the proGAV valve was set to a median of 5 (5/5 quartile) cm H2O at the time of implantation. Valve adjustments were carried out in 154 patients (41 %). A primary upregulation of the valve opening pressure was carried out in 41 of the cases (10.9 %) for the treatment of conditions related to CSF overdrainage. These conditions were orthostatic headache in 7 cases (1.9 %), slitlike ventricles in 18 cases (4.8 %), subdural hygroma in 13 cases (3.5 %), and subdural hematoma in 3 cases (0.8 %). All overdrainage-related events could be sufficiently treated by valve adjustments (excluding the case mentioned above). A primary downregulation of the valve opening pressure for the treatment of a functional underdrainage of CSF was carried out in 113 of the cases (30.1 %). We found a significant correlation between patient age and CSF overdrainage and underdrainage in our series. Patients suffering from primary overdrainage of CSF had a mean age of 47.1 (±18.3) years (p<0.01). In contrast, patients having signs and symptoms which were considered as a primary underdrainage had a mean age of 59.4 (±17.8) years (p<0.001) (Table 1). The incidence of CSF underdrainage was found to increase with age (0.4 % increase per age year) (p=0.05). No significant correlation of patient gender, body height, body weight, mobility, and the initial valve setting with the occurrence of overdrainage or functional underdrainage was found in a univariate analysis (Table 1). Multivariate analysis revealed that underdrainage was significantly less common in mobile patients (p<0.01) and more likely with higher initial valve settings (4 % increase per cm H2O) (p=0.001). Hydrocephalus entities were found to play a significant role in valve-related complications. Only five atients with pNPH were treated for overdrainage (p<0.05), while in 50 (of 99) cases a primary downregulation of the valve opening pressure for the treatment of a functional underdrainage was carried out (p<0.001). No gender-specific preponderance for this observation was found. The mean age in this subpopulation was 70.7 (±9) years; the median initial opening pressure of the DP valve was 5 (5/5 quartile) cm H2O (Table 1). Patients with MH had significantly fewer signs and symptoms of overdrainage than the remaining study population did (26 patients out of 133)(p<0.001). The mean age in the MH sub-population was 54 (±14.7) years; the median initial opening pressure of the DP valve was 5 (5/5 quartile) 1354 Acta Neurochir (2014) 156:1351–1356 Table 1 Patients’ general parameters, mobility, and hydrocephalus entities in regard to the primary overdrainage and underdrainage of CSF. Level of significance *=p<0.05, **=p<0.01, ***=p<0.001 compared to the study group Age (mean years ± SD) Gender Female Male Body height (mean cm ± SD) Body weight (mean kg ± SD) Mobility Mobile Bedridden Primary valve setting (median and 25 %/75 % quartile) Hydrocephalus entities Primary NPH Secondary NPH Malresorptive Hypertensive Pseudotumor Congenital All patients Primary overdrainage Primary underdrainage 55.6 (±18.2) 47.1 (±18.3)** 59.4 (±17.8)** 200 176 26 15 63 50 170 (±11) 75 (±16) 167 (±16) 71 (±12) 171 (±13) 73 (±13) 304 72 5 (5/5) 32 9 5 (5/5) 90** 23 5 (5/5) 99 57 133 37 16 27 5* 8 13 6 1 8** 50*** 15 26*** 8 3 9 cm H2O (Table 1). In contrast, the patients with CH who received the proGAV valve in a revision surgery had a significantly higher risk for overdrainage-related events and corresponding valve adjustments (8 patients out of 27)(p<0.01). The mean age in this sub-population was 27.4 (±7.2) ye;rs, the median initial opening pressure of the DP valve was 5 (5/6 quartile) cm H2O (Table 1). Valve implantation angle A deviation of the implantation angle of the SA in relation to the VL was measured in 360 patients of the whole study group (95.7 %)(Fig. 1). The absolute mean deviation from the VL was 10° (±7.8). 95 % of the patients had a deviation of less than 25°. No correlation was found between the implantation angle in relation to the VL of the FHP and the occurrence of overdrainage or underdrainage (all p >0.4) (Table 1). A reclination of the gravitational unit was found in 185 cases, with a mean deviation of 9.7° (±7.7); while an inclination was found in 175 cases, with a mean deviation of 10.3° (±8). Neither the reclination nor the inclination of the gravitational unit in relation to the VL was observed to predispose significantly for overdrainage or underdrainage of CSF (all p>0.3) (Table 2). No effect of the hydrocephalus entity, the mobility of the patients, or other parameters on the significance of the implantation angle for the overdrainage or underdrainage of CSF was found in our study group. Furthermore, no threshold value for the deviation from the VL of the FHP could be determined to predispose for overdrainage or underdrainage. Discussion The augmentation of adjustable DP valves with antisiphoning devices (ASD) is advocated in the literature. Beneficial effects for the prevention and the treatment of overdrainage and functional underdrainage in patients with a ventriculoperitoneal shunt have been reported, especially for the use of gravitational valves [6, 7, 12]. The opening pressure of gravitational units depends on their spatial positioning. A suboptimal placement of the gravitational unit might therefore predispose patients, along with other factors such as patients’ age, gender, body weight, body height, hydrocephalus entity, and the initial setting of the DP valve opening pressure, for overdrainage or underdrainage of CSF. Park et al. [16] described this phenomenon in a retrospective series of 24 adult patients shunted with a gravitational valve with a fixed opening pressure (GAV) (Miethke, Potsdam, Germany). They found a positive correlation of the valve inclination relative to the patients’ vertical position with the extent of ventricular volume changes after shunting. It seems notable that the radiographic images for this analysis were taken in the patient standing position. An inclination of more than 20° to a patient’s vertical position was described as a predisposition to functional underdrainage in the sub-group of non-ambulatory patients [16]. Deininger and Weyerbrock [5] and Kaestner et al. [8] also emphasized the relevance of the spatial positioning of gravitational units, especially for bedridden patients in smaller retrospective series [5, 8]. But to what extent is the implantation angle of the gravitational unit relevant for the clinical course of patients with a Acta Neurochir (2014) 156:1351–1356 Table 2 The deviation angles of the gravitational units from VL in regard to the primary overdrainage and underdrainage of CSF 1355 Deviation from VL of FHP (mean ± SD) Number of inclination Degree of inclination (mean ± SD) Number of reclination Degree of reclination (mean ± SD) ventriculoperitoneal shunt? We aimed at providing data on that question by retrospectively analyzing a series of 376 consecutive adult patients who received a proGAV valve (Miethke, Potsdam, Germany), which consists of an adjustable DP unit and a gravitational unit with a fixed opening pressure, for the treatment of various hydrocephalus entities. The spatial positioning of the gravitational units of the proGAV was evaluated on lateral scout CT images obtained from the patients while in a horizontal body position. A deviation from the vertical axis in the lateral direction is not detectable on two-dimensional lateral plane images; this is a limitation of our retrospective study design. However, a relevant deviation of the implantation angle from the VL is only possible in the anterior-posterior direction due to the skull shape. A deviation in the anterior-posterior direction requires a reference plane, which represents the gravity horizontal line (GHL), as is, in fact, the case for the intraoperative situation when the gravitational unit is implanted. The vertical axis to the FHP (VL) was used for the anterior-posterior direction as the reference for the implantation angle of gravitational units in regard to the patient’s vertical axis. The FHP is defined as a plane between the inferior margin of the orbit and the upper margin of the ipsilateral external auditory meatus. It was historically introduced in 1884 at the World Congress on Anthropology in Frankfurt am Main, Germany, and is nowadays still accepted as a plane that nearly matches the gravity horizontal line (GHL) [10, 13]. Nevertheless, some authors challenge the congruence of the FHP with the GHL, and a mean deviation of the FHP from the GHL of approximately 5° has been reported [14, 17]. The state of CSF overdrainage or underdrainage was evaluated by analyzing the initial DP shunt opening pressure, the first valve adjustments, and the corresponding clinical and radiological findings after shunt implantation. All subsequent valve adjustments were not included in this analysis. We regard those following adjustments as being mainly the result of the preceding adjustment. A clear relationship to the implantation angle of the gravitational unit or other independent factors contributing to CSF overdrainage or underdrainage cannot be abstracted from those actions. We observed a correlation between patient age and overdrainage and underdrainage. Patients of younger age had thereby a significantly higher risk for signs and symptoms All patients Primary overdrainage Primary underdrainage 10 (±7.8) 175 10.3 (±8) 185 9.7 (±7.7) 10 (±7.5) 22 10.8 (±7) 19 9.1 (±8.2) 10.4 (±6.9) 54 11.2 (±6.4) 58 9.6 (±7.2) indicating ovedrainage, while older patients had significantly more frequent valve adjustments for the treatment of a functional underdrainage. Furthermore, patients suffering from a hydrocephalus entity typical for those of younger age had a significantly higher risk for overdrainage-related events. We interpret this finding to reflect an assumedly higher grade of activity and mobility in younger patients. This is in agreement with our finding that underdrainage is less common in mobile patients. In contrast, patients suffering from hydrocephalus entities typical for advanced age were found to have a functional CSF underdrainage significantly more often. The phenomenon of a stepwise downregulation of the valve opening pressure was described in particular during the long-term treatment of pNPH [7]. The recently published data from a prospective and multicentric trial on "Shunt Valves plus shunt Assistant versus Shunt valves alone for controlling Overdrainage in idiopathic Normal pressure hydrocephalus in Adults" (SVASONA) indicate inter alia an association of female sex with a higher risk of clinical signs and symptoms suggestive of overdrainage [12, 15]. We also expected to find correlations between gender and other parameters, such as body height and body weight, and the overdrainage or underdrainage. The reason why no such correlation was found remains speculative, but we assume that these parameters were overrated compared to other less obviously influential variables within our large and inhomogeneous study group. We did not observe a significant correlation of the implantation angle of the gravitational unit in regard to the VL of the FHP. The heterogeneity of our study group and small numbers of patients of single hydrocephalus types might have masked an effect of the implantation angle in this particular subgroup. We hypothesize that the habitual head position and the need for CSF drainage varies between individuals and during daily activity. Furthermore, a deviation of the FHP from the GHL was reported in the literature. These factors may have eliminated possible effects resulting from different implantation angles in regard to the FHP on CSF overdrainage and underdrainage. We found a mean deviation from the VL of 10°; in 95 % of the patients the deviation was less than 25°. We therefore conclude that an implantation of the gravitational unit of the proGAV within this range is safe, as it was suggested previously [21]. Nevertheless a more precise 1356 orientation of the spatial positioning of gravitational units still has to be sought after. The FHP appears as a useful reference plane for the implantation of gravitational shunt valves. Conclusion The retroauricular implantation of the gravitational unit of the proGAV within a range of at least 10° deviation from the VL in reference to the FHP may not predispose for CSF overdrainage or underdrainage. The FHP may serve as a useful reference for the surgeon’s orientation. Conflicts of interest FBF, MLL, VR, PV, and SW have no conflicts of interest to disclose. CS is supported by Aesculap AG to deliver presentations at scientific meetings but has no financial interest in the product this article discusses. References 1. Allin DM, Czosnyka ZH, Czosnyka M, Richards HK, Pickard JD (2006) In vitro hydrodynamic properties of the Miethke proGAV hydrocephalus shunt. Cerebrospinal Fluid Res 3:9 2. Barbera AL, Sampson WJ, Townsend GC (2009) An evaluation of head position and craniofacial reference line variation. Homo 60(1): 1–28 3. Browd SR, Gottfried ON, Ragel BT, Kestle JRW (2006) Failure of cerebrospinal fluid shunts: part II: overdrainage, loculation, and abdominal complications. Pediatr Neurol 34(3):171–176 4. Browd SR, Ragel BT, Gottfried ON, Kestle JRW (2006) Failure of cerebrospinal fluid shunts: part I: Obstruction and mechanical failure. Pediatr Neurol 34(2):83–92 5. Deininger MH, Weyerbrock A (2009) Gravitational valves in supine patients with ventriculo-peritoneal shunts. Acta Neurochir (Wien) 151(6):705–709, discussion 709 6. Freimann FB, Sprung C (2012) Shunting with gravitational valvescan adjustments end the era of revisions for overdrainage-related events? J Neurosurg. doi: 10.3171/2012.8.JNS1233 7. Freimann FB, Vajkoczy P, Sprung C (2013) Patients benefit from low-pressure settings enabled by gravitational valves in normal pressure hydrocephalus. Clin Neurol Neurosurg. doi: 10.1016/j.clineuro. 2013.06.010 Acta Neurochir (2014) 156:1351–1356 8. Kaestner S, Kruschat T, Nitzsche N, Deinsberger W (2009) Gravitational shunt units may cause under-drainage in bedridden patients. Acta Neurochir (Wien) 151(3):217–221, discussion 221 9. Kiefer M, Eymann R, Meier U (2002) Five years experience with gravitational shunts in chronic hydrocephalus of adults. Acta Neurochir (Wien) 144(8):755–767, discussion 767 10. Leitão P, Nanda RS (2000) Relationship of natural head position to craniofacial morphology. Am J Orthod Dentofac Orthop 117(4):406– 417 11. Lemcke J, Meier U (2010) Improved outcome in shunted iNPH with a combination of a Codman Hakim programmable valve and an Aesculap-Miethke ShuntAssistant. Cent Eur Neurosurg 71(3):113–116 12. Lemcke J, Meier U, Müller C, Fritsch MJ, Kehler U, Langer N, Kiefer M, Eymann R, Schuhmann MU, Speil A, Weber F, Remenez V, Rohde V, Ludwig HC, Stengel D (2013) Safety and efficacy of gravitational shunt valves in patients with idiopathic normal pressure hydrocephalus: a pragmatic, randomised, open label, multicentre trial (SVASONA). J Neurol Neurosurg Psychiatr 84(8): 850–857 13. Lundström A, Lundström F (1995) The Frankfort horizontal as a basis for cephalometric analysis. Am J Orthod Dentofac Orthop 107(5):537–540 14. Madsen DP, Sampson WJ, Townsend GC (2008) Craniofacial reference plane variation and natural head position. Eur J Orthod 30(5): 532–540 15. Meier U, Stengel D, Müller C, Fritsch MJ, Kehler U, Langer N, Kiefer M, Eymann R, Schuhmann MU, Speil A, Weber F, Remenez V, Rohde V, Ludwig HC, Lemcke J (2013) Predictors of subsequent overdrainage and clinical outcomes after ventriculoperitoneal shunting for idiopathic normal pressure hydrocephalus. Neurosurgery 73(6):1054–1060 16. Park J, Kim G-J, Hwang S-K (2007) Valve inclination influences the performance of gravity-assisted valve. Surg Neurol 68(1):14–18, discussion 18 17. Petricevic N, Celebic A, Celic R, Baucic-Bozic M (2006) Natural head position and inclination of craniofacial planes. Int J Prosthodont 19(3):279–280 18. Sprung C, Miethke C, Schlosser H-G, Brock M (2005) The enigma of underdrainage in shunting with hydrostatic valves and possible solutions. Acta Neurochir Suppl 95:229–235 19. Stockhammer F, Miethke C, Knitter T, Rohde V, Sprung C (2013) Flow-related noise in patients with ventriculoperitoneal shunt using gravitational adjustable valves. Acta Neurochir (Wien). doi: 10.1007/ s00701-013-1876-9 20. Toma AK, Tarnaris A, Kitchen ND, Watkins LD (2011) Use of proGAV® shunt valve in normal pressure hydrocephalus. Neurosurgery. doi: 10.1227/NEU.0b013e318214a809 21. Vienenkötter B, Unterberg A, Aschoff A (2009) Implantation failures and suboptimal positions of gravitational valves - with massive impacts on shunt dysfunction. Cerebrospinal Fluid Res 6(Suppl 2):20